Abstract
Purpose
Children with Hirschsprung’s disease (HD) and anorectal malformations (ARM) may benefit from a bowel management program (BMP) to treat constipation and fecal incontinence. This study describes a pilot BMP in Uganda.
Methods
Patients treated for HD or ARM were recruited for the BMP. Local staff underwent training and progressively took over decision-making. The rates of patient involuntary bowel movements (IBMs) and provider confidence were evaluated pre- and post-BMP with questionnaires. The results were compared with Fischer’s exact test.
Results
Ten staff—2 surgeons, 6 nurses and 2 physiotherapists—and 12 patients participated. Patient median age was 4.5 years (IQR 3–6.6) and ten were male. Ten reported at least daily IBMs prior to the BMP. All patients underwent a clean-out. The parents were then taught to perform daily enemas or irrigations. Specific regimens were determined by patient history and imaging and titrated throughout the BMP. There were differences in the rates of both daytime and nighttime IBMs before and after the BMP (p = 0.0001 and 0.002, respectively). All staff reported increased confidence.
Conclusions
We describe the first BMP in Uganda. BMPs can successfully treat constipation and fecal incontinence in low-income countries, although there are challenges with resources and follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Children with anorectal malformation (ARM) or Hirschsprung’s disease (HD) often suffer from constipation and fecal incontinence with significant related morbidity, social isolation, and decreased quality of life. Formal bowel management programs (BMPs) have been developed to address constipation and fecal incontinence in this population and help these children remain clean and free from soiling [1,2,3,4]. In high-resource settings, several BMPs have clearly demonstrated significant improvement in the rates of incontinence, pseudo-incontinence, and severe constipation with improvement in overall quality of life for children and families who participate. As many as 60–80% of patients who participate experience a significant improvement in fecal continence and quality of life [5,6,7,8]. For example, in patients with ARM specifically suffering from fecal incontinence, over 70% remain clean without incontinence following medical therapy as part of a BMP [6].
However, there are very few BMPs outside of high-income countries (HICs), with only three reported in the literature in low-middle-income countries (LMICs) or middle-income countries [9,10,11]. An evaluation of a BMP in China demonstrated improved continence and quality of life at 2 years [9]. Similarly, BMPs in Egypt and Iran also both report improved quality of life for children with fecal incontinence following therapy [10, 11]. However, to our knowledge, there are no reported BMPs from low-income countries (LICs) in the literature, particularly in Sub-Saharan Africa which is predominantly low income or low–middle income (Fig. 1) [12].
Conversely, children with ARM and HD in lower resource settings are at high risk of suffering from fecal incontinence and severe constipation. In Uganda, nearly half of ARM patients evaluated after primary posterior sagittal anorectoplasty (PSARP) and colostomy closure report at least daily soiling [13]. This is at least partially due to delays in care [14], which can subsequently lead to prolonged periods of constipation, potentially exacerbating bowel dysmotility. At a large referral center in Uganda, over 60% of ARM patients had a delayed presentation (> 48 h after birth), and all patients underwent initial diversion instead of PSARP [15]. Similarly, patients with HD in LMIC often present after a significant delay with fecal impaction [16]; for example, 80% of patients with HD presenting after delay in a LIC had a palpable fecaloma on exam [17]. The severe constipation can then lead to stool overflow manifesting as pseudo-incontinence with soiling.
Furthermore, in LICs like Uganda, there are fewer resources available to manage incontinence with significant resulting quality of life concerns. For example, families of children with HD or ARM who have ostomies report social isolation. They often are unable to attend school, church or other social/community functions, and their families have further socioeconomic concerns as a result [18]. Similarly, even after stoma reversal, the implication of persistent soiling for children is more significant in LICs than higher resource settings as children cannot attend school with daily soiling. Children with ARM and HD in lower resource settings are at high risk of fecal incontinence with associated morbidity and quality of life concerns, yet they often have few management options and no formal treatment programs available to them.
The pediatric surgery team at a tertiary referral center in Uganda, in conjunction with supporting partners involved in a BMP in a HIC, sought to adapt and pilot a BMP in Uganda. The goal of this paper is to describe the process of adapting a BMP from a HIC setting to a LIC setting, describe the lessons learned, and evaluate the initial efficacy of the pilot program.
Methods
Setting
The pilot BMP was carried out at a tertiary referral center in Uganda in June 2022. Prior to conducting the program, IRB approval was obtained from both the local institution and the institution affiliated with the HIC partners. The hospital in Uganda is a 400+ bed regional referral center that serves a catchment area of over 3 million and supports one of the few dedicated pediatric surgery centers in the country. The pediatric surgery program includes pediatric surgeon specialists, pediatric surgery fellows, residents, nurses, physiotherapists, and support staff. They treat a wide range of disorders, including patients with ARMs and HD [14].
