Abstract
Introduction
Intradural transection of the filum terminale (FTI) is often used to treat tethered cord syndrome. Recently, some have proposed that the extradural part of the filum terminale (FTE) can be sectioned with equal results but with fewer complications. Therefore, the present cadaveric study aimed to evaluate the anatomical foundation of such procedures.
Methods
A posterior lumbosacral approach was performed on five fresh-frozen cadaveric specimens to expose both the FTI and FTE. Tension was then applied to the FTE and observations and measurements made of any movement of the FTI. Other morphological measurements (e.g., length, diameter) of the FTI and FTE were also made.
Results
Although very minimal movement of the FTI was seen in the majority of specimens following tension on the FTE, no specimen was found to have more cranial movement of the conus medullaris or cauda equina. The mean length and diameter of the FTI was 52.2 and 0.38 mm, respectively. The mean length and diameter of the FTE was 77 and 0.60 mm, respectively. The force necessary to move the FTI with tension applied to the FTE had a mean of 0.03 N. The average distance that the FTI moved with distal FTE tension was 1.33 mm. All specimens had a thecal sac that terminated at the S2 vertebral level. And no specimen had a low-lying conus medullaris, cutaneous stigmata of occult spinal dysraphism, or grossly visible adipose tissue in either the FTI or FTE.
Conclusions
Based on our studies, tension placed on the FTE has very little effect on the FTI and no obvious effect on the conus medullaris or cauda equina. Therefore, isolated transection of the FTE for a patient with tethered cord syndrome is unlikely to have significant effect. To our knowledge, this is the first study to quantitate the distal forces needed on the FTE to move the FTI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tethered cord syndrome (TCS) is a form of occult spinal dysraphism often characterized by a low-lying conus medullaris. Clinically, a wide variety of neurologic symptoms has been associated with TCS including an abnormal gait, club foot, pain, weakness, and often issues related to dysfunction of the conus medullaris (e.g., urinary incontinence) [1, 7, 9, 10, 17]. In conjunction with clinical appraisals, the vast majority of TCS diagnoses are made by using MRI [6, 21] in order to visualize the position of the conus medullaris and many times after cutaneous stigmata are observed in the midline lumbar region [20, 23].
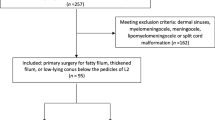
The filum terminale (FT), an extension of the pia mater at the distal end of the spinal cord (SC), runs from the CM to the first segment of the coccyx (Fig. 1) [18, 19]. The FTI runs within the dura mater and carries with it a filar vein and artery [4, 14] before fusing with the distal end of the thecal sac, emerging as the FTE. The FTE then travels caudally through the sacral hiatus before terminating on the dorsal coccyx [19].
Schematic drawing (left) of the FTI (brown) and FTE (green). Cadaveric dissection (right) with FTI colored yellow and most proximal FTE (purple) and most distal FTE (green). The distal dorsal elements of the sacrum are still intact to illustrate the sacral hiatus and the terminal thecal sac is opened and tented laterally with silk sutures
A thickened FT may anchor the SC during embryonic development [2, 7, 23]. Once the embryo reaches approximately 30 mm in length, the vertebral column begins to lengthen more rapidly than the spinal cord, causing undue mechanical tension to be exerted on the cord [16]. This tension leads to metabolic stress and hypoxia in spinal cord tissue, generating the symptoms associated with TCS [9, 10, 23]. TCS was first described by Garceau in 1953 [3], who dubbed it “filum terminale syndrome.” Classically, the FT is one of the anatomical structures most at risk of being tethered in cases of TCS, especially when laden with adipose tissue and greater than 2 mm in diameter.
In the event of a symptomatic tethered FTI, standard surgical protocol involves the release of the FT [15]. Traditional surgical approaches to the FTI involve a laminectomy at the L5 or S1 level. The act of removing bone and opening the dura mater during these procedures can often lead to the formation of scar tissue or CSF leak post-operatively. Therefore, a variety of minimally invasive procedures have been explored as potential alternatives to traditional TCS surgery [5].
Recently, a few reports have suggested that in certain cases of TCS, release of the FTE alone may lead to a significant amelioration of patient symptoms [11, 15, 22]. In order to establish a wider set of indications for release of the FTE, a consistent mechanical relationship between the FTI and the FTE must be established. In this study, the mechanical relationship between the FTI and FTE was explored in fresh cadavers in order to analyze whether or not release of the FTE may be a viable and minimally invasive form of treatment for TCS.
