Abstract
Pediatric stroke and transient ischemic attack (TIA) are uncommon but true emergencies with a wide differential diagnosis. Diagnostic imaging plays a critical role in differentiating the diverse range of etiologies. In this case, we report a 3-year-old female with no medical history who developed acute neurological deficits and demonstrate how adjunct advanced imaging including susceptibility weighted imaging (SWI) and pseudo-continuous arterial spin labeling (pCASL) can play a significant diagnostic role in the emergent setting. Imaging was performed with a Philips Ingenia 3.0T MRI. MRI brain, MR angiography (MRA), and phase contrast angiography MR Venography (PCA-MRV) were obtained. pCASL and SWI sequences were performed using SENSE (sensitivity encoding) parallel imaging techniques. MRI/MRA brain showed no restricted diffusion, abnormal T1/T2/FLAIR signal, arterial occlusion, or irregular angioarchitecture. SWI revealed increased susceptibility along the posterior falx cerebri and right posterior parietal and occipital lobes, and pCASL showed decreased blood flow within these same regions. No falcine sinus was visualized on PCA-MRV, but SWI and pCASL findings led to diagnosis of falcine sinus thrombosis and initiation of appropriate treatment. Repeat MRI one month later showed interval resolution of the abnormal SWI findings and a now patent persistent falcine sinus visualized on PCA-MRV imaging. Routine use of SWI imaging on all brain MRIs and addition of pCASL imaging when there is concern for ischemia or infarction in the emergent setting can limit the risk of missed occult diagnoses like a thrombosed falcine sinus.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pediatric stroke and transient ischemic attack (TIA) are uncommon but true emergencies with a wide range of etiologies, including complications of embryologic structures such as a falcine sinus [1, 2]. A falcine sinus is an embryologic venous drainage pathway between the vein of Galen and the superior sagittal sinus, which typically closes around birth [2, 3]. While a persistent falcine sinus is often an incidental finding, it is a potential source of venous thrombosis and has been associated with transient ischemic attack and venous infarction [4, 5]. Below is the case of a 3-year-old female who presented acutely with transient neurologic deficits and was found to have a falcine sinus thrombosis. Key clinical and radiologic features of falcine sinus thromboses are reviewed with emphasis on how advanced imaging techniques such as susceptibility weighted imaging (SWI) and pseudo-continuous arterial spin labeling (pCASL) can play a significant diagnostic role in the emergent setting.
Case
A developmentally normal 3-year-old female with no significant medical history presented to the emergency department with acute left upper extremity weakness, headache, and slurred speech with left-sided facial droop. Her left upper extremity weakness resolved by the time of initial evaluation in the emergency department, and after subsequent 15 min of monitoring, her other neurological abnormalities resolved as well. Given her resolution of acute symptoms, tissue plasminogen activator (tPA) and computed tomography (CT) of the head were deferred in favor of expedited magnetic resonance (MR) imaging under sedation after several hours of observation.
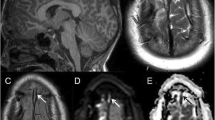
MRI brain, MR angiography (MRA), and phase contrast angiography MR venography (PCA-MRV) were obtained. MRI/MRA brain showed no restricted diffusion, abnormal T1/T2/FLAIR signal, arterial occlusion, or abnormal angioarchitecture. There were no masses and no congenital or parenchymal abnormalities. SWI revealed multiple curvilinear regions of increased susceptibility along the posterior falx cerebri and right posterior parietal and occipital lobes (Fig. 1e). Furthermore, pCASL showed decreased blood flow within the regions of abnormal susceptibility signal in the right posterior parietal and right occipital lobes (Fig. 1g). There was no falcine sinus visualized on initial PCA-MRV (Fig. 1a/c). The SWI and pCASL findings of decreased cerebral blood flow, abnormal signal of the falx cerebri, and subsequent engorgement of the right posterior parietal and occipital venous drainage pathways helped to identify and confirm the diagnosis of venous thrombosis in a persistent falcine sinus.