An initial needs and resource assessment was performed by the local site project lead and partners. This consisted of an evaluation of local human resources including staff availability and necessary time commitment, physical resources with space to conduct the BMP, equipment availability, pharmacologic resources, radiologic capabilities/availability, and cost. The pediatric surgery program manages a large number of patients with ARM and HD who have completed definitive therapy. A small number of these patients were selected by staff to participate in the pilot program.
BMP logistics
The pilot BMP was conducted over 10 days in June 2022. At the start of the program, all patients received abdominal radiographs and then were evaluated by the full team comprised of local staff and HIC partners who included a pediatric colorectal surgeon, pediatric colorectal surgery nurse practitioner, and surgical resident. During the initial assessment, a detailed past surgical and medical history along with characterization of the incontinence and/or severe constipation was performed, followed by physical examination. Based on the history, physical exam, and radiographs, an initial clean-out strategy and initial enema regimen was selected.
The patients then spent 2 days undergoing the clean-out, which consisted of rectal irrigations and/or enemas. Following the initial clean-out, they began a daily enema regimen. Abdominal radiographs were obtained on the first day after initiation of the enemas, and then selectively thereafter. Over the next 5 to 7 days, the patients were evaluated daily to assess the effectiveness of the enema therapy, and the enema regimens were titrated as needed.
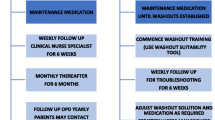
Initially, the daily evaluations, titrations, and enema therapy were conducted largely by partners from a HIC with experience in a BMP, supported by the local staff. Thereafter, the local staff took progressive ownership of each aspect of the evaluation and therapy, including making decisions on therapy titration and troubleshooting enema administration. Near the end of the program, the local staff then taught the families how to perform the enemas and troubleshoot complications.
Training
The training consisted of a mix of hands-on demonstrations, PowerPoint presentations, pamphlet materials, and direct patient care. Topics included how to perform the initial assessment, choosing an initial therapy, how to perform a daily assessment, general guidelines for enema titration, practical tips for troubleshooting, how to evaluate abdominal radiographs in the context of a BMP, and post-BMP discharge planning. Several topics were presented each day based on the phase of care during the BMP. Most of the direct patient care including enema administration and teaching took place in one of two open ward rooms with multiple families admitted in each room. In this context, multiple staff and multiple patient families could observe and learn from each other during each child’s evaluation and enema therapy.
Survey development and analysis
To evaluate the initial efficacy of the BMP, both participating staff and patient families were surveyed before and after the BMP. The staff survey was designed to evaluate prior staff knowledge of bowel management principles, along with their confidence managing fecal incontinence and severe constipation in this population before and after the BMP. Family surveys were adapted from prior studies evaluating fecal incontinence in the context of a BMP, and specifically from the Pediatric Fecal Incontinence Severity Score (PFISS) [5]. The surveys were administered immediately prior to the BMP, within 2 weeks of completion of the BMP, and at approximately 6-month follow-up. The primary outcome from the survey was the rate of reported fecal incontinence. An additional brief survey instrument was used at the 6-month follow-up to evaluate for any barriers or challenges to continued enema therapy, and to evaluate family satisfaction with the BMP. Surveys of patients were conducted by local staff in the patient’s native language. Fischer’s exact test was used to compare results pre- and post-BMP.
Results
Staff training and survey results
A total of ten staff participated in the BMP. This included two physicians—one pediatric surgeon and one pediatric surgery fellow—six nurses, and two physiotherapists. All the staff participated throughout the program with the nurses and physiotherapists taking over primary responsibility for the decision-making and family teaching by the end of the program.
On pre-BMP survey, eight of ten staff had heard of a BMP before, all ten staff felt a BMP would be important for their patients, and four of ten reported routinely performing some type of bowel management for these patients. On the pre-BMP survey, when asked to self-report their confidence in managing fecal incontinence or severe constipation for patients with HD or ARM, only one person felt very confident, while six reported average confidence, and three reported below average confidence. The results were significantly different on post-BMP survey (p = 0.013); no one reported below average confidence, two reported average confidence, two reported above average confidence and six staff reported that they felt very confident (Fig. 2).
