Abstract
Purpose
Pediatric cerebral sinovenous thrombosis (CSVT) is a potentially life-threatening condition which is usually diagnosed by MRI. We analyzed the signal changes of the thrombus over time and the role of diffusion-weighted/tensor imaging (DWI/DTI) in the diagnosis of CSVT.
Methods
Clinical histories were reviewed for risk factors for CSVT, neurologic manifestation, and interval from onset of symptoms related to CSVT to the neuroimaging diagnosis. MRI studies were retrospectively evaluated for the appearance of thrombi on T1- and T2-weighted, fluid-attenuated inversion recovery (FLAIR), DWI/DTI, susceptibility-weighted imaging (SWI), and magnetic resonance venography (MRV) images.
Results
Thirty-three children with CSVT were included in this study. Seventy-seven thrombi were found. Seventy-four thrombi could be identified on T1- or T2-weighted images (96 %), 72 thrombi were seen on DWI/DTI (94 %) and 68 on FLAIR (88 %). DWI showed restricted diffusion in 29 thrombi (40 %). Thrombi older than 1 day were more likely to have a T1-hyperintense signal (p = 0.002). No additional correlation between signal intensity and age of the thrombi was found. Intraparenchymal changes secondary to CSVT were seen in 11 children.
Conclusion
MR sequences individually are not sensitive enough to provide the diagnosis. DWI/DTI does not provide complementary diagnostic value. Approximation of the age of the thrombus is difficult because of poor correlation between signal intensity and age of the thrombi.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
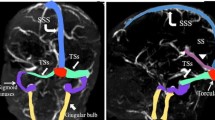
Cerebral sinovenous thrombosis (CSVT) is defined by thrombosis within the superficial (cortical veins, superior sagittal sinus, transverse sinus, sigmoid sinus, and jugular vein) or deep (inferior sagittal sinus, internal cerebral veins, vein of Galen, straight sinus) venous system [1]. Although likely underestimated, CSVT occurs in about one of 100,000 children per year including neonates and accounts for one in four cases of pediatric stroke [2]. CSVT is associated with high mortality and morbidity. Pediatric CSVT cohort studies report mortality rates of 8–19 % and severe long-term neurological sequelae in 38–48 % of patients [2, 3]. Acute antithrombotic interventions to prevent thrombus propagation are increasingly used in children and are expected to decrease the mortality and improve the long-term outcome [4]. However, the diagnosis of CSVT must first be made as soon as possible after onset of symptoms.
Neuroimaging plays a key role in the diagnosis of CSVT [5]. The primary goal of neuroimaging is (1) to visualize and characterize the thrombus, (2) to identify the degree of impaired flow within the affected venous system, and (3) to rule out secondary complications such as venous ischemia or hemorrhage. Different techniques have been applied in the diagnostic workup of CSVT: computed tomography (CT) with or without venography (CTV), magnetic resonance imaging (MRI) with or without venography (MRV), conventional angiography, and trans-fontanel Doppler ultrasonography [5]. MRI is the diagnostic modality of choice in pediatric CSVT and combines both conventional and advanced sequences such as diffusion-weighted/tensor imaging (DWI/DTI) and susceptibility-weighted imaging (SWI). Neuroimaging findings in CSVT may be subtle and a number of potential pitfalls such as anatomical variants of the cerebral venous system may challenge the diagnosis [2]. In addition, the signal characteristics of a venous thrombus may vary depending its age and utilized MR sequence. A high index of suspicion as well as familiarity with the neuroimaging findings is important for an early, sensitive, and specific diagnosis of CSVT in children.
Here, we review the experience of our tertiary university children’s hospital in the neuroimaging diagnosis of CSVT. The goals of our study were to evaluate (1) the changes in signal intensity of the thrombus over time on different MRI sequences and (2) the role of DWI/DTI in the diagnosis of CSVT.
Methods
This retrospective study was approved by our Institutional Review Board.
The inclusion criteria for this study were (1) neuroimaging diagnosis of CSVT and (2) age at diagnosis of 18 years of younger. Data from eligible children were obtained through an electronic search of our pediatric neuroradiology database covering the period between January 1, 2008 and January 31, 2014.