Materials and methods
A posterior lumbosacral approach was performed on five fresh-frozen cadaveric specimens to expose both the FTI and FTE. The cadaveric specimens studied ranged in age from 59 to 79 at the time of death and included both sexes (three males/two females). In the prone position, laminectomies of the entire lumbosacral region were performed with bone rongeurs. The terminal portion of the thecal sac was then opened with dissecting scissors and the FTI identified and followed distally out of the thecal sac as it became the FTE and attached through the sacral hiatus onto the dorsal coccyx. A silk suture was then tied to the FTE. Then, it was placed under tension using a hand-triggered tensometer (Lyman, Middletown, CT, USA) and the force needed to produce movement of the FTI recorded. Other measurements (all made with a microcaliper (Mitsutoyo, Kanagawa, Japan) with a resolution of 0.01 mm and accuracy of ± 0.025 mm recorded during the study included total distance moved by FTI during tension, length of the FTI and FTE, and diameter of the FTI and FTE. The approximate ending of the thecal sac was also recorded for each cadaveric specimen.
Results
Although very minimal movement of the FTI was seen in the majority of specimens following tension on the FTE, no specimen was found to have more cranial movement of the conus medullaris or cauda equina. No gross adipose tissue was found in any FTI or FTE. The mean length and diameter of the FTI was 52.2 mm (range 41–50 mm) and 0.38 mm (range 0.10–0.76 mm), respectively. The mean length and diameter of the FTE was 77 mm (range 66–88.3 mm) and 0.60 mm (range 0.28–0.87 mm), respectively. The force necessary to move the FTI with tension applied to the FTE ranged from 0.014 to 0.06 N with a mean of 0.03 N. The average distance that the FTI moved with distal FTE tension was 1.33 mm (range 0–3.49 mm). All specimens had a thecal sac that terminated at the S2 vertebral level. No specimen had signs of previous surgery or gross pathology in the regions examined. No specimen was found to have a low-lying conus medullaris or cutaneous stigmata of occult spinal dysraphism. The FTE was very adherent and difficult to correctly identify without full exposure of the dorsal elements of the sacrum and confirmation of this structure up to the termination of the cul de sac of the spinal dura mater.
Discussion
We found that grossly visible motion of the FTI was observed when the FTE had distal tension applied to it. However, this movement was very minimal and sometimes, there was no movement (Fig. 2). Traditionally, the surgical approach for TCS includes lumbar laminotomy, lumbar laminectomy, or S1 laminectomy. However, some have reported that TCS symptoms can be relieved with minimally invasive extradural transection of the FTE [15, 22] through the sacral hiatus with or without endoscopy [11, 15]. Advantages of a minimally invasive procedure include lower risk of retethering, shortened operating time, and lower post-operative complications. Additionally, although caudal epidural anesthesia via the sacral hiatus usually carries minimal risks [8, 12, 13], correctly identifying the FTE at the sacral hiatus is very difficult and in our study, required confirmation by removing all of the dorsal elements of the sacrum and confirming its proximal attachment to the spinal dura cul de sac.
For example, recently, Veronesi et al. [22] described a single case in which a trans-hiatal approach was used in order to section the FTE of a patient presenting with pain and progressive gait disruption. This procedure involved neither bone removal nor violation of the dural sac. Evaluation of the patient 3 months post-operatively showed that symptoms had improved significantly [22]. In a larger study, Royo-Salvador et al. [15] reported mostly adult patients with tethered cord syndrome of which, nine patients underwent filum terminale section outside of the dural sac. Although their paper made it difficult to discern which nine patients had an extradural procedure, all patients were reported to have improvement of their preoperative symptoms.
Our study found that motion of the FTI was present in four of the five specimens after tensing the FTE. However, the movement of the FTI was very minimal. Moreover, in order to verify the anatomy of the FTE, removal of all of the dorsal sacral elements is necessary.
Conclusion
To our knowledge, this is the first study to quantitate the distal forces needed on the FTE to move the FTI. Based on our cadaveric findings, extradural transection of the filum terminale is probably inappropriate.