Patient demographics and survey results
There were 12 patients who participated in the BMP (Table 1). Patient median age was 4.5 years (IQR 3–6.6). Ten were male (83%). Eight patients (67%) had ARM, while four (33%) had HD. Ten reported at least daily involuntary bowel movements prior to the BMP, with multiple families consequentially reporting social isolation and their child “being chased out of school.” With regard to fecal urgency, three reported the ability to sense the need to stool, four reported no ability to sense the need to stool, while one patient never stooled without an enema, and it was unclear for four patients who were mostly younger. All 12 patients reported daytime urinary continence. On initial X-rays, all had a significant stool burden, at least four had notable stool balls, one had a large/redundant sigmoid colon and one had a megarectum. After initial assessment, they all underwent a clean-out consisting of irrigations and enemas over the course of 2 days. The patient with the megarectum was then started on daily irrigations instead of an enema regimen, while the 11 other patients were started on an enema regimen.
There were significant differences in the rates of both daytime and nighttime involuntary bowel movements within 2 weeks post-BMP compared to pre-BMP (p = 0.0001 and 0.002, respectively, Fig. 3). For example, 10 of 12 patients pre-BMP reported at least daily daytime involuntary bowel movements while two reported no involuntary daytime bowel movements. Post-BMP, 10 of 12 families reported no daytime involuntary bowel movements, while one patient reported a rate of 1–2 times per week and another reported a rate of 3–4 times per week.
Nine patients were able to make the 6-month follow-up visit, while three of the original patients could not be reached and did not follow-up. At 6 months, eight of nine patients were still continuing the therapy, while one of the eight had transitioned to several weekly enemas instead of daily enemas and reported remaining free from soiling. All nine patients reported technical challenges at some point over the last 6 months, largely related to broken equipment. Several were able to buy foley replacements locally, while most had to get the equipment (foleys and enema bags) replaced at a facility. Three of the nine also reported difficulty finding supplies to make the enemas, and in particular, appropriate soap. For example, one family reported sending a boda boda (motorcycle driver) into a neighboring town to find the soap additive. All nine families said that if they could do it over they would participate again, and all nine would highly recommend the program to similar families.
The improvement in fecal incontinence was maintained at the 6-month follow-up. There was still a statistically significant difference in the rates of both daytime and nighttime involuntary bowel movements at the 6-month follow-up compared to pre-BMP (p = 0.0011 and p = 0.0012, respectively). Two patients reported less than once weekly daytime involuntary bowel movements, while the rest reported no daytime involuntary bowel movements. Only one patient reported a rate of 1–2 involuntary nighttime bowel movements per week while the rest reported none (Fig. 4).
Discussion
Bowel management programs can significantly improve the quality of life for children with ARM or HD who suffer from fecal incontinence and severe constipation. Here, we demonstrate that despite some challenges, BMPs can be adapted to lower resource settings. This is the only BMP in Uganda, and to our knowledge, the first report of a pilot BMP in a LIC. The pilot program was effective in improving local capacity for managing fecal incontinence and severe constipation, with significant improvements in self-reported confidence by staff who participated. Nursing and other allied health professionals have been integral to the implementation of BMPs in HICs, and similarly in Uganda, nurses and physiotherapists were essential. By the end of the pilot program, they were the primary providers managing the program and interfacing with patients and their families. Since completion of the pilot program in June 2022, local staff have continued to independently apply bowel management principles and therapies for other children with ARM or HD suffering from fecal incontinence or severe constipation.
In addition to increasing staff confidence and subsequent independent practice, the follow-up surveys also support improved patient outcomes as a result of the BMP. While the sample size was intentionally small with only 12 patients, there were substantial improvements in both daytime and nighttime fecal incontinence immediately following completion of the BMP and at 6 months for 9 of the 12 patients who completed follow-up. Most families reported technical and resource-related challenges at 6 months follow-up, but they also reported continued therapy, improved fecal continence, and would still highly recommend the program to other families in similar situations. BMPs in high-income and middle-income country settings have been effective at improving rates of fecal incontinence and patient quality of life outcomes [5,6,7,8,9,10,11]. The data from this pilot program, albeit limited to a small patient population, would seem to support the feasibility and efficacy of adapting and implementing a BMP in a lower resource setting.
