Abstract
Purpose
Surgical revascularization for pediatric moyamoya disease improves cerebral blood flow (CBF) and consequently may prevent further ischemic events. However, the timing of the treatment is controversial especially for patients with no ischemic symptom and normal CBF. The purpose of this case report is to inform and infer the surgical treatment timing for pediatric moyamoya disease patients.
Case report
A 10-year-old female patient with unilateral moyamoya disease complaining of only headache as a symptom and whose Suzuki stage was II or in transition to III by angiography and CBF was almost normal was admitted to Tokyo Women’s Medical University Hospital. We performed superficial temporal artery-middle cerebral artery (STA-MCA) double anastomoses for the patient because we estimated her headache was derived from low perfusion in the brain. STA-MCA bypass surgery was not only effective for relief of her severe headache but also valid for her cerebral perfusion. Her angiography showed much supply from external carotid artery to intracranial arteries via bypass grafts in 7 months.
Conclusion
Our case showed early surgical treatment was beneficial for relief of severe headache even for early staged pediatric moyamoya disease patients by improving perfusion pressure and cerebral circulation.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Moyamoya disease is a progressive occlusive cerebrovascular disease characterized by bilateral stenosis of the internal carotid arteries at the level of their terminal bifurcation together with abnormalities of the anterior and middle cerebral arteries and the development of extensive collateral vessels (moyamoya vessels) [17].
In general, pediatric patients with moyamoya disease present with ischemic symptoms [17]. Surgical revascularization to the ischemic brain is a recommended treatment option [2], which reduces the incidence of subsequent ischemic stroke and risk of intellectual and executive problems [19, 20]. Headache in moyamoya disease is one of the major complaints in young patients, which was mentioned by a Japanese nationwide survey [21]. The Research Committee on Moyamoya Disease classified a headache as non-ischemic symptom [2], and surgical indication for pediatric patients whose complaint is only headache is controversial. Besides, it is difficult to make a surgical decision for patients in relatively early stage of the moyamoya disease (Suzuki stage I–II) and whose cerebral blood flow (CBF) is not diminished. The purpose of this case report is to inform and infer the surgical treatment timing for pediatric moyamoya disease patients.
Case presentation
A 10-year-old girl referred to our department to investigate severe headache, which had no previous history of motor weakness, sensory disturbance, seizure and involuntary movement, and only a history of severe headache several times from childhood. Magnetic resonance image (MRI) and magnetic resonance angiography (MRA) were performed by a local doctor, and moyamoya disease was suspected.
Neuroimaging findings
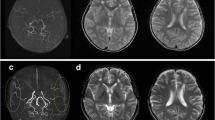
MRI did not reveal stroke lesions but multiple flow voids in the basal ganglia. The presence of stenosis of the terminal portion of the right intracranial internal carotid artery was shown by MRA. Left internal carotid angiography revealed no stenosis of the internal carotid artery, and right anterior cerebral artery was supplied from the left anterior cerebral artery via anterior commissure artery. Right internal carotid angiography demonstrated the stenosis of the terminal portion of the internal carotid artery and no anterior cerebral artery (Fig. 1). The middle cerebral artery distended compared to the left one (Fig. 1). Moyamoya vessels developed at the top of the internal carotid artery (Fig. 1). Suzuki stage was II or in transition between stage II and III. Xenon computed tomography (XeCT) showed 64.4 (at rest) and 73.9 ml/100 g/min (after diamox loading), and cerebrovascular reaction was 14.8 % in the right middle cerebral artery area (Fig. 2). There was no markedly decreased uptake in the right middle cerebral artery area in comparison with the left side (Fig. 2).
Operation
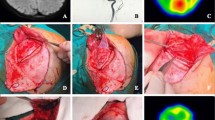
STA-MCA double anastomoses were performed. Cortical branches of middle cerebral arteries (M4) in the supra-sylvian and infra-sylvian area were selected for candidates as a recipient, and frontal branch and parietal branches of STA were manipulated as a donor. Both anastomoses were performed by 10-0 monofilament lines. Patency was evaluated by indocyanine green fluorescence angiography and micro-Doppler sonography intraoperatively. The amount of the flow of STA was 52 ml/min (systemic blood pressure was 103/52 mmHg) measured by electromagnetic blood flow meters.
