Abstract
Background
Though the foramen magnum (FM) is often altered in complex craniosynostosis, no study analysed the FM dimensions in patients with brachycephaly specifically.
Patients and methods
We measured the FM area, sagittal and transverse diameters on preoperative CT scans in patients with bicoronal synostosis (n = 40) and age-matched control group (n = 18). Our study included 16 children with FGFR3 p.Pro250Arg mutation (mean age 6.1 months), 10 with TWIST-1 mutation (mean age7.6 months) and 14 patients with isolated bicoronal synostosis (mean age 6.1).
Results
We observed a significantly smaller FM area in FGFR3 group compared to control group and isolated brachycephaly group (p = 0.001 and p = 0.038, respectively). The mean FM area in FGFR3 group was 426.13 mm2 (p = 0.001), while in TWIST-1 group was 476.34 mm2 (p = 0.103), and in isolated brachycephaly group 489.43 mm2 (p = 0.129) compared to control group: 528.90 mm2. The posterior segment of the sagittal diameter of the FM and its width as well as the bi-interoccipital synchondrosis diameters were significantly smaller in FGFR3 group compared to control group. In TWIST-1 group, the only altered dimension was the FM anterior segment of the sagittal diameter (p = 0.008). We did not observe any significant alteration of FM in patients with isolated brachycephaly compared to control group.
Discussion and conclusions
The FM area is significantly altered in FGFR3-related brachycephaly, whereas in patients with Saethre–Chotzen syndrome (TWIST-1 mutation) the mean FM area is similar to control group. This study confirms the importance of FGFRs on FM growth whereas TWIST-1 seems to have a minor role.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
FGFRs play a major role in the growth of the skull base. Some FGFRs mutations are associated with an altered growth of the foramen magnum.
In fact, in achondroplasia (FGFR3 related), as well as in Crouzon syndrome (FGFR2 related), the size of the foramen magnum (FM) is significantly reduced [2–4, 8, 12]. However, in such syndromes the growth of the whole craniofacial skeleton including the face is also altered [1, 6]. In this study, we evaluated the extent of the alterations of the FM in milder forms of craniofacial anomalies in which the growth of the face is typically not affected, such as the bicoronal craniosynostosis.
We analysed the dimensions of the FM in brachycephalic children in particular, in two craniosynostosis forms with two underlying genetic mutations (p.Pro250Arg FGFR3 of the so-called Muenke–Lajeunie syndrome, and TWIST-1 mutation of the Saethre–Chotzen syndrome (SCS)) [9] and in "isolated" brachycephalies non-FGFR3 non-TWIST-1.
Patients and methods
Population
All infants with a bicoronal synostosis followed at the Craniofacial Unit of the Pediatric Neurosurgical Department of Necker Hospital, Paris and who underwent digital preoperative thin cut CT scans between 2006 and 2012 were considered for this study. A genetic testing searching for FGFR2, FGFR3 and TWIST-1 mutations was performed in all of them at the time of surgery. Children were divided into three groups: FGFR3 group in case of p.Pro250Arg FGFR3 mutation (so-called Muenke–Lajeunie syndrome), TWIST-1 group in case of TWIST-1 mutation or deletion of the Saethre–Chotzen syndrome) and "isolated brachycephaly" group in case where no mutation in FGFR2 nor FGFR3 nor TWIST-1 were found.
An age-matched control group was created which included infants submitted to a CT scan for a head injury (infants with skull or cerebral parenchymal lesions were excluded).
Measurements
Computer analysed millimetric data acquisition and anatomic measurements of FM dimensions on preoperative CT scans were obtained by Osirix v. 3.9.4 32 – bit.
