Abstract
Background
The impact of various clinical variables on long-term survival of patients with acutely decompensated diastolic heart failure (DHF) compared to systolic heart failure (SHF) has not been sufficiently investigated.
Methods
Clinical, laboratory, electrocardiographic and echocardiographic data were collected and analyzed for all-cause mortality in 473 furosemide-treated patients aged ≥60 years, hospitalized for acutely decompensated HF.
Results
Diastolic heart failure patients (n = 183) were more likely to be older, female, hypertensive, obese, with shorter preexisting HF duration, atrial fibrillation, lower New York Heart Association (NYHA) class, lower maintenance furosemide dosages, and to receive calcium antagonists. The SHF group (290 patients) demonstrated prevailing coronary artery disease, nitrate or digoxin treatment, and electrocardiographic conduction disturbances (P ≤ 0.01 in all comparisons). On median 35-month follow-up, the respective one-, three- and five-year survival rates were 82%, 48% and 33% in DHF versus 74%, 46% and 30% in SHF (P = 0.3). Higher furosemide daily dosage at discharge (OR = 1.24, 95% CI = 1.11–1.37, P < 0.001), increasing age (OR = 1.29, 95% CI = 1.09–1.54, P = 0.003), peripheral arterial disease (OR = 1.47, 95% CI = 1.02–2.13, P = 0.043), and a history of stroke (OR = 1.44, 95% CI = 0.98–2.1, P = 0.066) were most significantly associated with shorter survival in SHF. DHF, in turn, demonstrated higher NYHA class (OR = 2.52, 95% CI = 1.48–4.29, P < 0.001), history of non-advanced malignancy (OR = 2.51, 95% CI = 1.3–4.85, P = 0.012), and atrial fibrillation (OR = 1.6, 95% CI = 0.97–2.64, P = 0.066). Antilipid treatment (OR = 0.56, 95% CI = 0.3–1.02, P = 0.049) predicted better survival.
Conclusion
In-patients with acutely decompensated DHF differ from similar SHF subjects with respect to prognostic significance of a number of clinical variables. This observation might carry practical implications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diastolic heart failure (DHF) is a clinical syndrome manifested by symptoms and signs of heart failure (HF), accompanied by normal left ventricular ejection fraction (LVEF) and diastolic dysfunction [3, 7, 26, 32, 34]. LVEF remains preserved in as many as 24% to 55% of HF cases [4, 5, 10, 15, 17, 19, 22, 23, 25, 27–29, 31, 33], and with time the percentage progressively increases [25]. Clinical profile of DHF patients substantially differs from those with systolic HF (SHF). Thus, DHF patients are more likely to be older, of female sex, hypertensive, obese, suffering from chronic obstructive pulmonary disease (COPD), atrial fibrillation or receiving calcium antagonists, compared to subjects with SHF [4, 5, 10, 15, 17, 19, 22, 23, 25, 27–29, 31, 33]. Nevertheless, clinical manifestations of HF are ameliorated in DHF patients compared to those with SHF [5, 17, 31]. DHF patients are less likely to demonstrate coronary artery disease (CAD), left bundle branch block on electrocardiogram (ECG), as well as to receive angiotensin-converting enzyme inhibitors or digoxin [4, 5, 10, 15, 17, 19, 22, 23, 25, 27–29, 31, 33].
DHF is frequently associated with survival rates either better [15, 17, 22, 25, 27–29, 33] or similar [4, 5, 31] to those observed in SHF. Over recent decades, the survival rates were shown to improve in a majority of HF patients, except those with preserved LVEF [25]. However, the regimen of optimal management for DHF patients is still questionable [3, 7]. Information available on the impact of various clinical variables on the long-term survival in the context of DHF versus SHF is scarce [4, 25]. Part of the predictors of death among patients with reduced or preserved LVEF was found to be the same in a number of studies [4, 25]. These predictors included age, renal dysfunction, diabetes mellitus, anemia, peripheral arterial disease, dementia, and hyponatremia [4, 25]. However, while male gender predicted higher mortality rate in patients with preserved LVEF, this was not true for patients with SHF [25]. Furthermore, CAD was found to be associated with high mortality only in patients with reduced LVEF [25]. It is conceivable that the list is still incomplete, and additional clinical variables, not yet evaluated, might also be associated with higher mortality in DHF.