One of the keys to implementing this BMP was performing a local needs and resource assessment and allowing those assessments to inform program implementation. For example, while many BMPs in HICs treat patients with a variety of pathologies, and the majority of patients may even have idiopathic constipation [5, 8], the population of interest for this initial LIC BMP focused on children with HD or ARM managed by the local pediatric surgery team. The majority of these patients in this setting suffer either from pseudo-incontinence as a result of severe, prolonged constipation with limited access to medical therapy, or from true incontinence resulting from anatomical defects including defects in sensation, sphincter control, and/or dysmotility [2,3,4]. As a result, these patients will require initial, and potentially prolonged, enema therapy. For those with true incontinence, they may require lifelong enema therapy. In addition, for those with severe pseudo-incontinence, prolonged initial enema therapy is necessary to deal with the severe constipation/stool burden, to allow the child to experience what an empty rectum feels like, and to allow an enlarged rectum/colon to appropriately contract over time. Therefore, while some patients in this population may ultimately transition to laxative therapy, all will require enemas as an essential first step. On the other hand, the initial resource assessment highlighted the fact that common laxatives may not be widely available in Uganda, or when they are available, they may be cost-prohibitive for most patients. The additives for enemas commonly used in HICs can also be difficult or cost-prohibitive to acquire, but there are some milder soaps or shampoos available. Given the population of interest and the resources available, it became clear that in this setting an enema only program (at least initially) could be successful. Indeed, the decision to pursue an enema only initial program also allowed the teaching and training to remain focused on a single therapy which may have helped facilitate adoption. This lesson could similarly be applied to other resource limited settings with ARM and HD patients who suffer from more severe fecal incontinence and constipation.
Based on the initial resource assessment, it was also clear that obtaining daily radiographs would be difficult. The films are expensive, and coordinating to ensure the images are taken shortly after completing enema therapy can also be challenging. As such, the team elected to perform initial imaging, but then only selective evaluation thereafter based on whether there was difficulty finding an effective “enema recipe” or if there was a concern for inadequate stool evacuation.
It is also worth highlighting several of the strengths of the environment in Uganda that contributed to its success. First, there are different cultural expectations around privacy that allowed for mutual support and learning. The pediatric surgery ward is primarily made up of two larger rooms that each house multiple families. In this case, the local team cleared out the elective schedule so that the staff could focus primarily on the BMP. Each room then “housed” six families participating in the BMP. Nearly, all the patient care took place in these larger, communal settings. As a result, multiple staff members could observe each patient assessment and participate in decision-making. Similarly, families often supported each other and learned from each other during enema administration and troubleshooting. Coupled with both high levels of motivation and an expectation for hands-on learning, this led to very quick adoption by both local staff and families.
Challenges to BMP implementation
Lastly, it is worth briefly highlighting some of the additional challenges to implementing a BMP in a lower resource setting. First, as already mentioned it may be difficult to find widely available laxative or motility therapies, and even the additives for the enema therapy may be difficult to obtain. In Uganda, detergents which include harsher chemicals that are inappropriate for enema administration are widely used as “soap”. While glycerin is available, it would be cost-prohibitive for many families, and other brands of “baby soap” can similarly be difficult to acquire. Ultimately, the local team leads and study partners went to local grocery stores and markets to find a soap that would hopefully be available to patients. Even so, at the 6-month follow-up, three of nine patients still reported difficulty finding the additive in order to make the enemas. There were additional challenges around replacing broken catheters and/or enema bags, and many of the patients had to return to the tertiary level facility to find these supplies. Lastly, it is also worth highlighting the challenges of following these patients. Despite extensive efforts by the local team, 25% (3/12) of patients could not be reached at 6 months and even for those who did follow-up, there may be logistical barriers and associated financial concerns. Lastly, the need for adequate space has been a challenge, and during the initial BMP, the team had to postpone elective cases.
Future direction
The local team has already expanded the program, treating new patients with ARM or HD who suffer from severe constipation or fecal incontinence. There are ongoing challenges around the logistics of expanding the BMP and providing high quality care, nevertheless, the team is committed to this goal. Similarly, there is also the hope of expanding the BMP to other facilities given the challenges associated with travel for many patients. There is further need for additional mid-term and long-term follow-up to continue to evaluate the efficacy of a BMP in this context. There are ongoing efforts to identify appropriate laxative and motility agents that could be used for those patients who successfully maintain an enema therapy and wish to attempt to transition to oral therapy. Lastly, there is also an opportunity and need to consider other aspects of an effective BMP including diet and nutrition counseling/education, and potentially incorporating pelvic floor physical therapy treatments.
Conclusions
There is significant need for BMPs in LICs to help patients with ARM and HD who suffer from fecal incontinence and/or severe constipation. We report the implementation of the first BMP in Uganda, and to our knowledge, the first in a LIC setting reported in the literature. Despite intentionally smaller numbers for this pilot program, we highlight the potential feasibility and efficacy of an enema only program to effectively treat fecal incontinence and severe constipation for these patients. Continued expansion to treat additional patients and incorporate additional therapies, along with further evaluation of long-term outcomes in this setting, are needed.