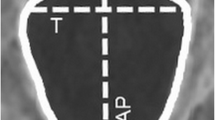
Six measurements of FM were performed according to our previous study (Fig. 1) [2]:
-
Area: Foramen magnum area [mm2]
-
Sagittal diameter: the maximum sagittal dimension of foramen magnum length: basion to opisthion (sd) [mm]
-
Anterior sagittal diameter: basion to anterior bi-interoccipital synchondrosis (sdi) [mm]
-
Posterior-sagittal diameter: anterior bi-interoccipital synchondrosis to opisthion (sdio) [mm]
-
Foramen magnum width: maximum dimension of foramen magnum width (td) [mm]
-
Anterior bi-interoccipital synchondrosis width (tdi) [mm]
Statistical method
For the statistical analysis of our series we used the directional non-parametric statistical hypothesis Mann–Whitney–Wilcoxon rank-sum test to compare the measured parameters in each group using z scores. The alternative hypothesis (control group measurements higher than in brachycephaly groups) was accepted if the results were considered significant (p ≤ 0.05).
A graphical analysis was performed using a Loess non-parametric regression for each measured value. Best-fit curves were calculated on the scatterplot of each measurement against age using 0.75 as the smoothing parameter when comparing brachycephaly and control group and 0.99 when analyzing the subgroups (FGFR3, TWIST-1 and isolated brachycephaly groups). These curves extrapolate the change of measurements during childhood.
All statistical data were analysed by IBM SPSS Statistics version 20 for mac OS X 10.7.5.
Results
During the period studied 40 infants with a brachycephaly were operated on at Necker Craniofacial Unit. The genetic analysis allowed dividing them in the three groups: FGFR3 (n, 16), TWIST-1 (n, 10) or isolated (n, 14).
FGFR3 group
The FGFR3 group included 16 patients with a genetically confirmed FGFR3 p.Pro250Arg mutation and bicoronal suture synostosis. The age of the patients ranged between 3 to 8 months (mean age 6.10 months, median 6.02 months, standard deviation 1.29 and sex ratio 0.5).
TWIST-1 group
The group of children with Saethre–Chotzen syndrome included 10 patients aged from 1 to 11 months (mean 6.37, median 6.4, standard deviation 2.82 and sex ratio 1). All children in this group had genetically confirmed mutation of TWIST-1 gene.
Isolated brachycephaly group
The group of patients with non-syndromic isolated brachycephaly included 14 patients with bicoronal suture synostosis and negative test of FGFR 2, FGFR 3 and TWIST-1 mutations. Age ranged from 0 to 8 months (mean age 6.10 months, median 6.15 months, standard deviation 2.31 and sex ratio 1.3). In this group we found a patient (# 12) having a large posterior fossa cyst and large craniometric dimensions of the FM. For such a reason we performed a double statistical analysis of the series—including and excluding patient # 12.
Control group
Age-matched control group included 18 patients aged from 0 to 8 months (mean age 5.78 months, median 6.24, standard deviation 1.92 and sex ratio 1.25).
Table 1 shows the composition of the studied population and a summary of craniometric data. To be noted, none of the children in our study presented with hydrocephalus or cerebellar tonsillar prolapse on pre-operative CT scan.
Foramen magnum area
A significant difference of FM area between the groups was observed. The mean FM area was smallest in FGFR3 group (mean area 426.13 mm2). Mean FM area in Twist group was 476.34 mm2, in patients with isolated brachycephaly 489.43 mm2 and in control group 528.90 mm2 (Fig. 2).
We found a significant difference in the foramen magnum area when comparing children with brachycephaly and control group (p = 0.004, z = 2.857 and p = 0.002, z = 3.073 when patient # 12 was included and excluded, respectively).
The FM area was significantly smaller in FGFR3 group compared to control group (p = 0.001, z = 3.347) and to isolated brachycephaly group (p = 0.038, z = 2.079). However, no significant differences were observed when comparing FGFR3 group to Saethre–Chotzen group (p = 0.182, z = 1.370) or to isolated brachycephaly group when patient # 12 was excluded (p = 0.066, z = 1.842, respectively). No statistically significant differences were found when comparing TWIST-1 group to control group or isolated brachycephaly group to control group.