Postoperative findings
Directly after the operation, XeCT was performed under sedation to evaluate hyperperfusion. Focal hyperperfusion areas were observed where bypass was conducted; however, the postoperative course was uneventful. The patient experienced no delirium, seizure, headache, and new neurological deficit. MRI showed no ischemic lesion at 5 days and 7 months after the operation. STA seemed to develop and expand in the 7 months by MRA. Selective right external carotid angiography revealed much blood supply to the right MCA area via right STA (Fig. 3).
Postoperative right carotid angiograms demonstrating bypass flow via the right external cerebral arteries supplying to the less perfusion area by MCA and ACA. Anteroposterior view (a) and lateral view (b) of right internal carotid artery. Anteroposterior view (c) and lateral view (d) of the right external carotid artery
Discussions
Most pediatric moyamoya disease patients develop ischemic symptoms including transient ischemic attack (TIA) and cerebral infarctions. Guidelines for Diagnosis and Treatment for Moyamoya Disease mentions that surgical revascularization is effective for moyamoya disease manifesting as cerebral ischemic symptoms (recommendation grade B) [2]. In the guidelines, headache is not categorized as one of the ischemic symptoms [2]. Treatment of headache of moyamoya disease patients have not been established [11]. However, severe headache is related to cerebral ischemia with disturbed cerebrovascular reactivity and may be treated by bypass therapy [8, 11]. Seol et al. mentioned that headaches can persist or develop after indirect bypass surgery despite successful prevention of cerebral ischemia [16], so direct and/or combined bypass surgery will be more beneficial for reducing of headache in moyamoya disease [8, 11]. Taking causes of childhood headache into cosideration, migraine is to be listed as one of the common differential diagnoses. On the one hand, children with moyamoya disease clinically complain of morning headache in the frontal or temporal region [8], but on the other hand, headache caused by migaine is aggravated by routine physical activity [13]. Clinically, it is difficult to distinguish between those vascular headaches. In addition, acute sinusitis, intracranial infection, trauma, and intracranial tumor should be generally considered for differential diagnoses of pediatric headache, but our present case had no evidence of infection and intracranial lesions.
Essentially, internal carotid arteries of moyamoya disease cause progressive stenosis [17]. Progression to bilateral lesions from unilateral moyamoya disease is known to occur in 25 to 58.8 % of pediatric patients [5, 14] and leads to more frequent ischemic attacks compared with non-progressed patient [9]. Family history of moyamoya disease is associated to progression from unilateral to bilateral disease [14]. Unilateral cases show earlier angiographical stage compared with bilateral cases [3], so close and careful follow-up would be essential. However, wait-and-see strategy is controversial. It may be harmful to wait and see for the occurrence of ischemic attack because of lack of knowledge which demonstrates that symptoms arise from TIA or permanent ischemia. Once cortical infarctions occur in pediatric moyamoya patients, various functions such as activities of daily living (ADL) and long-term prognosis of higher brain functions are diminished [1, 7, 15, 19, 20]. Imaizumi et al. refered that the intelligence quotient (IQ) begins to decrease after the onset of symptoms in pediatric moyamoya patients [6]. Everyone will hope to treat patients before the onset of infarctions. Typically, the sooner surgical intervention is performed, the better the clinical outcome. On the other hand, excellent patency after bypass surgery may not be promised if there is less demand in donors. STAs as a donor for bypass surgery develop in some cases after surgery in one month in accordance with the demand of less cortical perfusion pressure of recipient, [4] but some cases do not, making it difficult to distinguish the boundary line before surgery.