Pretreatment sagittal 3D PCA-MRV image of the brain (a) shows decreased opacification of the persistent falcine sinus with possible filling defect near its origin at the vein of Galen. On one-month post-treatment 3D PCA-MRV imaging (b), there is increased signal consistent with filling of the falcine sinus. This finding is better characterized on the pre- and post-treatment 3D PCA-MRV reconstructions (c and d). Initial pretreatment SWI (e) of the brain showing thrombus within the falcine sinus (closed arrow) and multiple curvilinear regions of susceptibility artifact in the right posterior parietal and right occipital lobes that are consistent with venous engorgement (open arrow). SWI one-month post-treatment (f) of the brain showing interval resolution of falcine sinus thrombus and venous engorgement in those same regions. Corresponding initial pretreatment pCASL image (g) of the brain showing region of decreased cerebral blood flow involving the posterior right frontal, right parietal, and right occipital lobes. The venous engorgement is in the same venous vascular distribution as the decreased cerebral blood flow
The patient began treatment for venous thrombosis with weight-based Lovenox and hydration. Other work-up was normal with no evidence of systemic hypercoagulability. She had no recurrence of symptoms after initial presentation. Repeat MRI brain and PCA-MRV were performed one month after her initiated treatment. MRI showed interval resolution of the abnormal SWI signal along the posterior falx cerebri and right posterior parietal and occipital lobe veins (Fig. 1e/f). On the PCA-MRV imaging, the persistent falcine sinus was visualized (Fig. 1b/d) confirming the diagnosis and successful reabsorption of a persistent falcine sinus thrombosis.
Imaging technique
Using a Philips Ingenia 3.0 T MRI and 20 channel head coil, pCASL and SWI sequences are performed on all examinations concerning for possible neurovascular pathology. PCASL uses SENSE (sensitivity encoding) parallel imaging techniques, performed in image space after reconstruction of data from the base and head coils. This produces the highest possible temporal resolution. The scan is a Fast Field Echo (FFE) with a field of view (FOV) of 240 × 240 × 95 mm (RL × AP × RH), ACQ voxel size of 2.75 × 0.75 mm (RL × AP), and matrix size of 88 × 88 (RL × AP). The TE is set to “shortest” at 16 ms, TR set to 4550 ms, and a flip angle of 90 degrees. Arterial spin labeling is performed 90 mm inferior to the skull base with the post-label decay set to 1600 ms. Sixteen slices are obtained in a transverse orientation with a slice thickness of 5 mm and a 1-mm gap between slices. The total scan time is 04:42 (min:sec). Images are typically obtained using a pseudo-continuous labeling method with a single-phase image acquisition following the post-label delay. After the delay, read out occurs and measures the signal (spins) from the arterially labeled blood throughout the brain arterial system and creates an image. A color scheme is applied to the grayscale images where the grayscale intensity is based on the strength of the returned signal, resulting in the final images.
SWI also employs SENSE parallel imaging techniques to obtain the highest possible temporal resolution. The scan is a T1 Fast Field Echo with a field of view of 180 × 230 × 149 mm (RL × AP × FH), ACQ voxel size of 0.6 × 0.6 × 2 (RL × AP × FH), and matrix size of 384 × 301 (AP × RL). The TE first is set at 7.2 ms with 6.2 ms echo spacing and a flip angle of 17 degrees. The TR is set to 31 ms with delta TE set to 6.2 ms. One hundred forty-nine slices are obtained in transverse orientation with a slice gap of 1-mm. The total scan time is 02:49 (min:sec).
Discussion
Prompt diagnosis of acute stroke or TIA can be challenging in the pediatric population given the broad differential diagnosis and relative rarity of the conditions [4]. The patient described above suffered a TIA secondary to a thrombosed falcine sinus. If left untreated, the patient could have developed a venous infarct in the draining venous vascular territory of the right parietal and occipital lobes. The occipital lobe territory affected may have caused cortical blindness.
Persistent falcine sinuses were once thought to be rare; however, recent studies have shown a much higher incidence ranging from 2.1 to 5.3% in the general population [5, 6]. Thrombosis of a persistent falcine sinus reduces venous flow dynamics in its corresponding draining venous territory, which results in segmental venous hypertension and engorgement. This can lead to venous infarction if alternative drainage pathways are not present, resulting in restricted diffusion and T2/Flair abnormalities in the affected cerebral parenchyma [3]. Given that persistent falcine sinus thromboses often lack the significant abnormalities seen on standard MRI brain sequences, especially in pediatric patients, this diagnosis can be easily overlooked [1].
Previously, persistent falcine sinus thrombosis and cerebral sinovenous thrombosis (CSVT), in general, were often diagnosed with contrast-enhanced MRV [3, 4, 6]. As demonstrated in Fig. 1a, however, a persistent falcine sinus thrombosis may show incomplete or absent opacification on PCA-MRV. Alternatively, SWI sequences can enhance evaluation of congested and engorged venous vasculature by revealing paramagnetic susceptibility effects of deoxygenated blood [7]. SWI is also far more sensitive at detecting these blood products than standard T2*-weighted gradient-recalled echo (GRE) sequences often performed in community settings [4]. Furthermore, the ability of SWI to demonstrate venous output from ischemic tissues is well-established and can help to indicate the severity of a perfusion disturbance [8].