After extrapolation, the Loess curve of the FM area for bicoronal synostosis group was inferior to the control group curve. Similarly, when divided into subgroups, the loess curve of FGFR3 group was inferior to the curve of Saethre–Chotzen group, non-syndromic group and control group. The Loess curve of TWIST-1 group was very similar to the curve of isolated brachycephaly group after the age of 4 months (Fig. 3).
Sagittal diameter
A statistically significant difference in sd dimension was noted in FGFR3 group compared to control group (p = 0,012, z = 2,502). The sd difference was not statistically significant between children with Saethre–Chotzen syndrome and control group (p = 0.314, z = 1.007), nor between patients with isolated brachycephaly and control group.
The Loess curve of brachycephaly was below the curve of control group after the age of 4 months. For FGFR3 group the Loess curve was always inferior to the curve of patients with isolated brachycephaly, control group and TWIST-1 group (Fig. 4).
The extrapolation of the growth rate showed some differences in the growth pattern of sd between the groups. In FGFR3 group, we found a rapid growth of sd until the age of 6 months with a stabilisation afterwards, whereas the growth pattern in other groups was more linear.
Anterior sagittal diameter
Interestingly, the only statistically significant value in the anterior sagittal diameter was observed in TWIST-1 group: when compared to control group, the sdi dimension was significantly smaller in children with Saethre–Chotzen syndrome (p = 0.008, z = 2.637).
We did not note any other statistically significant difference in sdi dimensions between the other groups
Loess curve of patients with bicoronal synostosis was similar to the curve of control group (Fig. 5). When divided into subgroups, by extrapolation we could observe a rapid increase of sdi in FGFR3 group before the age of 5 months, with a stabilisation afterwards. The growth pattern of sdi in other groups was more linear. Specifically in Saethre–Chotzen group, we did not observe any increase of sdi with ageing of the child.
Posterior sagittal diameter
sdio dimensions were significantly lower in children with FGFR3 group than in control group (p = 0.009, z = 2.605). Significantly larger sdio were noted in patients with TWIST-1group compared to FGFR3 group (p = 0.002, z = 3.162), or isolated brachycephaly group (p = 0.021 and p = 0.05, z = 2.313 and z = 2.698 for inclusion and exclusion of patient # 12, respectively), but not when compared to control group (p = 0.125, z = 1.534).
The Loess curve for FGFR3 group was inferior to that of the isolated brachycephaly, Saethre–Chotzen and control group curve. By extrapolation, we noted a rapid sdio growth phase in children in FGFR3 group until the age of 6 months with a stabilisation of growth afterwards (Fig. 6).
Foramen magnum transverse diameter
A significant reduction of td was observed in FGFR3 group when compared to control group (p = 0.005, z = 2.795). No statistically significant difference in TWIST-1 group or isolated brachycephaly were found.
The Loess curve of FGFR3 group was always under the non-syndromic brachycephaly and control group curve (Fig. 7).
By extrapolation, we can observe two phases of rapid growth rate of td dimension in patients with bicoronal synostosis: before the age of 4 months and after the age of 7 months. When divided to subgroups, this growth pattern only applies to isolated brachycephaly group. Surprisingly, the growth pattern of td in children in Muenke–Lajeunie group is very stable; the td dimension does not show any enlargement with ageing of the child.
Bi-interoccipital synchondrosis diameter
We found a statistically significant difference of tdi in the FGFR3 group where tdi was significantly smaller than in controls (p = 0.010, z = 2.588). Statistically significant differences were not noted when comparing the isolated brachycephaly group to control group or Saethre–Chotzen group to control group (p = 0.170 and 0.401, z = 1.372 and 0.839, respectively).
By extrapolation of the Loess curve, in patients with Muenke–Lajeunie syndrome we observed the same phenomena as in td dimension—there was no enlargement of tdi with the ageing of patient. No statistically significant differences of tdi growth pattern were observed when comparing control group and patients with bi-coronal synostosis (Fig. 8).
