Abstract
Introduction
Gunshot penetrating brain injury is common in military conflict area and in urban violence area, but similar incident in pediatric population is rarely reported.
Case report
We reported three cases of gunshot penetrating brain injury in children. Two patients had a good recovery after surgery and no significant deficit on his neurologic function, the other patient was not having surgery due to the severity of the condition.
Conclusions
We suggest surgery should be performed immediately to prevent further injury and refractory brain edema due to the injury, in any case of penetrating brain injury; a good prognosis can be achieved from early surgery and with appropriate post-operative treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gunshot wounds to the head are the most lethal of penetrating brain injuries, and many do not survive after the injury. Harvey Cushing was a pioneer in the management of penetrating head injuries, and he popularized the craniectomy, debridement and closure for treating penetrating brain injury in World War I, although later the method was replaced by osteoplastic craniotomy in World War II by Cairns [1, 2]. The mortality rate among survivors of gunshot injury to the head is extremely high. Kaufman estimated that more than 90% of people experiencing gunshot injury to the head eventually died, two thirds of these died at the scene [1, 3], mostly because of respiratory arrest and circulatory arrest which followed within minutes [4,5,6].
GCS score of the patient on admission may predict the outcome of the patient; there was an 85% mortality for those with GCS less than 7 and all those with fixed pupils. However, the prognosis and survival may be more favorable in patients with GCS more than 12 [7]. In gunshot penetrating brain injury, aggressive resuscitation and debridement may benefit the survival rates and the outcome [8, 9]. Gunshot penetrating brain injury is common in military conflict area and urban violence area. Mostly, victims vary from teenagers to adult population; the incident of gunshot injury to the head in pediatric case is rarely reported in the literature. Here, we reported three cases of gunshot injury to the head in pediatric patients. The clinical features, treatment, and outcome were reviewed.
Case report
Case 1
A 6-year-old female child was admitted to our hospital due to gunshot injury. The missile has entered from the angulus oculi medialis and remained at the occipital lobe (Fig. 1a–b). The patient was referred to local hospital, head CT revealed hemorrhage on left frontal lobe, basal ganglia and corona radiate. No special treatment was given at that time. Later, patient’s consciousness gradually became somnolence and she was referred to our hospital for further treatment. On admission patient had lack of movement on right extremities. We performed left occipital craniotomy to the patient. The dura was quite rigid and tense. After dural opening, massive subdural hemorrhage was seen and some devitalized tissue was spilled out. We debrided the devitalized tissue and removed the missile. After debridement and careful hemostatic, we applied tension reduced suture and fixed the defect with artifical dura. Due to the local severe brain tissue edema, we did not place back the bone flap. Postoperatively, we gave antibiotic, anti-seizure, and symptomatic treatment post-operation. Post-operative head CT and MRI showed no post-operative hematoma (Fig. 1c–f). The postoperative course was uneventful and the patient was discharge later.
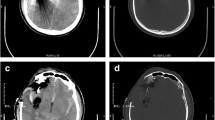
CT scan of the gunshot penetrating brain injury in case 1, (a–b) the missile was enter from the angulus oculi medialis and remained at the occipital lobe. c, f Post-operative CT and MRI scan showed removal of the missile and no post-operative hematoma was seen. d–e Post-operatively contusion with slight hemorrhage on right frontal lobe, basal ganglia and corona radiate and occipital lobe can be seen along the missile track
Case 2
A 7-year-old male child was admitted to our hospital due to a bullet-steel penetrating the head. On admission, the patient was in coma state. Physical examination revealed weak spontaneous respiration and dilated pupil with no pupillary reflex. Head CT showed a foreign matter in the right frontal lobe, right frontotemporoparietal subdural hematoma, diffuse subarachnoid hemorrhage, intraventricular hematoma and multiple contusion and laceration (Fig. 2a–d). Due to the severity of the condition, surgery was not indicated and we gave hemostatic agent, fluid infusion, mannitol and symptomatic treatment. But later, patient’s family gave up treatment and patient died due to deterioration of the disease.
Case 3
A 2-year-old male child was admitted to our hospital due to gunshot injury. The patient was in somnolence state; all vital signs were stable during admission. Head CT result showed subdural hemorrhage, and the hematoma on parietal temporal area increased slightly compared with the previous CT result (Fig. 3a–d). We performed a parietooccipital craniotomy to the patient. The intracranial pressure was high, and the brain enveloped by the dura was quite rigid and some devitalized tissue spilled out from the entry site. The injured lesion at the entry site revealed massive subdural hemorrhage. We debrided the devitalized tissue, removed the bone fragment and debrided the missile track. After debridement and careful hemostatic, we placed a drainage tube in the cavity left and applied tension reduced suture to the dura. We placed back the bone flap and used prolene to fix the bone flap. Postoperatively, the patient gradually regained his consciousness. We gave antibiotic, anti-seizure, and symptomatic treatment post-operation. Post-operative head CT showed bulk removal of the hematoma on the parietal lobe and slight increase of hematoma in the temporal area (Fig. 3e–f), but the patient’s condition was quite stable, so we continued to observe. Two days later, we re-examined the head CT and there was no volume change of the hematoma in the temporal area, so no particular treatment was given afterward. The patient gradually recovered and discharged from our hospital 1 week later without any neurological deficit.