Data availability
Sample teaching resources and survey tools have been made available in the supplemental files. Given the small sample size and concerns about patient confidentiality, individual patient data is not available.
References
Peña A, Guardino K, Tovilla JM, Levitt MA, Rodriguez G, Torres R (1998) Bowel management for fecal incontinence in patients with anorectal malformations. J Pediatr Surg 33(1):133–137
Bischoff A, Levitt MA, Peña A (2009) Bowel management for the treatment of pediatric fecal incontinence. Pediatr Surg Int 25(12):1027–1042
Levitt MA, Martin CA, Olesevich M, Bauer CL, Jackson LE, Peña A (2009) Hirschsprung disease and fecal incontinence: diagnostic and management strategies. J Pediatr Surg 44(1):271–277 (discussion 7)
Levitt MA, Peña A (2010) Pediatric fecal incontinence: a surgeon’s perspective. Pediatr Rev 31(3):91–101
Lim IIP, Cushing CC, Jenkins T, Troutt M, Zeller MH, Hossain M et al (2021) Prospective quality of life outcomes in pediatric fecal incontinence following bowel management. J Pediatr Surg 56(8):1459–1464
Wood RJ, Vilanova-Sanchez A, El-Gohary Y, Ahmad H, Halleran DR, Reck-Burneo CA et al (2021) One-year impact of a bowel management program in treating fecal incontinence in patients with anorectal malformations. J Pediatr Surg 56(10):1689–1693
Colares JH, Purcaru M, da Silva GP, Frota MA, da Silva CA, Melo-Filho AA et al (2016) Impact of the bowel management program on the quality of life in children with fecal incontinence. Pediatr Surg Int 32(5):471–476
Kilpatrick JA, Zobell S, Leeflang EJ, Cao D, Mammen L, Rollins MD (2020) Intermediate and long-term outcomes of a bowel management program for children with severe constipation or fecal incontinence. J Pediatr Surg 55(3):545–548
Wang Y, Liang H, Wu Q, Zheng H, Liu G, Wen Z et al (2017) Bowel management program for pediatric postoperative fecal incontinence in China: a surgeon’s experience. Medicine (Baltimore) 96(22):e7078
Gabr AA, Gad MA, Shalaby A (2020) Quality of life in children with pseudoincontinence after implementing a bowel management program in Egypt. J Pediatr Surg 55(2):261–264
Shahba Z, Ahmadi B, Haji Bandeh S, Hosseinpour M (2022) Evaluation of bowel management program on quality of life in children with fecal incontinence. Adv Biomed Res 11:69
The World Bank, World Development Indicators (2022). The World by Income [Data file]. Retrieved from https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html Accessed 19 Sept 2023
Oyania F, Ogwal A, Nimanya S, Muzira A, Kakembo N, Kisa P et al (2020) Long term bowel function after repair of anorectal malformations in Uganda. J Pediatr Surg 55(7):1400–1404
Pilkington M, Situma M, Winthrop A, Poenaru D (2018) Quantifying delays and self-identified barriers to timely access to pediatric surgery at Mbarara Regional Referral Hospital. Uganda J Pediatr Surg 53(5):1073–1079
Kayima P, Kitya D, Punchak M, Anderson GA, Situma M (2019) Patterns and treatment outcomes of anorectal malformations in Mbarara Regional Referral Hospital. Uganda J Pediatr Surg 54(4):838–844
Trinidad S, Kayima P, Kotecha V, Massenga A, Rymeski B, Frischer JS et al (2022) Hirschsprung’s disease in low- and middle-income countries. Semin Pediatr Surg 31(2):151163
Ekenze SO, Ngaikedi C, Obasi AA (2011) Problems and outcome of Hirschsprung’s disease presenting after 1 year of age in a developing country. World J Surg 35(1):22–26
Muzira A, Kakembo N, Kisa P, Langer M, Sekabira J, Ozgediz D et al (2018) The socioeconomic impact of a pediatric ostomy in Uganda: a pilot study. Pediatr Surg Int 34(4):457–466
Author information
Authors and Affiliations
Contributions
Study conception and design: ST, FO, MO, MK, and MS. Acquisition of data: ST, FO, CB, IN, MO, CO, and MK. Analysis and interpretation of data: ST, FO, CB, IN, MO, CO, and MK. Drafting of manuscript: ST. Critical revision of manuscript: FO, CO, and MK.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Trinidad, S., Oyania, F., Bingana, C. et al. Pilot bowel management program at Mbarara Hospital, Uganda. Pediatr Surg Int 39, 292 (2023). https://doi.org/10.1007/s00383-023-05574-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05574-z