Abstract
Purpose
We aimed to evaluate patients who had undergone pediatric LDLT with small-for-size graft (SFSG) and identify risk factors of graft failure to establish a preoperative graft selection strategy.
Methods
The data was collected retrospectively. SFSG was used in 14LDLTs (5.7 %) of 245 LDLTs performed between May 2001 and March 2014. The mean patient age and body weight at LDLT were 12.6 ± 2.0 years and 40.5 ± 9.9 kg, respectively. The graft type was left lobe in six patients, left + caudate lobe in seven patients, and posterior segment in one patient.
Results
The graft survival rates in SFSG and non-SFSG groups were 78.9 and 93.1 %, respectively (p = 0.045). In the univariate analysis, bleeding volume during LDLT were an independent risk factors for graft failure (p = 0.011). Graft failure was caused by sepsis in all three patients and occurred at a median of 70 postoperative days 70 (range 14–88 days). Among them, two cases showed high preoperative PELD/MELD score (PELD; 19.4 and MELD; 22, respectively).
Conclusions
Pediatric LDLT using SFSG had poor outcome and prognosis, especially when it accompanies the surgical infectious complications with preoperative high PELD/MELD scores.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Small-for-size syndrome (SFSS) was first described in 1999 and known mainly in the field of adult living-donor liver transplantation (LDLT) [1]. It occurs when the graft volume (GV) is too small to satisfy the recipients’ metabolic demand. The symptoms of SFSS are caused by functional impairment of the graft due to the small-for-size graft (SFSG) such as prolonged cholestasis, ascites, coagulopathy, and encephalopathy [2, 3]. In addition, a number of studies have shown that adult LDLT with SFSG is associated with poor prognosis [1, 4–8].
In the field of pediatric LDLT, the patients’ characteristics are different from those of adult LDLT patients [9]. However, SFSS has not been thoroughly discussed until now; some pediatric recipients in a later childhood are at risk of SFSS.
The purpose of this study was to analyze our experience with pediatric LDLT using SFSG and identify the risk factors of graft failure in order to establish a preoperative strategy for graft selection.
Patients and methods
Patients
Between May 2001 and December 2013, 245 LDLTs were performed at Jichi Medical University Hospital, Tochigi, Japan. In 14 of the 245 transplantations performed, SFSG were used.
The characteristics of the 14 patients are shown in Table 1. The original disease was biliary atresia in nine patients (64.3 %), Wilson disease in one, graft failure in one, ornithine transcarbamylase deficiency in one, congenital extrahepatic portosystemic shunt in one, and hepatoblastoma in one. The mean age and body weight of the patients at LDLT were 12.6 ± 2.0 years and 40.5 ± 9.9 kg, respectively. The graft type was left lobe in six patients (42.9 %), the left + caudate lobe in seven patients (50.0 %), and the posterior segment in one patient (7.1 %). SFSG was defined as a GV <40 % of the standard liver volume (SLV), and SLV was calculated using Urata’s formula [10]. The mean GV and GV/SLV were 331.1 ± 58.4 kg and 36.5 ± 2.5 %, respectively.
Graft selection and surgical procedures for LDLT
The type of donor hepatectomy was determined according to the recipient’s SLV and preoperative CT volumetry of the graft liver. In principle, we selected left lobe graft. If the GV/SLV of the left lobe graft was <40 %, we consider the selection of left and caudate lobe, right lobe or posterior segment graft. Routine graft hepatectomy was performed using intraoperative ultrasonic guidance. The donor biliary anatomy was evaluated using either intraoperative repeated real-time or preoperative magnetic resonance cholangiography. The allografts were preserved with University of Wisconsin solution (Viaspan). If necessary, graft hepatic vein venoplasty was performed on the back table.
For the recipient procedure, a Mercedes-Benz or transverse incision was created, and total hepatectomy was performed. In many recipients who had undergone total hepatectomy, the right, middle, and left hepatic veins were formed into a single orifice, which was then anastomosed end-to-end to the graft left hepatic vein, and the portal vein was reconstructed between the recipient right or left portal vein branch patch and the graft left portal vein. Hepatic artery reconstruction was performed using a microsurgical technique. Biliary reconstruction was performed using Roux-en-Y hepaticojejunostomy or duct-to-duct choledochocho-hepaticostomy. Intraoperative color Doppler ultrasonography was performed to assess the blood flow velocity and pattern after vascular reconstruction, and during abdominal wall closure.