CT scan of the gunshot penetrating brain injury in case 3, a showed description of the missile trajectory, b the missile was located near the masticatory muscle. c, d The entry site was located at parietal area near the functional area. Preoperative CT scan showed intracranial hematoma at parietal and temporal areas accompanied with diffused subdural hemorrhage; there were some bone fragments inside the hematoma. e, f Head CT scan showed bulk removal of the hematoma and slight increase of the hematoma at the temporal area
Discussion
Gunshot injury is the most lethal in penetrating brain injury, with reported survival rates on only 7 to 15%, and another study by Bellal et al. reported a survival rates of 10 to 15% [8, 10]. Gunshot injury to the head can cause cardiac and respiratory arrest; the pathophysiology mechanism of fatal apnea in penetrating brain injury is still unclear. Study with experimental animal models showed that a direct function of the energy deposited by the missile may affect the respiratory neurons of the medullary respiratory centre [5]. However, there is also evidence showing that the low cardiac output leading to a decrease in cerebral perfusion causes the damage in respiratory neurons [11]. Another conclusion from other study said that the mechanism might be due to the pressure to brainstem in acute stage caused by cerebral swelling [12]. One patient in our case had a diffuse brain swelling; we consider that this mechanism was to be the probable cause of respiratory dysfunction in this patient.
Surgery remains to be the first initial treatment for gunshot injury to the head; however, the decision of surgery should be based on the patient’s GCS status on admission. Grahm et al. [13] recommended immediate surgery for patients with GCS more than 8 and patients with an operable hematoma; patient with GCS of 3 to 5 after resuscitation was not a candidate for surgical treatment. Cavaliere and Carey [4, 14] recommended surgery on those patients with GCS more than 6, even though these patients have a 50% mortality. On the contrary, there were some authors recommending a selective policy for surgery in patients with GCS 3 to 5. Levy et al. [15] evaluated that patient with GCS 3 to 5 may have a better survival with surgery, but the outcomes are generally poor [9, 16]. The GCS in our two patients who undergone operation was more than 8 during admission and both were with an operable hematoma. One patient in our case had GCS of 3 accompany with respiratory dysfunction. Surgery is not recommended for this patient.
The surgical principles of gunshot penetration brain injury are to debride devitalized tissue, evacuate hematomas, and remove accessible missile or bone fragments [16]. Stone et al. [9] advise higher aggressiveness on debridement of devitalized tissue to reduce edema. Moreover, the timing of surgery in gunshot injury is important, not only can increase the survival rate, but early surgery may also decrease postoperative complication, such as infection, which is more likely to happen with the presence of retained bone fragment [17]. Consistent to that, we immediately performed the surgery and aggressively debrided and removed the local hematoma and partial brain tissue surrounding the missile track. Intensive postoperative treatments are crucial to improve post-operative morbidity and mortality, including monitoring of remaining hematoma or recurrence of the hematoma. Moreover, antibiotics and anticonvulsant drugs are recommended, although the use of antibiotics as a prophylaxis treatment is still a controversy. Many authors recommend the course of antibiotics for 10 to 14 days and anticonvulsant drugs, such as phenytoin or phenobarbital, for at least 6–12 months [18]. We used phenobarbitol postoperatively, and after the patient could consume oral food, we used oral carbamazepine as substitute. We suggested the patient to take oral carbamazepine for at least 3 months.
The prognosis of the gunshot injury to the head may depend on the patient’s conditions on admission, such as GCS status, papillary reaction, absence of bihemispheric injury with ventricular involvement, and absence of subarachnoid hemorrhage. The outcome for those who survive from gunshot injury varied; the combination of good recovery and moderate disability ranged from 63 to 92% [13, 18,19,20]. Those who survive from gunshot injury often have disability such as hemiparesis, blindness, and seizures [10, 21]. The mood, cognitive, and intelligence may also be affected, but they correlate with the lesion sites and the amount of brain lost, and children younger than 5 years tend to be affected more on the intelligent function, compared to older children and adult population [22, 23]. Other complications such epilepsy, vascular injuries, and CSF leak may occur in some cases [24, 25]. In our presented case, the postoperative course was uneventful. One patient was recovered with no neurological deficit; the other patient was left with neurological deficit due to injury caused by the missile in the basal ganglia.
Conclusions
Gunshot injury is the most lethal of penetrating brain injuries, with high mortality rate; this kind of injury is rarely reported in pediatric population. The outcome may depend on the severity of the injury, but early management and intensive postoperative treatment can increase survival rate and reduce complications.