Because revascularization surgery improves the cerebral hemodynamics and metabolism [12, 16], preoperative evaluation by positron emission tomography (PET), XeCT, and single photon emission computed tomography (SPECT) also forms the basis of decision of surgical indication [2]. Guidelines recommend that evaluation of the cerebral hemodynamics by SPECT and PET is useful for diagnosis and assessment of the severity of cerebral ischemia in patients with ischemic-type moyamoya disease (recommendation grade B) [2]. It is widely accepted to treat patients where CBF diminishes with demonstrative perfusion; however, the main issue is indication for patients with no CBF degeneration.
Our present case was also difficult to evaluate before surgery as consideration on whether bypass patency would develop after surgery because the stage of moyamoya disease was not progressive (Suzuki stage II) and that no laterality of CBF was observed, and there was no obvious avascular area angiographically. In addition, the symptom was only severe headache. However, we regard headache as one of the ischemic signs even if CBF is not diminished by perfusion modalities such as PET, XeCT, and SECT. Our strategy for pediatric patients with moyamoya disease complaining of headache is to perform surgical intervention in the same way as TIAs [11] to prevent further ischemia.
Particularly for pediatric moyamoya patients, we also need to consider the intellectual and executive function. Children with moyamoya disease typically score significantly low in intelligence and executive functioning [19, 20]. Although the influence against intellectual and executive problems by surgical revascularization for pediatric moyamoya patients is not sufficiently elucidated [19], there are literatures that recommend early revascularization procedures to improve the CBF [7] and intellectual outcome [10] because the IQ begins to decrease after the onset of symptoms [8, 11, 16, 18]. From these points of view, early surgery should be indicated especially in pediatric patients because headache may be one of the ischemic symptoms. Besides, frequent MR follow-up does not always promise the detection of advanced disease stage before irreversible brain and intellectual damage [8, 19].
The largest limitation is that this is only one single case report, and accumulation of the similar cases will be needed.
Conclusions
STA-MCA bypass surgery was effective for the 10-year-old pediatric moyamoya disease patient with severe headache as a symptom, even though her Suzuki stage was II, and CBF study revealed no degeneration. This result shows early surgical treatment may be beneficial for early-staged pediatric moyamoya disease in particular where patients have ischemic symptoms including headache by improving perfusion pressure and cerebral circulation.
References
Choi JU, Kim DS, Kim EY, Lee KC (1997) Natural history of moyamoya disease: comparison of activity of daily living in surgery and non surgery groups. Clin Neurol Neurosurg 99(Suppl 2):S11–18
Hashimoto N, Tominaga T, Miyamoto S, Nagata I, Houkin K, Suzuki N, Koizumi A, Nogawa S, Nakagawara J, Kitagawa K, Kuroda S, Kikuta K, Fujimura M, Takahashi J, Hayashi K, Oki K, Hoshino H, Takagi Y (2012) Guidelines for diagnosis and treatment for moyamoya disease. Neurol Med Chir (Tokyo) 52(5):245–266
Hayashi K, Suyama K, Nagata I (2010) Clinical features of unilateral moyamoya disease. Neurol Med Chir (Tokyo) 50(5):378–85
Houkin K, Nakayama N, Kuroda S, Ishikawa T, Nonaka T (2004) How does angiogenesis develop in pediatric moyamoya disease after surgery? A prospective study with MR angiography. Childs Nerv Syst 20:734–741
Houkin K, Abe H, Yoshimoto T, Takahashi A (1996) Is “unilateral” moyamoya disease different from moyamoya disease? J Neurosurg 85(5):772–6
Imaizumi C, Imaizumi T, Osawa M, Fukuyama Y, Takeshita M (1999) Serial intelligence test scores in pediatric moyamoya disease. Neuropediatrics 30:294–299