Clinical histories were reviewed for (1) age and gender of the children; (2) risk factors for CSVT; (3) neurologic manifestation related to CSVT according to deVeber et al. such as seizures, headaches, papilledema, and ataxia [5]; and (4) interval from onset of symptoms/findings related to CSVT to the neuroimaging diagnosis. The interval was classified as (1) less than 1 day, (2) less than 8 days, or (3) longer than 8 days. The interval from onset of symptoms/findings and the neuroimaging diagnosis of CSVT has been used to define the age of the thrombus.
All MRI studies were performed on a 1.5- or 3-T clinical scanner (Siemens, Erlangen, Germany) using our standard departmental protocol including three-dimensional T1- and axial T2-weighted images, an axial fluid-attenuated inversion recovery (FLAIR) sequence, a single-shot spin-echo, echo planar axial DTI sequence with diffusion gradients along 20 non-collinear directions (a b-value of 1000 s/mm2 was used for each of the 20 diffusion-encoding directions and an additional measurement without diffusion weighting (b = 0 s/mm2) was performed), and a time-of-flight magnetic resonance venography (TOF-MRV) or a contrast enhanced magnetic resonance three-dimensional venography (CE-MRV) with reformatted MIPs generated in a 360° tumble and rotate view. Since January 1, 2010, SWI has been included in the routine protocol for cerebrovascular disorders. For this evaluation, we used the minimum intensity projection (minIP) images. The minIP images are used to display the combined processed magnitude data using contiguous sections of thickness from 8 to 16 mm in the axial plane. In children, we typically use a minIP thickness of 16 mm with eight contiguous 2-mm slices. In neonates, a minIP thickness of 8 mm with eight contiguous 1-mm slices is preferred to avoid misinterpretation of localization or partial voluming.
All images were retrospectively evaluated by a radiology resident (MWW) and a pediatric neuroradiologist (TB). All MR images were systematically reviewed for location, number, and signal characteristics of thrombus. On T1- and T2-weighted images, the signal intensity of the thrombus was evaluated as (1) hypointense, (2) hyperintense, or (3) isointense compared to the adjacent gray matter. In addition, the diffusion characteristics of each thrombus were classified as (1) restricted or (2) normal. CE-MRV and TOF-MRV were assessed for the presence or absence of flow. Moreover, the presence of a matching SWI-hypointense signal in the location of the thrombus was evaluated for the SWI sequence. Finally, the presence of intraparenchymal edema and/or hemorrhagic infarction secondary to CSVT was assessed.
Statistical analysis was done using a z-test. Analysis was performed to evaluate the relation between age of thrombus and appearance of thrombus on T1- and T2-weighted, FLAIR, and DWI/DTI images. A p value of less than 0.05 was considered to be statistically significant.
Results
Thirty-three children with the neuroimaging diagnosis of CSVT were included in our study. Eighteen children (55 %) were male and 15 were female. The median age at time of head MRI was 5.59 years (range 4 days to 17.75 years). Five patients (15 %) were neonates, and ten patients (30 %) were younger than 1 year of age at MRI.
Risk factors for CSVT were found in 28 children (85 %). The most common risk factor was traumatic head injury (12 patients, 37 %). Other common risk factors were head and neck infections and prothrombotic disorders (six patients, 18 % and five patients, 15 %, respectively). Head and neck infection included bacterial meningitis due to Streptococcus pneumoniae, methicillin-resistant Staphylococcus aureus, and Streptococcus anginosus in four children; viral encephalitis due to presumed herpes simplex virus in one child, Lemierre syndrome in one child; and otitis media complicated by mastoiditis due to S. pneumoniae in another child. Prothrombotic risk factors comprised acute lymphatic leukemia, antiphospholipid syndrome, prothrombin G20210A mutation, antithrombin III deficiency, and an elevated homocysteine level. Each prothrombotic condition was present in a different child. Other risk factors are summarized in Table 1.