In particular, no sufficient information is available thus far regarding predictors of long-term mortality in furosemide-treated patients, who have been hospitalized for decompensated DHF. The present investigation was undertaken to define a profile of simple bedside variables and to evaluate their impact on long-term survival in such patients as compared to their SHF counterparts.
Methods
Study population
The study population included 473 randomly chosen patients aged ≥60 years, hospitalized for acutely decompensated HF as the primary diagnosis. HF was of various etiologies and was present for at least 3 months prior to admission. The patients had a New York Heart Association (NYHA) grade II-IV, and all of them were routinely maintained with furosemide. Diagnosis of chronic HF was based on data from previous hospitalizations and/or records from outpatient facilities consistent with modified Framingham criteria for HF [4, 24, 25]. Acute decompensation of HF was defined by the presence of an acute increase of shortness of breath (elevation of NYHA grade to III–IV), lung rales, pulmonary vascular enlargement and/or frank edema detected by chest X-ray at the time of admission [2, 15, 33]. Patients with advanced malignant diseases, significant heart-valve or pericardial disease, cor pulmonale, thyrotoxicosis or dialysis-dependent renal failure were excluded from this study. The study was carried out in accordance with the Declaration of Helsinki and was approved by the local Ethics Committee.
Data collection and analysis
On admission, demographic, clinical, ECG, chest X-ray and laboratory characteristics of the patients were recorded. Echocardiographic data were also collected from standard color two-dimensional and Doppler echocardiographic recordings. On discharge, the main underlying cause of HF, duration of hospital stay and recommended medications were registered. Following discharge, patients were contacted annually. At the end of the follow-up period, the collected data were subjected to statistical analysis. Prevalence and eventual association with all-cause mortality were evaluated for the entire patient group and for the SHF and DHF groups separately. Death was confirmed by hospital or outpatient death certificates.
Anemia was defined as hemoglobin <12 g/dl in females and <13 g/dl in males. Renal function was assessed by estimating glomerular filtration rate (GFR) using MDRD equation [21]. The inclusion cut-off for renal dysfunction was estimated GFR <60 ml/min/1.73 m2 [1, 9]. Cardiac conduction disturbances included atrioventricular or bundle-branch block. SHF was defined as decreased LVEF (<50%). Isolated DHF was diagnosed according to the presence of signs or symptoms of HF simultaneously with preserved LVEF (≥50%) and evidence of diastolic dysfunction (impaired left ventricular relaxation, pseudonormal pattern or restrictive filling, according to the measurement of mitral inflow E to A velocities ratio and deceleration time of E wave) on echocardiogram [3, 7, 16, 26, 32, 34].
Statistical analysis
Statistical analysis was performed using BMDP statistical software [8]. Univariate analysis was applied using Pearson’s χ 2 test for statistical comparison of discrete variables. Analysis of variance (ANOVA) was used for continuous variables. To determine the prognostic significance of variables, survival curves were plotted using Kaplan–Meier method. Mantel–Cox and Breslow’s tests were applied to evaluate significance of the differences between the curves. A P ≤ 0.05 was considered significant. Variables significantly associated with survival (P ≤ 0.1 by univariate analysis) were further evaluated by Cox proportional-hazards model for identification of parameters most significantly associated with mortality.
Results
Baseline characteristics
We investigated 473 HF patients, 290 (61%) with SHF and 183 (39%) with DHF. Their baseline characteristics are presented in Table 1. Hypertension was the most frequently observed primary underlying cause of DHF, while the main etiology of SHF appeared to be CAD. DHF patients demonstrated a shorter duration of preexisting HF (18.7 ± 24 months for DHF vs. 28.9 ± 25 months for SHF, P < 0.001), as well as a prolonged hospitalization time (7.3 ± 4 days for DHF vs. 6.3 ± 4 days for SHF, P = 0.009).