Ishii R, Takeuchi S, Ibayashi K, Tanaka R (1984) Intelligence in children with moyamoya disease: evaluation after surgical treatments with special reference to changes in cerebral blood flow. Stroke 15:873–877
Kawabori M, Kuroda S, Nakayama N, Hirata K, Shiga T, Houkin K, Tamaki N (2013) Effective surgical revascularization improves cerebral hemodynamics and resolves headache in pediatric moyamoya disease. World Neurosurg 80(5):612–9. doi:10.1016/j.wneu.2012.08.005, Epub 2012 Sep 25
Kawano T, Fukui M, Hashimoto N, Yonekawa Y (1994) Follow-up study of patients with “unilateral” moyamoya disease. Neurol Med Chir (Tokyo) 34(11):744–7
Kuroda S, Houkin K, Ishikawa T, Nakayama N, Ikeda J, Ishii N, Kamiyama H, Iwasaki Y (2004) Determinants of intellectual outcome after surgical revascularization in pediatric moyamoya disease: a multivariate analysis. Childs Nerv Syst 20:302–308
Okada Y, Kawamata T, Kawashima A, Yamaguchi K, Ono Y, Hori T (2012) The efficacy of superficial temporal artery-middle cerebral artery anastomosis in patients with moyamoya disease complaining of severe headache. J Neurosurg 116:672–679
Okada Y, Shima T, Nishida M, Yamane K, Yamada T, Yamanaka C (1998) Effectiveness of superficial temporal artery-middle cerebral artery anastomosis in adult moyamoya disease: cerebral hemodynamics and clinical course in ischemic and hemorrhagic varieties. Stroke 29:625–630
Olsen J (2004) Headache classification subcommittee of the international headache society. The international classification of headache disorders; 2nd edition. Cephalalgia 24(suppl 1):1–160
Park EK, Lee YH, Shim KW, Choi JU, Kim DS (2011) Natural history and progression factors of unilateral moyamoya disease in pediatric patients. Childs Nerv Syst 27(8):1281–7. doi:10.1007/s00381-011-1469-y, Epub 2011 May 7
Scott RM, Smith JL, Robertson RL, Madsen JR, Soriano SG, Rockoff MA (2004) Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. J Neurosurg 100:142–149
Seol HJ, Wang KC, Kim SK, Hwang YS, Kim KJ, Cho BK (2005) Headache in pediatric moyamoya disease: review of 204 consecutive cases. J Neurosurg 103:439–442
Suzuki J, Kodama N (1983) Moyamoya disease—a review. Stroke 14:104–109
Vuignier S, Akioka N, Hamada H, Kashiwazaki D, Kuroda S (2014) Headache attack followed by rapid disease progression in pediatric moyamoya disease—how should we manage it? Childs Nerv Syst 30(10):1733–6. doi:10.1007/s00381-014-2408-5, Epub 2014 Apr 1
Weinberg DG, Rahme RJ, Aoun SG, Batjer HH, Bendok BR (2011) Moyamoya disease: functional and neurocognitive outcomes in the pediatric and adult populations. Neurosurg Focus 30, E21. doi:10.3171/2011.3.FOCUS1150
Williams TS, Westmacott R, Dlamini N, Granite L, Dirks P, Askalan R, Macgregor D, Moharir M, Deveber G (2012) Intellectual ability and executive function in pediatric moyamoya vasculopathy. Dev Med Child Neurol 54:30–37
Yamada M, Fujii K, Fukui M (2005) Clinical features and outcomes in patients with asymptomatic moyamoya disease—from the results of nation-wide questionnaire survey. No Shinkei Geka 33:337–342
Acknowledgments
We thank David Huang for their guidance and staff of the Department of Neurosurgery, Tokyo Women’s Medical University, in preparing this paper.
Declaration of funding source
This study was supported by research funds of the Department of Neurosurgery, Tokyo Women’s Medical University.
Conflict of interest
The authors have no personal financial or institutional interest in any of the materials or devices described in this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matsuoka, G., Aihara, Y., Yamaguchi, K. et al. Early surgical treatment benefits early staged pediatric moyamoya disease—single case report. Childs Nerv Syst 31, 1195–1199 (2015). https://doi.org/10.1007/s00381-015-2709-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2709-3