Immunosuppressive therapy
Tacrolimus and methylprednisolone were used as the standard postoperative immunosuppression therapy regimen. The target trough levels of tacrolimus and methylprednisolone decreased gradually. Mycophenolate mofetil was used when more potent immunosuppression was required, for example, in ABO-incompatible recipients older than 5 years, in patients with steroid-resistant acute rejection episodes, and in those who developed liver dysfunction after the cessation of methylprednisolone therapy.
Statistical analysis
Data are expressed as median (range) and mean ± standard deviation values. Graft survival was calculated according to the Kaplan–Meier product-limited method. We compared the survival (n = 11) and non-survival groups (n = 3) using the Student t and Fisher exact tests. All the statistical analyses were performed using the StatView software package (SAS Institute, Cary, NC), and differences with p < 0.05 were considered as statistically significant.
Results
The median recipient operative time and amount of bleeding were median 20 h 3 min ± 6 h 1 min and 5321.8 ± 3888.6 mL, respectively.
The graft survival rates in the patients without SFSG (n = 231) and in those with SFSG (n = 14) were 93.1 and 78.6 %, respectively (p = 0.045; Fig. 1). In the SFSG group, we compared the characteristics between the survival (n = 11) and graft failure groups (n = 3; Table 2). Bleeding volume was larger in the graft failure group than in the survival group [9132 mL (7438–13,338) vs 2112 ml (700–9618), p = 0.011]. No significant differences were observed in the other factors. We plotted the relationship of GV/SLV and PELD/MELD score (Fig. 2), and it revealed that the extremely high PELD/MELD score with SFSG are higher risk of patient survival. In addition, to clarify how the relationship between preoperative PELD/MELD score and GV/SLV affects graft survival, we categorized the recipients older than 8 years into four groups based on the presence or absence of a SFSG and a PELD/MELD score >15 or not, and compared the graft survival rates (Table 3). A preoperative PELD/MELD score >15 is considered an indicator of an extremely high risk of graft failure in patients with a predictive SFSG.
The causes of graft failure were sepsis in all three recipients [bowel perforation (Case 3), acute peritonitis (Case 11), and cholangitis (Case 12)]. We performed liver biopsy in Case 11 and Case 12, and they did not show any findings of acute cellular rejection. Graft failure occurred after a median of 70 postoperative days (range 14–88 days).
To examine the impact of splenectomy and septic surgical complications, we examined the age matched 26 recipients who were older than 8 years at LDLT and absence of SFSG. The splenectomy was performed in eight patients (31.8 %) and septic surgical complications occurred in ten patients (38.5 %). These are not statistically different compared with the presence or absence of SFSG (p = 0.31 and p = 0.521, respectively). In five patients with absence of SFSG, splenectomy was performed and septic surgical complications occurred. Among them, one patient could not be rescued, but the four patients (80.0 %) were cured and alive now.
Discussion
In LDLT, the biggest problem due to SFSG is primary non-function derived from SFSS. Once SFSS occurs, the patient are suffer from much amount ascites due to portal hypertension, coagulopathy, and cholestasis and it may sometime result in graft failure. The SFSG was first defined Graft recipient weight ratio <0.8 % [1] and the definition is slightly differentiated based on the each institute now. In our institute, we use GV/SLV because the body surface area is more reliable especially in cases of obesity or skinny, and considered that the GV/SLV <40 % as a SFSG. In pediatric LDLT, SFSG is a relatively rare condition and it had not been discussed enough, and the strategy is not established until now. However, there actually exist many cases which could not be avoided using SFSG, especially when the recipient is teenagers and the mother is selected as the living donor. To avoid SFSG, a larger graft such as the right lobe graft, has been used as the standard strategy for adult-to-adult LDLT. Although LDLT using a right lobe graft can provide an adequate graft size to meet the metabolic demands of patients, it poses greater risks to the living donors [11, 12]. Therefore, the focus of the SFSG issue is now shifting from how to obtain a larger graft from the living donor to how to manage the use of a smaller graft to save the recipient, prioritizing donor safety [13].