References
Kaufman HH (1993) Civilian gunshot wounds to the head. Neurosurgery 32:962–964
Lepore FE (1994) Harvey Cushing, Gordon Holmes, and the neurological lessons of World War I. Arch Neurol 51:711–722
Rish BL, Dillon JD, Caveness WF, Mohr JP, Kistler JP, Weiss GH (1980) Evolution of craniotomy as a debridement technique for penetrating craniocerebral injuries. J Neurosurg 53:772–775
Cavaliere R, Cavenago L, Siccardi D, Viale GL (1988) Gunshot wounds of the brain in civilians. Acta Neurochir 94:133–136
Kordestani RK, Martin NA, McBride DQ (1995) Cerebral hemodynamic disturbances following penetrating craniocerebral injury and their influence on outcome. Neurosurg Clin N Am 6:657–667
Siccardi D, Cavaliere R, Pau A, Lubinu F, Turtas S, Viale GL (1991) Penetrating craniocerebral missile injuries in civilians: a retrospective analysis of 314 cases. Surg Neurol 35:455–460
Suddaby L, Weir B, Forsyth C (1987) The management of .22 caliber gunshot wounds of the brain: a review of 49 cases. Can J Neurol Sci 14:268–272
Joseph B, Aziz H, Pandit V, Kulvatunyou N, O'Keeffe T, Wynne J, Tang A, Friese RS, Rhee P (2014) Improving survival rates after civilian gunshot wounds to the brain. J Am Coll Surg 218:58–65
Stone JL, Lichtor T, Fitzgerald LF (1995) Gunshot wounds to the head in civilian practice. Neurosurgery 37:1104–1110
Selden BS, Goodman JM, Cordell W, Rodman GH Jr, Schnitzer PG (1988) Outcome of self-inflicted gunshot wounds of the brain. Ann Emerg Med 17:247–253
Carey ME (1995) Experimental missile wounding of the brain. Neurosurg Clin N Am 6:629–642
Sullivan HG, Martinez J, Becker DP, Miller JD, Griffith R, Wist AO (1976) Fluid-percussion model of mechanical brain injury in the cat. J Neurosurg 45:521–534
Grahm TW, Williams FC Jr, Harrington T, Spetzler RF (1990) Civilian gunshot wounds to the head: a prospective study. Neurosurgery 27:696–700
Carey ME (2000) An overview of civilian brain wounds from bullets: 1963–1996. Neurosurg Quart 10:1–41
Levy ML, Masri LS, Lavine S, Apuzzo ML (1994) Outcome prediction after penetrating craniocerebral injury in a civilian population: aggressive surgical management in patients with admission Glasgow Coma Scale scores of 3, 4, or 5. Neurosurgery 35:77–84
Kaufman HH, Makela ME, Lee KF, Haid RW Jr, Gildenberg PL (1986) Gunshot wounds to the head: a perspective. Neurosurgery 18:689–695
Taha JM, Haddad FS, Brown JA (1991) Intracranial infection after missile injuries to the brain: report of 30 cases from the Lebanese conflict. Neurosurgery 29:864–868
Kaufman HH (1995) Care and variations in the care of patients with gunshot wounds to the brain. Neurosurg Clin N Am 6:727–739
Hernesniemi J (1979) Penetrating craniocerebral gunshot wounds in civilians. Acta Neurochir 49:199–205
Nagib MG, Rockswold GL, Sherman RS, Lagaard MW (1986) Civilian gunshot wounds to the brain: prognosis and management. Neurosurgery 18:533–537
Kennedy F, Gonzalez P, Dang C, Fleming A, Sterling-Scott R (1993) The Glasgow coma scale and prognosis in gunshot wounds to the brain. J Trauma 35:75–77
Ewing-Cobbs L, Thompson NM, Miner ME, Fletcher JM (1994) Gunshot wounds to the brain in children and adolescents: age and neurobehavioral development. Neurosurgery 35:225–233
Salazar AM, Schwab K, Grafman JH (1995) Penetrating injuries in the Vietnam war. Traumatic unconsciousness, epilepsy, and psychosocial outcome. Neurosurg Clin N Am 6:715–726
Aarabi B (1989) Causes of infections in penetrating head wounds in the Iran-Iraq war. Neurosurgery 25:923–926
Aarabi B (1995) Management of traumatic aneurysms caused by high-velocity missile head wounds. Neurosurg Clin N Am 6:775–797
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no declaration of interest.
Rights and permissions
About this article
Cite this article
Liu, R., Liu, Y., Liu, W. et al. Gunshot penetrating brain injury in children: report of three cases with review of the literature. Childs Nerv Syst 34, 1459–1463 (2018). https://doi.org/10.1007/s00381-018-3858-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3858-y