Decreased level of consciousness was the most common neurologic manifestation of CSVT in our cohort (15 patients, 50 %). The other neurologic symptoms and findings at presentation are summarized in Table 2. In three patients (9 %), no neurologic symptoms or findings primarily related to CSVT were present. These patients suffered from traumatic brain injury, resulting in loss of consciousness, and the diagnosis of CSVT was made during the initial neuroimaging workup.
The interval between onset of CSVT-related symptoms and time of neuroimaging diagnosis could be calculated for 26 out of 33 children (79 %). The interval was less than 1 day in 15 patients (45 %), less than 8 days in 10 children (31 %), and longer than 8 days (3 weeks) in one child (3 %). The interval could not be calculated in four children due to unavailability of the date of symptoms’ onset and in the other three children who presented without symptoms/findings related to CSVT.
In 33 children, we found a total of 77 thrombi. Multiple thrombi have been found in 24 patients (73 %) including five thrombi in one child, four thrombi in three children, three thrombi in nine children, and two thrombi in 11 children. In nine patients (27 %), only one thrombus was present. Thrombi have been seen at different locations within the superficial and/or deep venous system. The majority of thrombi (90 %) was found in the superficial venous system (Table 3). The transverse (34 %) and sigmoid (24 %) sinuses were the most common locations of thrombi.
The signal of the thrombus was assessed on different MRI sequences (Supplemental Table 1). Seventy-four of 77 thrombi could be identified on T1- or T2-weighted images (96 %), respectively, while 72 thrombi were seen on DWI/DTI (94 %) and 68 on FLAIR (88 %). The signal of the thrombus was variable on the MRI sequences, and several combinations were found. On T1-weighted images, the thrombus was isointense in 21 locations (28 %), hypointense in 14 (19 %), and hyperintense in 39 (53 %). On T2-weighted images, the thrombus was isointense in 20 locations (27 %), hypointense in 16 (22 %), and hyperintense in 38 (51 %). On FLAIR images, the thrombus was isointense in six locations (8 %), hypointense in 14 (21 %), and hyperintense in 48 (71 %). On DWI/DTI, restricted diffusion was seen in 29 thrombi (40 %). The most common signal patterns are shown in Table 4. Statistical analysis showed that thrombi older than 1 day have more likely a hyperintense signal on T1-weighted images compared to thrombi younger than 1 day (p = 0.002 for thrombus age less than 1 day vs. one to 8 days and p = 0.036 for thrombus age less than 1 day vs. older than 8 days). No statistically significant correlation was found between age of the thrombi and signal on T2-weighted images, FLAIR, and DTI.
Additional sequences including SWI, TOF-MRV, and CE-MRV were performed in a subset of patients. SWI was performed in 16 of 33 patients including 33 thrombi. On SWI, the thrombus was hypointense in 11 of 33 thrombi (33 %) and isointense in nine thrombi (27 %), and 13 thrombi could not be evaluated due to artifacts. No correlation was found between the signal and the age of thrombi on SWI. TOF-MRV was performed in 22 patients including 47 thrombi. A reduced or absent flow was noted for 40 thrombi (85 %). Finally, CE-MRV was performed in five patients including 14 thrombi and all showed reduced or absent flow.
Intraparenchymal changes secondary to CSVT were found in 11 of 33 children (33 %) including cytotoxic edema and hemorrhagic infarction in seven, only cytotoxic edema in two, and only hemorrhagic infarction in two patients.
Discussion
CSVT is an important cause of stroke in children, but it remains underdiagnosed because of the subtle and usually non-specific clinical presentation. A high index of suspicion is needed for clinicians and radiologists. In children, up to 60 % of CSVT occurs in neonates and infants and risk factors are identifiable in more than 95 % of patients [5]. Clinical features are usually subtle, diffuse, or misleading. The most common symptoms and clinical findings of pediatric CSVT include seizures, decreased level of consciousness, and headaches. Less common clinical presentations include papilledema, hemiparesis, visual impairment, and cranial nerve palsies [5]. All these symptoms and findings are non-specific making the early diagnosis of pediatric CSVT very challenging and typically delaying appropriate therapy. In addition, CSVT in children most commonly involves multiple vessels with the superficial sinovenous system more commonly affected compared to the deep system [5]. The age distribution, presence of risk factors, clinical features, and number as well as location of thrombi in our cohort of children with CSVT are in accordance with the literature [1, 5].