Older age, female sex, hypertension, obesity and atrial fibrillation were found more common in DHF compared to SHF (P ≤ 0.01 for each). In contrast, CAD, higher NYHA grade and cardiac conduction disturbances were more prevalent in the SHF group (P < 0.001 in all comparisons). With respect to prevalence of diabetes mellitus, renal dysfunction, dyslipidemia, anemia, COPD, peripheral arterial disease, non-advanced malignancy and history of stroke, no statistically significant differences were observed between the DHF and SHF groups.
Compared to SHF patients, those with DHF showed an increased frequency of left ventricular hypertrophy and thicker interventricular septum, but fewer segmental wall motion abnormalities and a smaller left ventricular end-diastolic diameter on echocardiographic examination (P < 0.001 in each comparison).
Significant differences were also observed between the treatment regimens of the two groups. Thus, patients with DHF received lower daily furosemide dosages on admission and discharge (P < 0.001). These patients were more frequently discharged with prescription of calcium channel blockers (P < 0.001) or anticoagulants (P = 0.01). Finally, they were less likely to be treated with nitrates (P < 0.001), digoxin (P = 0.004) or antiplatelet agents (P = 0.04). Treatment regimens with other relevant medications were comparable in both groups.
Survival
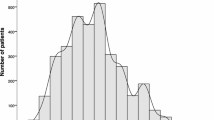
Mean and median follow-up periods in the whole patient group were 47.5 months and 35 months, respectively. During the study period, 231 out of 473 (49%) patients died. The registered one-, three- and five-year survival rates were 77%, 47% and 32%. Fig. 1 illustrates the survival curves of the DHF vs. SHF groups. The respective mean survival durations as well as the one-, three- and five-years survival rates showed no statistically significant difference between the two groups (49 months, 82%, 48% and 33% for DHF, and 45.9 months, 74%, 46% and 30% for SHF, P = 0.3).
Association of various variables with survival: univariate analysis
Variables associated with shorter survival within the entire group were as follows: longer period of preexisting HF (P = 0.04), higher NYHA class (P = 0.002), anemia (P = 0.05), renal dysfunction (P < 0.001), atrial fibrillation (P = 0.008), COPD (P = 0.01), peripheral arterial disease (P = 0.002), history of stroke (P = 0.01), hypermagnesemia (P = 0.004), higher furosemide dosages (>80 mg/day) on discharge (P = 0.02), and digoxin treatment (P = 0.03). Treatments with β-receptor blockers (P = 0.01) or antiplatelet agents (P = 0.004) were, by contrast, associated with better survival.
When the two groups were analyzed separately, shorter survival in the SHF group (Table 2) was associated with higher NYHA class (P = 0.046), presence of CAD (P = 0.03), renal dysfunction (P = 0.006), COPD (P = 0.01), history of stroke (P = 0.01), peripheral arterial disease (P < 0.001), higher furosemide dosages (P < 0.001), and abnormal levels of serum magnesium (either hypomagnesemia or hypermagnesemia, P = 0.002). By contrast, treatment with β-receptor blockers (P = 0.03) predicted better survival in SHF.
In the DHF group (Table 3), shorter survival was associated with longer period of preexisting HF, higher NYHA class, renal dysfunction, history of non-advanced malignancy, atrial fibrillation and treatment with digoxin (P = 0.048, 0.008, 0.04, 0.02, 0.001 and 0.02, respectively). By contrast, antiplatelet and antilipid agents administration predicted longer survival (P = 0.04 and 0.01, respectively).
