Abstract
Purpose
This study aimed to analyze our radiologically supervised bowel management program (RS-BMP) outcomes in patients with chronic idiopathic constipation (CIC).
Methods
A retrospective study was conducted. We included all patients with CIC who participated in our RS-BMP at Children´s Hospital Colorado from July 2016 to October 2022.
Results
Eighty patients were included. The average time with constipation was 5.6 years. Before our RS-BMP, 95% had received non-radiologically supervised treatments, and 71% had attempted two or more treatments. Overall, 90% had tried Polyethylene Glycol and 43% Senna. Nine patients had a history of Botox injections. Five underwent anterograde continence procedure, and one a sigmoidectomy. Behavioral disorders (BD) were found in 23%. At the end of the RS-BMP, 96% of patients had successful outcomes, 73% were on Senna, and 27% were on enemas. Megarectum was detected in 93% of patients with successful outcomes and 100% with unsuccessful outcomes (p = 0.210). Of the patients with BD, 89% had successful outcomes, and 11% had unsuccessful.
Conclusion
Our RS-BMP has been proven to be effective in treating CIC. The radiologically supervised use of Senna and enemas was the appropriate treatment in 96% of the patients. BD and megarectum were associated with unsuccessful outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic idiopathic constipation (CIC) is children's most common colonic motility disorder [1]. It represents a functional condition of the lower gastrointestinal tract with an estimated prevalence worldwide of 14% [1, 2]. Peak incidence occurs during toilet training age, with no consistent effect of gender on prevalence [3, 4]. Constipation requires proper treatment and long follow-up because it significantly negatively impacts patients' daily and social lives and reduces health-related quality of life [5].
Symptoms include, among others, hard stools, infrequent bowel movements, abdominal pain, painful bowel movements, and pseudo-fecal incontinence. Most patients with CIC suffer from persistent fecal impaction, which should be considered a partial intestinal obstruction. Consequently, after being toilet trained, these patients have involuntary bowel movements in their underwear due to the overflow of soft stools passing around solid retained feces in the rectum. Additionally, urinary symptoms can be present, such as urinary incontinence and urinary tract infections [6,7,8]. CIC is commonly associated with megarectum, facilitating chronic and involuntary bowel movements. Megarectum becomes a low motility zone that enables the persistence or recurrence of fecal impaction and incontinence [7, 9].
CIC is a clinical spectrum with no clinical severity scale, making its management challenging. Children can be treated successfully on one side of the spectrum with minimal life changes, dietary modifications, and pharmacological interventions. However, on the other side, some patients require surgical interventions [6, 10,11,12,13,14,15,16].
Several studies reported the association of behavioral disorders (BD) with CIC and have demonstrated that these children suffer more attention-deficit / hyperactivity disorder (ADHD), autism spectrum disorder (ASD), anxiety, depression, emotional problems, and problems with peers [17,18,19,20,21].
We have a long experience managing patients suffering from idiopathic constipation for many years. They received inadequate amounts of laxatives or non-effective enemas and never had an abdominal x-ray. As a result, these patients continue with symptoms and are classified as refractory constipation to medical treatment. This study aimed to evaluate the outcome of a radiologically supervised bowel management program (RS-BMP) for patients with CIC.
Materials and methods
Study design
We conducted a retrospective, cross-sectional, single-institution, and descriptive study. We included all patients with CIC who participated in the RS-BMP in the Colorectal Center at Children’s Hospital Colorado from July 2016 to January 2023. The RS-BMP lasts for eight successive days. Primary care physicians, pediatricians, or gastroenterologists referred these patients to us. Electronic medical records were reviewed to determine demographics, previous treatment, contrast enema results, rectum size, and behavioral disorder diagnosis. Also, we analyzed outcomes and treatment types after completing SR-BMP. Patients with anorectal malformations, Hirschsprung´s Disease, and spina bifida were excluded. The Colorado Multiple Institutional Review Board approved this study (COMIRB 20-2275).
Definitions
-
CIC: included all patients with constipation lasting more than six months who had been examined and studied to rule out organic etiologies.