Patent venous sinuses usually have low signal intensity due to flow-related signal void on spin-echo images and are best seen on T2-weighted and FLAIR images. On spin-echo images, thrombosis causes time-dependent changes of signal intensity within the affected sinuses [6, 7]. The signal intensity varies during thrombus evolution and depends on the interval between the onset of thrombus formation and the time of imaging [8, 9]. Changes in signal intensity over time are related to the paramagnetic effects of the products of hemoglobin breakdown in the thrombus and parallels extravascular clot evolution [7, 8, 10–12]. Thrombus evolution has been classified into four different stages: (1) hyperacute thrombosis (<24 h), (2) acute thrombosis (1 to 3 days), (3) subacute thrombosis (early subacute: 3 to 7 days and late subacute: 7 to 14 days), and (4) chronic thrombosis (>14 days) [2]. Previous neuroimaging literature showed that the hyperacute thrombus has an isointense signal on T1-weighted images due to lack of flow-related signal void and a slightly hyperintense signal on T2- and FLAIR images due to residual intracellular oxyhemoglobin. In the acute stage, the thrombus may appear predominantly T1-isointense and T2- and FLAIR-hypointense due to lack of flow-related signal void and the presence of intracellular deoxyhemoglobin, respectively. During the early subacute stage, intracellular methemoglobin causes the thrombus to appear T1-hyperintense and T2- and FLAIR-hypointense. In the late subacute stage, the thrombus remains T1-hyperintense, but the accumulation of extracellular methemoglobin leads to a hyperintense signal on T2-weighted and FLAIR images. Finally, the chronic thrombus has a hypointense signal on T1-weighted, T2-weighted, and FLAIR images due to hemosiderin [2, 7, 9, 11, 13, 14]. The changes in signal intensity of the thrombus over time have been used to estimate its age [2, 7, 9, 11, 13, 14].
In our study, the signal intensity of the thrombus was highly variable on the spin-echo images. We found T1-isointensity and T1-hypointensity of the thrombus in the hyperacute and early subacute phase (Fig. 1). Iso- and hypointense signals of the thrombus on T2-weighted and FLAIR images were seen in hyperacute and acute as well as early subacute stages (Fig. 2). Finally, T1-, T2-, and FLAIR-hyperintense signal was seen at all the different stages of thrombus evolution (Fig. 3). Statistical analysis showed a significant correlation only between T1-signal intensity and age of the thrombus: T1-hyperintense thrombi were more likely to be older than 1 day. No correlation was found between age of the thrombus and signal intensity on T2-weighted and FLAIR images. Our results are not matching the previous literature. Two possible explanations are the following: (1) the duration of each stage of thrombus evolution is only approximate and factors such as variability in the degree of initial oxygenation of the red blood cells in the developing thrombus and dilution may affect the rate at which the thrombus evolves and (2) secondary extension of the thrombus may lead to different ages of thrombus evolution resulting in non-uniform signal intensities [2, 8]. In addition, the retrospective design of our study did not always allow a precise estimation of the age of the thrombus. Our study, however, matches the clinical pediatric neuroradiology daily practice and shows the difficulties in approximating the age of the thrombi.