Discussion
The ontogenesis of FM is complex [5, 10, 11]. The FM is bound by the exoccipital, supraoccipital and basooccipital bones, which develop and grow by endochondral ossification. The bones are separated by two anterior and two posterior synchondrosis that begin to fuse by 3 to 4 years and 7 years, respectively. A small FM will result in case of abnormal endochondral ossification or in case of premature synchondrosis fusion or when both events occur simultaneously [14]. In our series, despite the measurements of the FM were reduced, no synchondrosis fusion was observed.
According to Richards and Jabbour [13], the bony FM is divided into ventral and dorsal units. In the foetal period, growth is dominated by increases in dorsal unit length. This growth pattern changes between birth and 6 months of age as the ventral unit increases at a faster rate. After 6 months, the dorsal part of the FM reduces its growth rate, though continuing to develop slowly to arrest at 1 year of age while the ventral part continues to maintain a high growth rate until age of 1. Consequently, during the foetal period, the growth of FM is dominated by an increase in length, while in the first six postnatal months, it is the width that increases. In the ninth postnatal month, the growth in length and in breadth of the dorsal unit is equal [13].
To our knowledge, only the FGFR-related alterations in growth and size of the FM in Crouzon syndrome and achondroplasia were described [2, 4, 13]. In our previous study, we documented a significantly smaller FM area, sd and sdio compared to control group in FGFR2 Crouzon syndrome [2]. In achondroplasia, the smaller FM area results from the abnormal endochondral ossification of the basiocciput with a premature fusion of the synchondrosis [8]. This study identifies the alterations of FM in isolated and syndromic brachycephaly related to FGFR3 or TWIST-1 mutations, which account for 44 % of all the genetic causes of craniosynostosis [7].
Comparative analysis of FM in isolated and syndromic brachycephaly
The FM area was significantly smaller in children with bicoronal synostosis compared to control group (p = 0.004). However, when divided to isolated and syndromic brachycephaly, the only significant alteration of FM area was noted in FGFR3 group. The mean FM area in FGFR3 group was 426.13 mm2 (p = 0.001), followed by TWIST-1 group—476.34 mm2 (p = 0.103) and isolated brachycephaly group—489.43 mm2 (p = 0.055) compared to control group—528.90 mm2 (Fig. 2). The alterations of FM area in FGFR3 group were statistically significant also when comparing to isolated brachycephaly group (p = 0.038).
Foramen magnum width was significantly smaller in brachycephalic patients compared to control group (p = 0.036). When divided to syndromic and non-syndromic brachycephaly, FM width was significantly smaller in FGFR3 group (p = 0.005).Similarly, the second transverse dimension—bi-interoccipital synchondrosis was also altered in FGFR3 group (p = 0.01).
Surprisingly, by extrapolation of Loess curves for transverse dimensions, we observed that td and tdi in patients with Muenke–Lajeunie syndrome did not show any increase in size with ageing of children. Such observations need some longitudinal analysis and further studies to be confirmed.
Similarly, the only statistically significant difference of sd was observed in Muenke–Lajeunie group (p = 0.012). The alteration of sd was mostly composed by reduced growth of dorsal part of FM (sdio), which was significantly smaller in FGFR3 patients compared to control group (p = 0.009). This finding is consistent with Richards and Jabbour’s theory that the growth of FM in the foetal period and first 6 months of life is mostly depending on the growth of dorsal part of FM [13].
The extrapolated growth rate of the sd was also different among the groups. In fact, we observed a rapid increase of sagittal dimension in FGFR3 group until the age of 5 months with stabilisation afterwards, whereas the growth pattern in other groups was more linear.
This finding suggests that sagittal and transverse growths of the FM are differently affected in children harbouring a FGFR3 p.Pro250Arg mutation.
While the posterior part of the sagittal diameter was significantly reduced in FGFR3 group, the ventral part of FM was the only parameter altered in patients with SCS. In TWIST-1 patients the sdi was indeed significantly smaller compared to control group (p = 0.008). Such alteration in sdi was found mainly in TWIST-1 group, and not in the other groups. It suggests a specific role of TWIST-1 in the growth of the skull base at the level of the anterior part of the foramen magnum.