-
Successful outcome: On the last day of the RS-BMP, the amount of laxative or the enema recipe effectively produces a big voluntary bowel movement. The patient does not have involuntary bowel movements (feces accidents) between bowel movements. The abdominal radiograph obtained after a bowel movement shows no residual feces in the rectum, sigmoid, and left colon.
-
Unsuccessful outcome: At the end of the RS-BMP, the laxative or enema produces voluntary bowel movements, but the patient continues having involuntary bowel movements (accidents), and/or the abdominal radiograph confirms residual feces in the rectum, sigmoid, or left colon after the bowel movement.
-
Megarectum: a recto-pelvic ratio greater than 0.61 [22].
Statistical analysis
We compared the success rate of the RS-BMP with previous treatment types, duration of constipation, megarectum, and BD. The Student's t-test and Chi-square or Fischer's exact test to compare proportions were used. The statistical analysis was conducted using the 26.0 version of the Statistical Package for the Social Sciences (SPSS®). Statistical significance was considered when a p value was < 0.05.
Results
A total of 80 patients met the inclusion criteria. The average age was 8.5 years (range 1–38 years). The largest age group was 6–9 years, accounting for 36% of the patients. Forty-eight patients (60%) were male. The average duration of constipation was 5.6 years, and the range was 1–17 years. BD was reported in 19 patients (Table 1).
Before RS-BMP
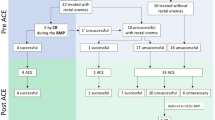
Four patients auto-enrolled in the RS-BMP; they did not receive any treatment prescribed by a physician. Seventy-six (95%) patients had received non-radiologically supervised treatments. Fifty-seven (71%) had attempted two or more treatments. Polyethylene Glycol (PEG) was the most prescribed medication; 90% of patients took PEG. Enemas were used in 46%, Senna in 43%, Botox injection in 11%, antegrade continence enema (ACE) procedure in 6%, and sigmoidectomy in 1% (Fig. 1). Sixty-nine patients had a contrast enema. Forty-six (66%) had megarectum; in 23 (43%), the recto-pelvic ratio was normal.
At the end of RS-BMP
Seventy-seven (96%) patients had a successful outcome. Fifty-seven patients (74%) were successful with Senna, and 20 (26%) with enemas. Sixty-nine patients were on PEG before RS-BMP, and 74% were successful with Senna and 26% with enemas. Similarly, 34 patients took Senna before RS-BMP, and 28 (82%) became successful after adjusting the amount of Senna (Table 2). Forty-three out of 46 (93%) patients with megarectum had a successful outcome, and all 23 (100%) patients with a normal recto-pelvic ratio also were successful (p = 0.210).
Three patients had unsuccessful outcomes. One patient refused to continue taking medication and the use of rectal enemas. We did not find the amount of Senna in one and the adequate enema recipe in the other. Both patients continued with fecal accidents. Two patients had BD.
There was no statistical significance when comparing the average age and duration of constipation between the successful group with the unsuccessful group (p = 0.98 and p = 0.18, respectively).
Sixty-one patients did not have BD; 60 (98%) had successful outcomes, and one (2%) had unsuccessful. Nineteen patients had BD; 17 (89%) had successful outcomes, and 2 (11%) had unsuccessful. There was no statistical significance in the outcome between patients with BD vs. those without BD (p = 0.075).
Discussion
CIC is highly prevalent in children. It harms patients' quality of life and significantly interferes with their social interactions [23,24,25]. As shown in this study, all patients with CIC received medical treatment without following a specific protocol. Over 70% of those patients had attempted two or more treatments. Six patients classified as refractory to medical management underwent an unnecessary surgical procedure, ACE or sigmoidectomy, with no improvement in their constipation.
We have previously demonstrated RS-BMP's effectiveness in treating CIC [10]. Russell K, et al. also published similar data and showed a decrease in hospital and admission and surgical interventions [15]
Our RS-BMP consists of a week-long process of trial and error to determine the adequate amount of laxative or rectal enema recipe for each patient. First, we perform a contrast enema to evaluate the characteristics of the rectum and sigmoid. Then, we check for fecal impaction, and if present, the patient undergoes a clean-out protocol based on enemas with daily radiological monitoring to confirm successful colon emptying objectively.