The physiopathology of SFSS is complex, but portal hyperperfusion has been reported to be an important etiological factors of SFSS [14–20]. Nowadays, a portal vein (PV) pressure <15 mmHg is considered adequate to avoid SFSS [21]. To adequately control PV pressure and flow, portal inflow modulation techniques such as splenectomy [21–23], splenic artery ligation [22, 24, 25], or portosystemic shunting [26–31] has been considered. They are effective for temporary control of portal flow, however, they are accompanied by other problems such as overwhelming postsplenectomy infection [32], splenic abscess [33] or the potential risk of the portal flow steal phenomenon [21], respectively. Meanwhile, Ishizaki et al. [34] reported that portal flow modulation is not required in adult LDLT using SFSG. In our institute, as shown in this study, we considered SFSG as the cause of graft failure, and portal flow modulation is needed for patients with excessively high portal flow on LDLT findings and additional splenectomy. The adaptation of portal flow modulation was unclear, but no statistically significant differences were observed in the efficacy and risk of infection with splenectomy in this study.
In the field of pediatric LDLT, the most common indications are cholestatic liver disease represented by biliary atresia. These patients, especially in later childhood, require extremely difficult surgical procedures because of severe adhesion or portal hypertension, which are accompanied by much more bleeding and longer operative time in LDLT. In addition, they are at a higher risk of surgical infections such as cholangitis, abdominal abscess, gastrointestinal perforation, or pancreatic fistula after LDLT. SFSG causes spontaneous cholestasis and portal hypertension; therefore, SFSG with infectious complications in the early period after LDLT may lead to graft failure. In our experience, all the three graft failure patients with SFSG had biliary atresia and were derived from surgical abdominal infections, which resulted in progressive graft failure in the early period after LDLT. We have to recognize that surgical infections in the early phase after LDLT using SFSG are the life-threatening conditions. Therefore, biliary atresia patients with SFSG are at an extremely high risk of graft failure.
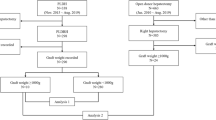
Sugawara et al. [35] reported that adult recipients with MELD scores >15 were at higher risk in LDLT using SFSG. They divided the criteria according to the presence or absence of SFSG, with a MELD score >15. In fact, adult recipients of LDLT using SFSG with high MELD scores are considered at high risk of graft failure [11]. Although the statistical analysis is difficult because of small number of cases, our clinical data support the strategy of graft selection according to a PELD/MELD score >15 in pediatric recipients. Based on this study, we show our strategy of preoperative graft selection in Fig. 3. We performed predictive CT-volumetry of the left lobe graft. If the PELD/MELD score of patients is <15, we considered that as sufficient basis to use SFSG. However, if the PELD/MELD score is >15, we have to change the graft to maintain the GV/SLV at >40 %. Then, we have to consider right lobe graft, living donor change, or whole-sized matched liver transplantation from deceased liver transplantation using whole-liver graft.
Our preoperative strategy of graft selection for the predictive SFSG. When the predictive left lobe graft volume allows for the use of a SFSG and the preoperative PELD/MELD score is >15, we have to consider using right lobe graft, posterior segment graft, change of donor or a whole-size matched liver transplantation from deceased donor
This study had limitation. The number of cases was small, and we could not find a significant difference in the multivariate analysis. In addition, we did not measure PV pressure in all the cases, and the impact of splenectomy performed as portal flow modulation was not evaluated. However, we believe that this study will help in the selection of the appropriate graft for pediatric recipients who need LDLT.
In conclusion, pediatric LDLT using SFSG is associated with poor outcome and prognosis, when it accompanies the surgical infectious complications in early period after LDLT. In high risk patients with higher PELD/MELD score and with surgical difficulties, using SFSG should be avoided and the graft should be changed to maintain the GV/SLV at >40 %.