Variables most significantly associated with survival
When Cox proportional-hazards model was applied to scrutinize the entire patient group (Table 4), the following variables emerged as the most significantly associated with lower survival: atrial fibrillation (P = 0.006), higher NYHA class (P = 0.007), higher furosemide dosages on discharge (P = 0.01), peripheral arterial disease (P = 0.015), renal dysfunction (P = 0.023), non-advanced malignancy (P = 0.026), and increasing age (P = 0.044).
Variables most significantly associated with mortality in SHF differed from those in DHF group (Table 4). In SHF, higher furosemide daily dosages (P < 0.001), older age (P = 0.003), peripheral arterial disease (P = 0.043), and history of stroke (P = 0.066) were most significantly associated with shorter survival. In the DHF group, higher NYHA class (P < 0.001), history of non-advanced malignancy (P = 0.012), and atrial fibrillation (P = 0.066) were most significantly associated with poor survival, while treatment with antilipid agents predicted better survival (P = 0.049).
Discussion
The main objective of the present investigation was to compare the profiles of the patients with DHF and SHF with respect to their bedside clinical variables, and to evaluate their impact on long-term survival. We have found that the two groups substantially differed in their demographic, clinical, ECG and echocardiographic characteristics. Although the two groups did demonstrate similar results with respect to the long-term survival, different clinical variables were associated with prolongation of their vitality.
In relevant publications, the reported diversity in prevalence and prognosis of DHF vary, depending on the methods used for diagnostic purposes, the study design, the cut-off value of LVEF, and the disease process underlying DHF [4, 25, 34]. HF with preserved LVEF has been studied in various distinct populations. These included outpatients [5, 10, 19], inpatients hospitalized for disorders other than HF [15, 22], inpatients with new onset HF [4], patients hospitalized for newly diagnosed or worsened HF [23, 25, 28, 29, 33], a whole population of patients admitted to cardiology service [31], males [30], African–American patients [18], and patients older than 70 years [27]. In our present investigation, we concentrated on a different study population, consisting of older furosemide-treated patients diagnosed for chronic HF prior to hospitalization for acute HF decompensation and subsequently subjected to extensive follow-up period. Their relatively long preexisting HF course was intended to minimize diagnostic bias, common in a setup of a newly diagnosed DHF. Moreover, all of our patients had a rather severe clinical profile of HF, thus requiring a maintenance furosemide treatment.
Similar to data from previous relevant studies, our DHF patients were more likely to be older, females, hypertensive, obese, with atrial fibrillation, lower NYHA class, and receiving calcium channel blockers [4, 5, 10, 15, 17, 19, 22, 23, 25, 27–29, 31, 33]. On the other hand, SHF patients were more likely to suffer from CAD, cardiac conduction disturbances as well as to receive nitrates, digoxin or antiplatelet agents [4, 5, 10, 15, 17, 19, 22, 23, 25, 27–29, 31, 33]. Furthermore, the respective mean daily furosemide dosages on admission (58 vs. 73 mg) and discharge (74 vs. 94 mg) were lower in the DHF group compared to the SHF patients. In addition, our DHF patients were more frequently treated with anticoagulants, probably due to the higher prevalence of atrial fibrillation, compared to previous reports [22, 29, 31].
The preexisting HF period was shorter in our DHF patients compared to the SHF group. Similarly, abridged or comparable preexisting diagnosis periods were previously reported for patients hospitalized with compensated or exacerbated HF [15, 28, 29]. The reason for the shorter duration of preexisting diagnosis in DHF might be a progressive decline of LVEF over time in part of the patients, eventually resulting in SHF [6]. Duration of hospital stay was longer in our DHF group (7.3 vs. 6.3 days). In one of a few relevant studies, the mean hospital stay tended to rise in patients with decreased versus preserved LVEF (15 vs. 13.6 days, respectively [31]), while in others it was similar in both groups (5 vs. 4.9 days [33], and 7.9 versus 7.5 days [28], respectively). Local differences in the routine of medical services may be, in part, responsible for the latter. On echocardiography, DHF in our patients was characterized by more frequent left ventricular hypertrophy, together with less common segmental wall motion abnormalities and lower values of left ventricular end-diastolic diameter, compared to the SHF group. Similar data have been previously reported [3, 5, 15, 17, 19, 34]. Most of these dissimilarities reflect the differences in pathophysiology between the two HF groups [3, 7, 34].