Our RS-BPM for CIC entails, in most cases, an initial cleaning of the colon. Then, based on the surgeon's experience during RS-BMP, the presence of megarectum, chronicity, history of overflow pseudo-fecal incontinence, regression using diapers, and significant social problems such as bullying and social isolation, it is worth considering using enemas for a period before attempting a laxative trial. The remaining patients are considered good candidates to start laxative trials.
The use of laxatives is based on trial and error. Our preference is to use a stimulant laxative, Senna. The initial dose is determined according to the characteristics described in the previous paragraph. The amount of Senna is adjusted daily based on the response to the initial dose. We evaluate the presence and characteristics of the feces and the occurrence of fecal soiling. But residual feces in the rectum, sigmoid, and left colon observed in the abdominal radiograph, obtained immediately after the bowel movement, is the most objective approach to maintain, increase, or reduce the amount of laxative.
According to the previously described, we proceed as follows:
-
1.
If there is no bowel movement after 24 h of the Senna dose, a rectal enema is given, and the amount of Senna is increased.
-
2.
The dose is also increased if there is a bowel movement, but the abdominal radiograph shows residual feces in the rectum.
-
3.
The laxative dose is decreased if the family reports multiple liquid or soft bowel movements and the abdominal x-ray is clean (no residual feces in the rectum).
-
4.
Finally, we keep the same amount of Senna if the patient has voluntary bowel movements, and the abdominal radiograph shows no residual feces in the rectum.
-
5.
Some patients need high doses of Senna to have a successful outcome. However, some patients suffer from nausea, abdominal pain, vomiting, and poor quality of life. In those scenarios, we consider changing them to rectal enemas.
For the use of enemas, the amount of normal saline, glycerin, and castile soap is also determined based on the contrast enema and surgeon experience. It is adjusted daily according to the number of bowel movements in 24 h and the amount of stool in the rectum, sigmoid, and left colon seen on the daily abdominal radiograph obtained after the bowel movement.
After completing the eight days of the RS-BMP described earlier, our success rate of 96% was like previous publications [10, 15]. Over 80% of the patients on Senna before our RS-BMP were successful after adjusting the dosage. Similarly, most patients on enemas, even those who underwent ACE, Botox injection, and sigmoidectomy, were successful with Senna. This emphasizes the positive impact of the adequate use of Senna based on daily clinical and radiological findings.
We had three patients with unsuccess outcomes. One refused to continue the treatment at the end of the RS-BMP week. The second patient, besides CIC, had ADHD, Ehlers-Danlos syndrome, and megarectum. The laxative protocol was attempted, but the patient continued to experience involuntary bowel movements. The last unsuccessful patient had ASD and megarectum. The enema-based protocol was tried; however, despite many adjustments to the enema recipe, we could not find the proper amount to keep the colon clean. EDS [26] and ADHD [20] have been associated with CIC, and it has been reported that these conditions could affect the chances of a successful BMP outcome.
Megarectum is a disorder that appears secondary to CIC [22]. It represents a life condition that makes CIC treatment challenging [13]. In the present study, the average duration of constipation was 5.6 years; by that time, 66% of the patients had megarectum. Although a megarectum did not show statistical significance in terms of success rate, it was interesting that the three patients with unsuccessful outcomes had a megarectum. It has been reported that most patients with CIC and megarectum can achieve success under protocolized BMP [10]. However, these patients were predisposed to fecal impaction and the need for higher doses of laxatives, which could cause nausea, abdominal pain, and vomiting. Finally, some patients require rectosigmoid resection [13]. These circumstances emphasize the importance of timely referral and the practice of RS-BMP. Some patients underwent ACE without previous proper RS-BMP. However, we have found [27] that the success rate of antegrade enemas is considerably higher after a RS-BMP with rectal enemas. Therefore, creating an ACE without a previous rectal enema program does not guarantee a successful outcome.
Following a RS-BMP is essential in the management of CIC. Unfortunately, late referrals are common in these challenging patients, leading to unnecessary interventions.
Conclusions
The Radiologically Supervised Bowel Management Program has been proven to be effective in treating Chronic Idiopathic Constipation.