References
Arya NG, Weissbart SJ (2017) Central control of micturition in women: brain-bladder pathways in continence and urgency urinary incontinence. Clin Anat 30:373–384
De Vloo P, Monea AG, Sciot R et al (2016) The filum terminale: a cadaver atudy of anatomy, histology, and elastic properties. World Neurosurg 90:565–573
Garceau GJ (1953) The filum terminale syndrome (the cord-traction syndrome). J Bone Joint Surg Am 35–A:711–6
Griessenauer CJ, Raborn J, Foreman P, Shoja MM, Loukas M, Tubbs RS (2015) Venous drainage of the spine and spinal cord: a comprehensive review of its history, embryology, anatomy, physiology, and pathology. Clin Anat 28:75–87
Hayashi T, Kimiwada T, Kohama M et al (2018) Minimally invasive surgical approach to filum lipoma. Neurol Med Chir (Tokyo) 58:132–137
Hendrix P, Griessenauer CJ, Cohen-Adad J, Rajasekaran S, Cauley KA, Shoja MM, Pezeshk P, Tubbs RS (2015) Spinal diffusion tensor imaging: a comprehensive review with emphasis on spinal cord anatomy and clinical applications. Clin Anat 28:88–95
Hertzler DA, DePowell JJ, Stevenson CB, Mangano FT (2010) Tethered cord syndrome: a review of the literature from embryology to adult presentation. Neurosurg Focus 29:E1
Maddali P, Moisi M, Page J, Chamiraju P, Fisahn C, Oskouian R, Tubbs RS (2017) Anatomical complications of epidural anesthesia: a comprehensive review. Clin Anat 30:342–346
Mortazavi MM, Harmon OA, Adeeb N, Deep A, Tubbs RS (2015) Treatment of spinal cord injury: a review of engineering using neural and mesenchymal stem cells. Clin Anat 28:37–44
Mortazavi MM, Verma K, Harmon OA, Griessenauer CJ, Adeeb N, Theodore N, Tubbs RS (2015) The microanatomy of spinal cord injury: a review. Clin Anat 28:27–36
Mourgela S, Anagnostopoulou S, Sakellaropoulos A, Koulousakis A, Warnke JP (2008) Sectioning of filum terminale externum using a rigid endoscope through the sacral hiatus. Cadaver study. J Neurosurg Sci 52:71–74
Prats-Galino A, Reina MA, Mavar Haramija M, Puigdellivol-Sánchez A, Juanes Méndez JA, De Andrés JA (2015) 3D interactive model of lumbar spinal structures of anesthetic interest. Clin Anat 28:205–212
Puigdellívol-Sánchez A, Reina MA, Sala-Blanch X, Pomés-Talló J, Prats-Galino A (2016) Pythagoras and cosines: the skin-dural sac distance and optimal angles in paramedian spinal anesthesia. Clin Anat 29:1046–1052
Rojas S, Ortega M, Rodríguez-Baeza A (2018) Vascular configurations of anastomotic basket of conus medullaris in human spinal cord. Clin Anat 31:441–448
Royo-Salvador MB, Solé-Llenas J, Doménech JM, Gonzàlez-Adrio R (2005) Results of the section of the filum terminale in 20 patients with syringomyelia, scoliosis and Chiari malformation. Acta Neurochir 147:515–523
Saker E, Henry BM, Tomaszewski KA, Loukas M, Iwanaga J, Oskouian RJ, Tubbs RS (2017) The filum terminale internum and externum: a comprehensive review. J Clin Neurosci 40:6–13
Shah AP, Mevcha A, Wilby D, Alatsatianos A, Hardman JC, Jacques S, Wilton JC (2014) Continence and micturition: an anatomical basis. Clin Anat 27:1275–1283
Tarlov IM (1938) Structure of the filum terminale. Arch Neurol Psych 40:1–17
Tubbs RS, Murphy RL, Kelly DR, Lott R, Salter EG, Oakes WJ (2005) The filum terminale externum. J Neurosurg Spine 3:149–152
Tubbs RS, Malefant J, Loukas M, Jerry Oakes W, Oskouian RJ, Fries FN (2016) Enigmatic human tails: a review of their history, embryology, classification, and clinical manifestations. Clin Anat 29:430–438
Van Schoor AN, Bosman MC, Bosenberg AT (2015) Descriptive study of the differences in the level of the conus medullaris in four different age groups. Clin Anat 28:638–644
Veronesi V, Sacco C, Mastronicola C, Staffa G (2017) Transhiatal approach to filum terminale externum sectioning in adult patient with tethered cord syndrome: case report. Oper Neurosurg
Yamada S (2004) Tethered cord syndrome in adults and children. Neurol Res 26:717–718
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report.
Rights and permissions
About this article
Cite this article
Patel, M., Vetter, M., Simonds, E. et al. Mechanical relationship of filum terminale externum and filum terminale internum: is it possible to detether the spinal cord extradurally?. Childs Nerv Syst 34, 1767–1770 (2018). https://doi.org/10.1007/s00381-018-3837-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3837-3