Eleven-year-old male (patient 16) with early subacute thrombosis (7 days to diagnosis) of the superior sagittal sinus. a Sagittal T1-weighted image shows isointense clot (arrow). b Axial T2-weighted image shows hyperintense clot (arrow). c Axial FLAIR image shows isointense clot. d Trace of diffusion and e matching ADC map show restricted diffusion (bright on d, dark on e) within the clot in the superior sagittal sinus (arrows)
Four-year-old male (patient 19) with acute thrombosis (2 days to diagnosis) of the vein of Galen and straight sinus. a Sagittal T1-weighted images shows hyperintense clot (arrow). b Axial T2-weighted image shows hypointense clot (arrow) as well as hyperintense signal within the basal ganglia, thalami, and midbrain. c Axial FLAIR image shows hypointense clot (arrow) as well as hyperintense signal within the basal ganglia, thalami, and midbrain. d Trace of diffusion and e matching ADC map show normal diffusion in the vein of Galen (arrows) as well as the prognostically more favorable increased diffusion within the basal ganglia, thalami, and midbrain (bright on e)
Six-year-old female (patient 23) with hyperacute thrombosis (hours to diagnosis) of the right jugular vein. a Sagittal T1-weighted image shows hyperintense clot (arrow). b Axial T2-weighted image shows hyperintense clot (arrow). c Axial FLAIR image shows hyperintense clot (arrow). d Trace of diffusion and e matching ADC map show normal diffusion in the right jugular vein (arrows)
Although MRI is the neuroimaging diagnostic tool of choice, making the diagnosis of CSVT may be challenging. Our study shows that none of the conventional MR sequences (T1- and T2-weighted images as well as FLAIR) individually allowed in making the diagnosis of all thrombi. DWI/DTI showed abnormal (diagnostic) findings only in up to 40 % of the children (Figs. 3 and 4). Our result is in accordance with data from adults showing restricted diffusion within the thrombi in 41 % of patients with CSVT [15]. A much higher percentage of thrombi showing restricted diffusion was expected. Diffusion restriction in CSVT, however, may be smaller than what DWI/DTI allows to detect [16]. In addition, DWI/DTI was not helpful in determining the age of the thrombus. Although DWI/DTI does not provide complementary value for the diagnosis of CSVT, it plays a key role to assess important secondary complications like, e.g., venous infarction.
Three-year-old male (patient 4) with hyperacute thrombosis (hours to diagnosis) of the superior sagittal sinus. a Axial T1-weighted image shows hyperintense clot (arrow). b Axial T2-weighted image shows isointense clot (arrow). c Axial FLAIR image shows hyperintense clot. d Trace of diffusion and e matching ADC map show restricted diffusion (bright on d and dark on e) in the superior sagittal sinus (arrows)
Although performed only in a limited number of patients, TOF-MRV and CE-MRV yielded the highest sensitivity in the detection of CSVT in our study (85 and 100 %, respectively). However, MRV is typically used to confirm the suspicion of CSVT and does not routinely serve as a primary test [11, 14].
Previous literature showed that SWI may provide additional diagnostic value for thrombus detection in CSVT and be a useful adjunct to conventional MR pulse sequences [17]. In our study, however, SWI hypointensity was only found in 33 % of thrombi with no correlation to the different stages of thrombus evolution (Fig. 5).
Top row, 7-month-old female (patient 22) with hyperacute thrombosis (hours to diagnosis) of the right sigmoid sinus. a Axial T2-weighted image shows hyperintense clot (arrow). b Matching axial minimum intensity projection (minIP)-SWI image shows isointense signal in the same location (arrow). Bottom row, 6-year-old female (patient 23) with hyperacute thrombosis (hours to diagnosis) of the right transverse sinus. c Axial T2-weighted image shows isointense clot (arrow). d Matching axial minIP-SWI image shows hypointense signal at the corresponding level (arrow)
We are aware of some limitations in our study, namely (1) the retrospective nature of the study, (2) the incompleteness of acquired MRI sequences in some patients, (3) the limited number of cases, and (4) the partial lack of valuable clinical information with regard to the age of the thrombus as well as the lack of follow-up MRI.
Conclusion
Our study shows that the diagnosis of CSVT in children is challenging and requires a high index of suspicion and a careful evaluation of multiple MR sequences to depict the thrombus. MR sequences individually are not sensitive enough to provide the diagnosis. DWI/DTI and SWI do not provide complementary value for the diagnosis of CSVT compared to conventional MR pulse sequences. A high index of suspicion is needed to add TOF-MRV or CE-MRV to the routine MR protocol. Finally, our study shows almost no correlation between signal intensity changes on different MR sequences and age of the thrombus, further emphasizing the difficulties in determining the age of the thrombi.