Abbreviations
- ACE:
-
Antegrade continence enema
- ADHD:
-
Attention-deficit/hyperactivity disorder
- ASD:
-
Autism spectrum disorder
- BD:
-
Behavioral disorders
- RS-BMP:
-
Radiologically supervised bowel management program
- CIC:
-
Chronic idiopathic constipation
References
Levitt MA, Peña A (2005) Surgery and constipation: when, how, yes, or no? J Pediatr Gastroenterol Nutr 41(Suppl 1):S58-60. https://doi.org/10.1097/01.scs.0000180308.02052.b2
Luthra P, Camilleri M, Burr NE, Quigley EMM, Black CJ, Ford AC (2019) Efficacy of drugs in chronic idiopathic constipation: a systematic review and network meta-analysis. Lancet Gastroenterol Hepatol 4(11):831–844. https://doi.org/10.1016/S2468-1253(19)30246-8
Suares NC, Ford AC (2011) Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol 106(9):1582–1591. https://doi.org/10.1038/ajg.2011.164
Loening-Baucke V (1993) Chronic constipation in children. Gastroenterology 105(5):1557–1564. https://doi.org/10.1016/0016-5085(93)90166-a
Mugie SM, Di Lorenzo C, Benninga MA (2011) Constipation in childhood. Nat Rev Gastroenterol Hepatol 8(9):502–511. https://doi.org/10.1038/nrgastro.2011.130
Wald A, Scarpignato C, Kamm MA, Mueller-Lissner S, Helfrich I, Schuijt C et al (2007) The burden of constipation on quality of life: results of a multinational survey. Aliment Pharmacol Ther 26(2):227–236. https://doi.org/10.1111/j.1365-2036.2007.03376.x
Vriesman MH, Koppen IJN, Camilleri M, Di Lorenzo C, Benninga MA (2020) Management of functional constipation in children and adults. Nat Rev Gastroenterol Hepatol 17(1):21–39. https://doi.org/10.1038/s41575-019-0222-y
Kirgizov IV, Minaev SV, Shishkin I, Aprosimova S, Ukhina L (2019) Surgical treatment of idiopathic megarectum in constipated children. J Pediatr Surg 54(7):1379–1383. https://doi.org/10.1016/j.jpedsurg.2018.10.103
De La Torre L, Cogley K, Calisto J, Nace G, Correa C (2016) Primary sigmoidectomy and appendicostomy for chronic idiopathic constipation. Pediatr Surg Int 32(8):767–772. https://doi.org/10.1007/s00383-016-3913-2
Bischoff A, Brisighelli G, Dickie B, Frischer J, Levitt MA, Peña A (2018) Idiopathic constipation: a challenging but manageable problem. J Pediatr Surg 53(9):1742–1747. https://doi.org/10.1016/j.jpedsurg.2017.09.022
Morishita D, Tomita T, Mori S, Kimura T, Oshima T, Fukui H, Miwa H (2021) Senna versus magnesium oxide for the treatment of chronic constipation: a randomized. Placebo-Controlled Trial Am J Gastroenterol 116(1):152–161. https://doi.org/10.14309/ajg.0000000000000942
Menees SB, Lembo AJ, Chey WD (2022) Polyethylene glycol 3350 in the treatment of chronic idiopathic constipation: post hoc analysis using FDA endpoints. Can J Gastroenterol Hepatol 2022:3533504. https://doi.org/10.1155/2022/3533504
De la Torre L, Cogley K, Cabrera-Hernández MA, Frias-Mantilla JE, Wehrli LA (2019) Transanal proximal rectosigmoidectomy. A new operation for severe chronic idiopathic constipation associated with megarectosigmoid. J Pediatr Surg 54(11):2311–2317. https://doi.org/10.1016/j.jpedsurg.2019.04.009
Levitt MA, Martin CA, Falcone RA Jr, Peña A (2009) Transanal rectosigmoid resection for severe intractable idiopathic constipation. J Pediatr Surg 44(6):1285–1290. https://doi.org/10.1016/j.jpedsurg.2009.02.049. (discussion 1290-1)
Russell KW, Barnhart DC, Zobell S, Scaife ER, Rollins MD (2015) Effectiveness of an organized bowel management program in the management of severe chronic constipation in children. J Pediatr Surg 50(3):444–447. https://doi.org/10.1016/j.jpedsurg.2014.08.006