ASL sequences and pCASL, in particular, are more sensitive to the subtle perfusion abnormalities in TIA than diffusion weight imaging (DWI) or MRA [9]. Additionally, when performed early in an acute diagnostic evaluation, pCASL can demonstrate perfusion abnormalities in TIA patients with otherwise normal imaging [10]. pCASL has emerged as the preferred MR perfusion technique (especially in pediatric patients), primarily due to its ability to avoid contrast agents and instead use blood as endogenous tracer. It further improves the signal to noise ratio (SNR) relative to other ASL sequences and can also be performed on systems not capable of continuous radiofrequency pulses [1].
Conclusion
Routine use of SWI imaging on all brain MRIs and addition of pCASL imaging when there is concern for ischemic vascular pathology in the emergent setting can limit the risk of missed occult diagnoses like a thrombosed falcine sinus and facilitate immediate appropriate treatment. The unique sensitivity of SWI to identify microscopic blood products, particularly at high (3T) field strength, allows for enhanced evaluation of venous thromboses and congestion. pCASL further works for dynamic assessment of perfusion alterations in cerebral blood flow to confirm potential causes of abnormal static findings. As this case of venous sinus thrombosis illustrates, both of these imaging techniques can play key roles in early accurate diagnosis of venous thrombosis and should be considered for utilization when possible in the future.
Data availability
Not applicable.
References
Khalaf A, Iv M, Fullerton H, Wintermark M (2018) Pediatric stroke imaging. Pediatr Neurol 86:5–18
Smith A, Choudhary A (2014) Prevalence of persistent falcine sinus as an incidental finding in the pediatric population. Am J Roentgenol 203:424–425
Lee I, Leach J, Tomsick T, Flaherty M (2015) Pearls & Oysters: cerebral venous sinus thrombosis involving a persistent falcine sinus. Neurology. 85(22):162–164
Mirsky D, Beslow L, Amlie-Lefond C (2017) Pathways for neuroimaging of childhood stroke. Pediatr Neurol 69:11–23
Lin L, Lin J, Guan J et al (2018) Falcine sinus: incidence and imaging characteristics of three-dimensional contrast-enhanced thin-section magnetic resonance imaging. The Korean Society of Radiology 19(3):463–469
Ryu C (2010) Persistent falcine sinus: is it really rare? Am J Neuroradiol 31:367–369
Meoded A, Poretti A, Benson J et al (2014) Evaluation of the ischemic penumbra focusing on the venous drainage: the role of susceptibility weight imaging (SWI) in pediatric ischemic cerebral stroke. J Neuroradiol 41:108–116
Havsteen I, Willer L, Ovesen C, Nybing JD, Ægidius K, Marstrand J, Meden P, Rosenbaum S, Folke MN, Christensen H, Christensen A (2018) Significance of arterial spin labeling perfusion and susceptibility weighted imaging changes in patients with transient ischemic attack: a prospective cohort study. BMC Med Imaging 18:24
Zaharchuk G, Olivot J, Fischbein N et al (2012) Arterial spin labeling imaging findings in transient ischemic attack patients: comparison with diffusion- and bolus perfusion-weighted imaging. Cerebrovasc Dis 34(3):221–228
Qiao X, Salamon N, Wang D, et al. Perfusion deficits detected by arterial spin labeling (ASL) in TIA Patients with Negative Diffusion and Vascular Imaging
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This report was approved by the author’s institution’s authored works component of the Directorate of Quality Management for submission for publication as a CASE REPORT/SERIES, #2413.
Consent to participate/for publications
This work was determined to be HIPAA compliant by the author’s institution’s authored works component of the Directorate of Quality Management for submission for publication. As such, consent to participate was not required for the present case report as all information and images are anonymized.
Disclaimer
The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the views, opinions or policies of the Department of the Navy, the Department of Defense (DoD), or the US Government. Mention of trade names, commercial products, or organizations does not imply endorsement by the US Government.
Copyright statement
The authors are military service members or employees of the US Government. This work was prepared as part of their official duties. Title 17 U.S.C. §105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. §101 defines a US Government work as a work prepared by a military service member or employee of the US Government as part of that person’s official duties.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Spiro, J.D., James, W.F. & Cho, A.A. Utility of susceptibility weighted imaging (SWI) and pseudo-continuous arterial spin labeling (pCASL) in diagnosis of falcine venous thrombosis in a child with transient ischemic attack. Emerg Radiol 28, 683–686 (2021). https://doi.org/10.1007/s10140-020-01882-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-020-01882-2