References
deVeber G (2011) Cerebral sinovenous (venous sinus) thrombosis. In: Ganesan V, Kirkham FJ (eds) Stroke and cerebrovascular disease in childhood. Mac Keith Press, London, pp 145–159
Bracken J, Barnacle A, Ditchfield M (2013) Potential pitfalls in imaging of paediatric cerebral sinovenous thrombosis. Pediatr Radiol 43:219–231
Berfelo FJ, Kersbergen KJ, van Ommen CH, Govaert P, van Straaten HL, Poll-The BT, van Wezel-Meijler G, Vermeulen RJ, Groenendaal F, de Vries LS, de Haan TR (2010) Neonatal cerebral sinovenous thrombosis from symptom to outcome. Stroke 41:1382–1388
Roach ES, Golomb MR, Adams R, Biller J, Daniels S, Deveber G, Ferriero D, Jones BV, Kirkham FJ, Scott RM, Smith ER (2008) Management of stroke in infants and children: a scientific statement from a Special Writing Group of the American Heart Association Stroke Council and the Council on Cardiovascular Disease in the Young. Stroke 39:2644–2691
deVeber G, Andrew M, Adams C, Bjornson B, Booth F, Buckley DJ, Camfield CS, David M, Humphreys P, Langevin P, MacDonald EA, Gillett J, Meaney B, Shevell M, Sinclair DB, Yager J (2001) Cerebral sinovenous thrombosis in children. N Engl J Med 345:417–423
Sze G, Simmons B, Krol G, Walker R, Zimmerman RD, Deck MD (1988) Dural sinus thrombosis: verification with spin-echo techniques. AJNR Am J Neuroradiol 9:679–686
Macchi PJ, Grossman RI, Gomori JM, Goldberg HI, Zimmerman RA, Bilaniuk LT (1986) High field MR imaging of cerebral venous thrombosis. J Comput Assist Tomogr 10:10–15
Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF (2006) Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics 26(Suppl 1):S19–S41, discussion S42-13
Bianchi D, Maeder P, Bogousslavsky J, Schnyder P, Meuli RA (1998) Diagnosis of cerebral venous thrombosis with routine magnetic resonance: an update. Eur Neurol 40:179–190
Dormont D, Anxionnat R, Evrard S, Louaille C, Chiras J, Marsault C (1994) MRI in cerebral venous thrombosis. J Neuroradiol 21:81–99
Hedlund GL (2013) Cerebral sinovenous thrombosis in pediatric practice. Pediatr Radiol 43:173–188
Poon CS, Chang JK, Swarnkar A, Johnson MH, Wasenko J (2007) Radiologic diagnosis of cerebral venous thrombosis: pictorial review. AJR Am J Roentgenol 189:S64–S75
Isensee C, Reul J, Thron A (1994) Magnetic resonance imaging of thrombosed dural sinuses. Stroke 25:29–34
Lafitte F, Boukobza M, Guichard JP, Hoeffel C, Reizine D, Ille O, Woimant F, Merland JJ (1997) MRI and MRA for diagnosis and follow-up of cerebral venous thrombosis (CVT). Clin Radiol 52:672–679
Favrole P, Guichard JP, Crassard I, Bousser MG, Chabriat H (2004) Diffusion-weighted imaging of intravascular clots in cerebral venous thrombosis. Stroke 35:99–103
Lovblad KO, Bassetti C, Schneider J, Guzman R, El-Koussy M, Remonda L, Schroth G (2001) Diffusion-weighted mr in cerebral venous thrombosis. Cerebrovasc Dis 11:169–176
Idbaih A, Boukobza M, Crassard I, Porcher R, Bousser MG, Chabriat H (2006) MRI of clot in cerebral venous thrombosis: high diagnostic value of susceptibility-weighted images. Stroke 37:991–995
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Table 1
Signal characteristics of 77 thrombi on T1- and T2-eighted images, FLAIR, and DTI as well as time since onset of symptoms in 33 children with CSVT (DOC 111 kb)
Rights and permissions
About this article
Cite this article
Wagner, M.W., Bosemani, T., Oshmyansky, A. et al. Neuroimaging findings in pediatric cerebral sinovenous thrombosis. Childs Nerv Syst 31, 705–712 (2015). https://doi.org/10.1007/s00381-015-2662-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2662-1