Conclusion
To the best of our knowledge, this is the first study to compare FM dimensions in children with isolated and syndromic brachycephaly (Muenke–Lajeunie syndrome and Saethre–Chotzen syndrome) using thin cut 3D CT scans. We observed a significantly smaller FM area in children with brachycephaly than control group (p = 0.004). Among the brachycephalic infants, the differences in FM area were statistically significant only in children with Muenke–Lajeunie syndrome—where we found a significantly smaller FM area compared to the isolated brachycephaly group (p = 0.001 and 0.038, respectively). Such small surface is mainly depending on a reduction of the transverse diameter, as the growth of the FM appears to occur principally along the sagittal plane in FGFR3 children during the first post-natal months.
This is in contrast with SCS syndrome where the only alteration of FM observed was a reduction in the anterior segment of the sagittal diameter (p = 0.008). Interestingly, such reduced growth was only found in patients with SCS.
References
Béder I, Horn F, Trnka J, Bielek J, Omaník P (2009) Craniosynostosis. Slovenskáchirurgia 6(2):22–25
Coll G, Arnaud E, Selek L, Brunelle F, Sainte-Rose C, Collet C, Di Rocco F (2012) The growth of the foramen magnum in Crouzon syndrome. Childs Nerv Syst 28:1525–1535
Goodrich JT (2005) Skull base growth in craniosynostoses. Child’s Nerv Syst 21(10):871–879
Hecht JT, Horton WA, Reid CS, Pyeritz RE, Chakraborty R (1989) Growth of the foramen magnum in achondroplasia. Am J Med Genet 32(4):528–535
Helms JA, Amasha RR, Leucht P (2007) Bone voyage: an expedition into the molecular and cellular parameters affecting bone graft fate. Bone 41(4):479–485
Horn F, Béder I, Omaník P, Sýkora P, Trnka J (2009) Craniosynostosis and surgical treatment options. Cesk Pediatr 64(11):603–604
Johnson D, Wilkie AO (2011) Craniosynostosis. Eur J Hum Genet 19(4):369–376
Ozcetin M, Arslan MT, Karapinar B (2012) An achondroplasic case with foramen magnum stenosis, hydrocephaly, cortical atrophy, respiratory failure and sympathetic dysfunction. Iran J Pediatr 22(1):121–124
Lattanzi W, Bukvic N, Barba M, Tamburrini G, Bernardini C, Michetti F, Di Rocco C (2012) Genetic basis of single-suture synostoses: genes, chromosomes and clinical implications. Child’s Nerv Syst 28:1301–1310
Menezes AH (2008) Craniocervical developmental anatomy and its implications. Child’s NervSyst 24:1109–1122
Pang D, Thompson DN (2011) Embryology and bony formation of the cranioovertebral junction. Child’s Nerv Syst 27(4):523–564
Reina V, Baujat G, Fauroux B, Couloigner V, Boulanger E, Sainte Rose C, Maroteaux P, Le Merrer M, Cormier-Daire V, Legai-Mallet L, Zerah M, Di Rocco F. Cranio vertebral junction anomalies in achondroplastic children. (2013) Advances and Technical Standards in Neurosurgery
Richards GD, Jabbour RS (2011) Foramen magnum ontogeny in Homo sapiens: a functional matrix perspective. Anat Rec (Hoboken) 294(2):199–216
Stevenson RE, Hall JG. (2006) Human malformations and related anomalies. Oxford University Press, Oxford, ISBN 0195165683.p.261.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Di Rocco, F., Dubravova, D., Ziyadeh, J. et al. The Foramen magnum in isolated and syndromic brachycephaly. Childs Nerv Syst 30, 165–172 (2014). https://doi.org/10.1007/s00381-013-2245-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-013-2245-y