Ahmadi J, Azary S, Ashjaei B, Paragomi P, Khalifeh-Soltani A (2013) Intrasphincteric botulinum toxin injection in treatment of chronic idiopathic constipation in children. Iran J Pediatr 23(5):574–578
Rajindrajith S, Ranathunga N, Jayawickrama N, van Dijk M, Benninga MA, Devanarayana NM (2020) Behavioral and emotional problems in adolescents with constipation and their association with quality of life. PLoS ONE 15(10):e0239092. https://doi.org/10.1371/journal.pone.0239092
Kilincaslan H, Abali O, Demirkaya SK, Bilici M (2014) Clinical, psychological and maternal characteristics in early functional constipation. Pediatr Int 56(4):588–593. https://doi.org/10.1111/ped.12282
Çağan Appak Y, Yalın Sapmaz Ş, Doğan G, Herdem A, Özyurt BC, Kasırga E (2017) Clinical findings, child and mother psychosocial status in functional constipation. Turk J Gastroenterol 28(6):465–470. https://doi.org/10.5152/tjg.2017.17216
McKeown C, Hisle-Gorman E, Eide M, Gorman GH, Nylund CM (2013) Association of constipation and fecal incontinence with attention-deficit/hyperactivity disorder. Pediatrics 132(5):e1210–e1215. https://doi.org/10.1542/peds.2013-1580
Fu SC, Lee CH, Wang H (2021) Exploring the association of autism spectrum disorders and constipation through analysis of the gut microbiome. Int J Environ Res Public Health 18(2):667. https://doi.org/10.3390/ijerph18020667
van der Plas RN, Benninga MA, Staalman CR, Akkermans LM, Redekop WK, Taminiau JA, Buller HA (2000) Megarectum in constipation. Arch Dis Child 83(1):52–58. https://doi.org/10.1136/adc.83.1.52
Youssef NN, Langseder AL, Verga BJ, Mones RL, Rosh JR (2005) Chronic childhood constipation is associated with impaired quality of life: a case-controlled study. J Pediatr Gastroenterol Nutr 41(1):56–60. https://doi.org/10.1097/01.mpg.0000167500.34236.6a
Arruda VPA, Bellomo-Brandão MA, Bustorff-Silva JM, Lomazi EA (2020) Refractory functional constipation: clinical management or appendicostomy? J Pediatr (Rio J) 96(2):210–216. https://doi.org/10.1016/j.jped.2018.09.001
Clarke MC, Chow CS, Chase JW, Gibb S, Hutson JM, Southwell BR (2008) Quality of life in children with slow transit constipation. J Pediatr Surg 43(2):320–324. https://doi.org/10.1016/j.jpedsurg.2007.10.020
Thwaites PA, Gibson PR, Burgell RE (2022) Hypermobile Ehlers-Danlos syndrome and disorders of the gastrointestinal tract: what the gastroenterologist needs to know. J Gastroenterol Hepatol 37(9):1693–1709. https://doi.org/10.1111/jgh.15927
Reppucci ML, Nolan MM, Cooper E, Wehrli LA, Schletker J, Ketzer J et al (2022) The success rate of antegrade enemas for the management of idiopathic constipation. Pediatr Surg Int 38(12):1729–1736. https://doi.org/10.1007/s00383-022-05214-y
Funding
This research received no specific grant from public, commercial, or not-for-profit funding agencies.
Author information
Authors and Affiliations
Contributions
Study conception and design: LT, AB, AD-M. Data acquisition: AD-M, LAW, JK, VR, LS, AM and MW. Analysis and data interpretation: LT, AD-M, LJ-G. Drafting of the manuscript: LT, AD-M. Critical revision: LT, AB, AP, AD-MM. Figures and Tables: LT, AB, AP, AD-M All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Domínguez-Muñoz, A., Bischoff, A., Wehrli, L.A. et al. Radiologically supervised bowel management program outcome in patients with chronic idiopathic constipation. Pediatr Surg Int 39, 229 (2023). https://doi.org/10.1007/s00383-023-05508-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05508-9