We have also found similar long-term survival in patients with DHF and their SHF counterparts, despite their milder clinical profile (lower NYHA class and lower maintenance furosemide dosages). In a number of previous studies, patients with preserved LVEF were reported to have either better [15, 17, 22, 25, 27–29, 33] or similar [4, 5, 31] prognosis, compared to those with reduced LVEF, the outcome greatly depending on the choice of inclusion criteria and diagnostic methods [4, 25, 34].
In the present investigation, one-year survival rates were found comparable in both groups and similar to those reported recently for hospitalized patients with new-onset HF [4]. On the other hand, information concerning the impact of various clinical variables on the long-term survival in the context of DHF vs. SHF was rather limited [4, 25]. Several predictors of death among patients with reduced and preserved LVEF were found to be similar in a handful of studies [4, 25]. These predictors included age, renal dysfunction, diabetes mellitus, anemia, peripheral arterial disease, dementia, and hyponatremia [4, 25]. However, while male sex was associated with a higher mortality rate only in patients with preserved LVEF, such association was evident only in patients with CAD and reduced LVEF [25].
In the present study, application of univariate statistical analysis combined with further evaluation by Cox proportional-hazards model enabled us to uncover profound differences in the statistical significance of the death predictors between SHF and DHF among our patients. In accordance with previously reported data [4, 25, 27, 33], only higher NYHA class and renal dysfunction were associated with shorter survival in both HF groups. One can conclude that renal insufficiency not only contributed to the severity of HF, but was also responsible for increased mortality of HF patients, by aggravating the impairment of their hemodynamics, electrolyte, acid base, immunological and other mechanisms [9].
In the SHF group, CAD, COPD, peripheral arterial disease, history of stroke, higher furosemide dosages (>80 mg/day) on discharge and abnormal levels of serum magnesium were also found to be significant predictors of poor survival, while treatment with β-receptor blockers was associated with better survival. On evaluation by Cox proportional-hazards model, higher furosemide daily dosages, older age, peripheral arterial disease and history of stroke emerged as the variables most significantly associated with shorter survival in SHF, this being consistent with the reported data [4, 11, 12, 14, 20, 25, 33].
Univariate analysis of the DHF group revealed longer preexisting HF duration, history of non-advanced malignancy, atrial fibrillation and treatment with digoxin to be significantly associated with poor survival. Of interest, treatment with antiplatelet or antilipid agents was also associated with better survival. In accordance with these results, two recent publications reported history of cancer [4] and atrial fibrillation [22] to be the predictors of death in HF patients with preserved LVEF. Moreover, in DHF patients, treatment with digoxin was associated with shorter survival [22], while use of aspirin [22] or statins [13, 22] with longer survival. This detrimental effect of atrial fibrillation on survival in DHF may encourage the attempts to convert atrial fibrillation to sinus rhythm in order to, hopefully, improve the prognosis. The observed negative association of digoxin treatment with survival by us and by others [22] was not evident in ambulatory patients with mild to moderate chronic DHF [1].
In conclusion, we have found that bedside clinical variables, as well as their ability to predict survival, differ between patients with decompensated DHF and SHF. The study might be defined as epidemiologic, since the subject cohort and the duration of surveillance were sufficient. It should be noted, however, that the main limitation of this study was that diastolic dysfunction was not assessed according to the currently used guidelines, since the study started before the latter were introduced. It is possible that improvement in management of relevant comorbidities (including renal dysfunction, peripheral arterial disease, atrial fibrillation, malignancy) as well as pharmacologic measures, such as diminishing maintenance dosages of furosemide in SHF, may substantially decrease these patients’ mortality. Bearing in mind that optimal treatment of DHF patients has not been established thus far, these two main outcomes of the present study, namely limiting the digoxin treatment and maximizing the antiplatelet and antilipid agents, should be a subject of further research.