Abbreviations
- LDLT:
-
Living-donor liver transplantation
- SFSS:
-
Small-for-size syndrome
- SFSG:
-
Small-for-size graft
- GV:
-
Graft volume
- SLV:
-
Standard liver volume
- MELD:
-
Model for end-stage liver disease
- PELD:
-
Pediatric end-stage liver disease
- PV:
-
Portal vein
References
Kiuchi T, Kasahara M, Uryuhara K, Inomata Y, Uemoto S, Asonuma K et al (1999) Impact of graft size mismatching on graft prognosis in liver transplantation from living donors. Transplantation 67:321–327
Ikegami T, Shimada M, Imura S, Arakawa Y, Nii A, Morine Y et al (2008) Current concept of small-for-size grafts in living donor liver transplantation. Surg Today 38:971–982
Dahm F, Georgiev P, Clavien PA (2005) Small-for-size syndrome after partial liver transplantation: definition, mechanisms of disease and clinical implications. Am J Transplant 5:2605–2610
Sugawara Y, Makuuchi M, Takayama T, Imamura H, Dowaki S, Mizuta K et al (2001) Small-for-size grafts in living-related liver transplantation. J Am Coll Surg 192:510–513
Fan ST, Lo CM, Liu CL, Yong BH, Wong J (2003) Determinants of hospital mortality of adult recipients of right lobe live donor liver transplantation. Ann Surg 238:864–869 (discussion 869–870)
Shimada M, Ijichi H, Yonemura Y, Harada N, Shiotani S, Ninomiya M et al (2004) Is graft size a major risk factor in living-donor adult liver transplantation? Transpl Int 17:310–316
Tsunematsu I, Ogura Y, Inoue K, Koizumi A, Tanigawa N, Tanaka K (2006) Quantitative survival model for short-term survival after adult-to-adult living donor liver transplantation. Liver Transpl 12:904–911
Nishizaki T, Ikegami T, Hiroshige S, Hashimoto K, Uchiyama H, Yoshizumi T et al (2001) Small graft for living donor liver transplantation. Ann Surg 233:575–580
Kasahara M, Umeshita K, Inomata Y, Uemoto S (2013) Japanese Liver Transplantation Society Long-term outcomes of pediatric living donor liver transplantation in Japan: an analysis of more than 2200 cases listed in the registry of the Japanese Liver Transplantation Society. Am J Transplant 13(7):1830–1839
Urata K, Kawasaki S, Matsunami H, Hashikura Y, Ikegami T, Ishizone S et al (1995) Calculation of child and adult standard liver volume for liver transplantation. Hepatology 21:1317–1321
Lei JY, Wang WT, Yan LN (2012) Risk factors of SFSS in adult-to-adult living donor liver transplantation using the right liver: a single-center analysis of 217 cases. Hepatogastroenterology 59:1491–1497
Chan SC, Fan ST, Chok KS, Sharr WW, Dai WC, Fung JY et al (2012) Increasing the recipient benefit/donor risk ratio by lowering the graft size requirement for living donor liver transplantation. Liver Transpl 18:1078–1082
Roll GR, Parekh JR, Parker WF, Siegler M, Pomfret EA, Ascher NL et al (2013) Left hepatectomy versus right hepatectomy for living donor liver transplantation: shifting the risk from the donor to the recipient. Liver Transpl 19:472–481
Demetris AJ, Kelly DM, Eghtesad B, Fontes P, Wallis Marsh J, Tom K et al (2006) Pathophysiologic observations and histopathologic recognition of the portal hyperperfusion or small-for-size syndrome. Am J Surg Pathol 30:986–993
Man K, Lo CM, Ng IO, Wong YC, Qin LF, Fan ST et al (2001) Liver transplantation in rats using small-for-size grafts: a study of hemodynamic and morphological changes. Arch Surg 136:280–285
Fondevila C, Hessheimer AJ, Taura P, Sanchez O, Calatayud D, de Riva N et al (2010) Portal hyperperfusion: mechanism of injury and stimulus for regeneration in porcine small-forsize transplantation. Liver Transpl 16:364–374
Asakura T, Ohkohchi N, Orii T, Koyamada N, Tsukamoto S, Sato M et al (2003) Portal vein pressure is the key for successful liver transplantation of an extremely small graft in the pig model. Transpl Int 16:376–382
Yagi S, Iida T, Hori T, Taniguchi K, Nagahama M, Isaji S et al (2012) Effect of portal haemodynamics on liver graft and intestinal mucosa after small-for-size liver transplantation in swine. Eur Surg Res 48:163–170