References
Ahmed A, Rich MW, Fleg JL, Zile MR, Young JB, Kitzman DW, Love TE, Aronow WS, Adams KF Jr, Gheorghiade M (2006) Effects of digoxin on morbidity and mortality in diastolic heart failure: the ancillary digitalis investigation group trial. Circulation 114:397–403
Angermann C, Hoyer C, Ertl G (2006) Differential diagnosis of dyspnea–significance of clinic aspects, imaging and biomarkers for the diagnosis of heart failure. Clin Res Cardiol 95(Suppl 4): 57–70
Aurigemma GP, Gaasch WH (2004) Diastolic heart failure. N Engl J Med 351:1097–1105
Bhatia RS, Tu JV, Lee DS, Austin PC, Fang J, Haouzi A, Gong Y, Liu PP (2006) Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med 355:260–269
Bursi F, Weston SA, Redfield MM, Jacobsen SJ, Pakhomov S, Nkomo VT, Meverden RA, Roger VL (2006) Systolic and diastolic heart failure in the community. JAMA 296:2209–2216
Cahill JM, Ryan E, Travers B, Ryder M, Ledwidge M, McDonald K (2006) Progression of preserved systolic function heart failure to systolic dysfunction: a natural history study. Int J Cardiol 106:95–102
Chatterjee K, Massie B (2007) Systolic and diastolic heart failure: differences and similarities. J Cardiac Fail 13:569–576
Dixon WJ (1993) BMDP Statistical Software. University of California Press, Los-Angeles
Dries DL, Exner DV, Domanski MJ, Greenberg B, Stevenson LW (2000) The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol 35:681–689
Dubourg O, Gueret P, Beauchet A, Nisse-Durgeat S, Ducardonnet A (2008) Focale: study of systolic and diastolic heart failure in a French elderly population. Int J Cardiol 124:188–192
Düngen HD, Apostolović S, Inkrot S, Tahirović E, Krackhardt F, Pavlović M, Putniković B, Lainščak M, Gelbrich G, Edelmann F, Wachter R, Eschenhagen T, Waagstein F, Follath F, Rauchhaus M, Haverkamp W, Osterziel KJ, Dietz R (2008) Bisoprolol vs. carvedilol in elderly patients with heart failure: rationale and design of the CIBIS-ELD trial. Clin Res Cardiol 97:578–586
Eshaghian S, Horwich TB, Fonarow GC (2006) Relation of loop diuretic dose to mortality in advanced heart failure. Am J Cardiol 97:1759–1764
Fukuta H, Sane DC, Brucks S, Little WC (2005) Statin therapy may be associated with lower mortality in patients with diastolic heart failure: a preliminary report. Circulation 112:357–363
Gottlieb SS, Baruch L, Kukin ML, Bernstein JL, Fisher ML, Packer M (1990) Prognostic importance of the serum magnesium concentration in patients with congestive heart failure. J Am Coll Cardiol 16:827–831
Gustafsson F, Torp-Pedersen C, Brendorp B, Seibaek M, Burchardt H, Kobel L; DIAMOND Study Group (2003) Long-term survival in patients hospitalized with congestive heart failure: relation to preserved and reduced left ventricular systolic function. Eur Heart J 24:863–870
Hettwer S, Panzner-Grote B, Witthaut R, Werdan K (2007) Isolated diastolic dysfunction – diagnostic value of tissue Doppler imaging, colour M-mode and N-terminal pro B-type natriuretic peptide. Clin Res Cardiol 96:874–882
Hogg K, Swedberg K, McMurray J (2004) Heart failure with preserved left ventricular systolic function: epidemiology, clinical characteristics, and prognosis. J Am Coll Cardiol 43:317–327
Ilksoy N, Hoffman M, Moore RH, Easley K, Jacobson TA (2006) Comparison of African-American patients with systolic heart failure versus preserved ejection fraction. Am J Cardiol 98:806–808
Kitzman DW, Little WC, Brubaker PH, Anderson RT, Hundley WG, Marburger CT, Brosnihan B, Morgan TM, Stewart KP (2002) Pathophysiological characterization of isolated diastolic heart failure in comparison to systolic heart failure. JAMA 288:2144–2150
Lee DS, Austin PC, Rouleau JL, Liu PP, Naimark D, Tu JV (2003) Predicting mortality among patients hospitalized for heart failure: derivation and validation of a clinical model. JAMA 290:2581–2587
Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, Kusek JW, Van Lente F; Chronic Kidney Disease Epidemiology Collaboration (2006) Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 145:247–254
Lewis BS, Shotan A, Gottlieb S, Behar S, Halon DA, Boyko V, Leor J, Grossman E, Zimlichman R, Porath A, Mittelman M, Caspi A, Garty M (2007) Late mortality and determinants in patients with heart failure and preserved systolic left ventricular function: the Israel Nationwide Heart Failure Survey. IMAJ 9:234–238
Masoudi FA, Havranek EP, Smith G, Fish RH, Steiner JF, Ordin D, Krumholz HM (2003) Gender, age, and heart failure with preserved left ventricular systolic function. J Am Coll Cardiol 41:217–223
McKee PA, Castelli WP, McNamara PM, Kannel WB (1971) The natural history of congestive heart failure: the Framingham study. N Engl J Med 285:1441–1446
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM (2006) Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 355:251–259
Paulus WJ, Tschöpe C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, Marino P, Smiseth OA, De Keulenaer G, Leite-Moreira AF, Borbély A, Edes I, Handoko ML, Heymans S, Pezzali N, Pieske B, Dickstein K, Fraser AG, Brutsaert DL (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J 28:2539–2550
Pernenkil R, Vinson JM, Shah AS, Beckham V, Wittenberg C, Rich MW (1997) Course and prognosis in patients ≥ 70 years of age with congestive heart failure and normal versus abnormal left ventricular ejection fraction. Am J Cardiol 79:216–219
Philbin EF, Rocco TA Jr, Lindenmuth NW, Ulrich K, Jenkins PL (2000) Systolic versus diastolic heart failure in community practice: clinical features, outcomes, and the use of angiotensin-converting enzyme inhibitors. Am J Med 109:605–613
Smith GL, Masoudi FA, Vaccarino V, Radford MJ, Krumholz HM (2003) Outcomes in heart failure patients with preserved ejection fraction: mortality, readmission, and functional decline. J Am Coll Cardiol 41:1510–1518
Varadarajan P, Pai RG (2003) Prognosis of congestive heart failure in patients with normal versus reduced ejection fractions: results from a cohort of 2,258 hospitalized patients. J Card Fail 9:107–112
Varela-Roman A, Grigorian L, Barge E, Bassante P, de la Pena MG, Gonzalez-Juanatey JR (2005) Heart failure in patients with preserved and deteriorated left ventricular ejection fraction. Heart 91:489–494
Vasan RS, Levy D (2000) Defining diastolic heart failure: A call for standardized diagnostic criteria. Circulation 101:2118–2121
Yancy CW, Lopatin M, Stevenson LW, De Marco T, Fonarow GC (2006) Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) Database. J Am Coll Cardiol 47:76–84
Zile MR, Baicu CF, Bonnema DD (2005) Diastolic heart failure: definitions and terminology. Prog Cardiovasc Dis 47: 307–313
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gorelik, O., Almoznino-Sarafian, D., Shteinshnaider, M. et al. Clinical variables affecting survival in patients with decompensated diastolic versus systolic heart failure. Clin Res Cardiol 98, 224–232 (2009). https://doi.org/10.1007/s00392-009-0746-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-009-0746-1