Troisi R, Cammu G, Militerno G, De Baerdemaeker L, Decruyenaere J, Hoste E et al (2003) Modulation of portal graft inflow: a necessity in adult living-donor liver transplantation? Ann Surg 237:429–436
Hori T, Yagi S, Iida T, Taniguchi K, Yamagiwa K, Yamamoto C et al (2007) Stability of cirrhotic systemic hemodynamics ensures sufficient splanchnic blood flow after living-donor liver transplantation in adult recipients with liver cirrhosis. World J Gastroenterol 13:5918–5925
Ogura Y, Hori T, El Moghazy WM, Yoshizawa A, Oike F, Mori A et al (2010) Portal pressure <15 mm Hg is a key for successful adult living donor liver transplantation utilizing smaller grafts than before. Liver Transpl 16:718–728
Ito T, Kiuchi T, Yamamoto H, Oike F, Ogura Y, Fujimoto Y et al (2003) Changes in portal venous pressure in the early phase after living donor liver transplantation: pathogenesis and clinical implications. Transplantation 75:1313–1317
Cheng YF, Huang TL, Chen TY, Concejero A, Tsang LL, Wang CC et al (2006) Liver graft-to-recipient spleen size ratio as a novel predictor of portal hyperperfusion syndrome in living donor liver transplantation. Am J Transplant 6:2994–2999
Troisi R, de Hemptinne B (2003) Clinical relevance of adapting portal vein flow in living donor liver transplantation in adult patients. Liver Transpl 9:S36–S41
Umeda Y, Yagi T, Sadamori H, Matsukawa H, Matsuda H, Shinoura S et al (2008) Effects of prophylactic splenic artery modulation on portal overperfusion and liver regeneration in small-for-size graft. Transplantation 86:673–680
Boillot O, Delafosse B, Mėhet I, Boucaud C, Pouyet M (2002) Small-for-size partial liver graft in an adult recipient: a new transplant technique. Lancet 359:406–407
Masetti M, Siniscalchi A, De Pietri L, Braglia V, Benedetto F, Di Cautero N et al (2004) Living donor liver transplantation with left liver graft. Am J Transplant 4:1713–1716
Takada Y, Ueda M, Ishikawa Y, Fujimoto Y, Miyauchi H, Ogura Y et al (2004) End-to-side portocaval shunting for a small-for-size graft in living donor liver transplantation. Liver Transpl 10:807–810
Troisi R, Ricciardi S, Smeets P, Petrovic M, Van Maele G, Colle I et al (2005) Effects of hemi-portocaval shunts for inflow modulation on the outcome of small-for-size grafts in living donor liver transplantation. Am J Transplant 5:1397–1404
Yamada T, Tanaka K, Uryuhara K, Ito K, Takada Y, Uemoto S (2008) Selective hemi-portocaval shunt based on portal vein pressure for small-for-size graft in adult living donor liver transplantation. Am J Transplant 8:847–853
Botha JF, Langnas AN, Campos BD, Grant WJ, Freise CE, Ascher NL et al (2010) Left lobe adult-to-adult living donor liver transplantation: small grafts and hemiportocaval shunts in the prevention of small-for-size syndrome. Liver Transpl 16:649–657
Takeda K, Morioka D, Kumamoto T, Matsuo K, Tanaka K, Endo I et al (2009) Survival case of ABO-incompatible liver transplantation complicated with severe preoperative infection and subsequent overwhelming postsplenectomy infection. Transplant Proc 41:3941–3944
Balci D, Taner B, Dayangac M, Akin B, Yaprak O, Duran C et al (2008) Splenic abscess after splenic artery ligation in living donor liver transplantation: a case report. Transplant Proc 40:1786–1788
Ishizaki Y, Kawasaki S, Sugo H, Yoshimoto J, Fujiwara N, Imamura H (2012) Left lobe adult-to-adult living donor liver transplantation: Should portal inflow modulation be added? Liver Transpl 18:305–314
Sugawara Y, Makuuchi M, Kaneko J, Kokudo N (2003) MELD score for selection of patients to receive a left liver graft. Transplantation 75:573–574
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No financial support and commercial sponsorship.
Rights and permissions
About this article
Cite this article
Yamada, N., Sanada, Y., Hirata, Y. et al. The outcomes of pediatric living donor liver transplantation using small-for-size grafts: experience of a single institute. Pediatr Surg Int 32, 363–368 (2016). https://doi.org/10.1007/s00383-016-3859-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3859-4