Abstract
Background
Though the craniovertebral junction is often abnormal in children with Crouzon’s syndrome, no study had measured accurately the size of their foramen magnum (FM).
Patients and methods
We compared the FM size (area, diameters) on computed tomography examination in 21 children with a genetically confirmed Crouzon’s syndrome prior to any surgery and in 23 control children without craniofacial abnormalities. We extrapolated the growth pattern in both groups.
Results
We found a statistically significant smaller FM area (p = 0.0228), FM sagittal diameter (p = 0.0287), and FM sagittal posterior diameter (p = 0.0023) in children with Crouzon’s syndrome. No differences were detected with regard to the transversal diameter. Hydrocephalus in children with Crouzon’s syndrome was associated with a small FM area (p = 0.05), small sagittal diameter (p = 0.023), small sagittal posterior diameter (p = 0.0173), and reduced transversal diameter (p = 0.03985). No association of the aforementioned findings was found with the position of the cerebellar tonsils or the lambdoid suture functional state (open or fused). Comparable results were observed among the two genetic forms (exon 8 or 10 mutations). Concerning the growth pattern, a first phase of rapid increase and a second phase of slow increase could be recognized in all the measurements in both populations, though with some significant differences.
Discussion and conclusions
The growth of FM follows a biphasic pattern in both Crouzon’s and control children. The sagittal diameter and the global size of the FM are mostly affected in children with Crouzon’s syndrome. The small FM, especially its posterior part, is likely to play a key role in the physiopathology of hydrocephalus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One century ago, Crouzon described a syndrome associating a cranial synostosis and facial dysmorphism characterized by hypertelorism, exophthalmos, hypoplastic maxilla with relative prognathism, parrot-beaked nose, and a short upper lip that has been named after him [11]. This syndrome is nowadays well known both from the phenotypic and genetic points of view. Several mutations in the fibroblast growth factor receptors 2 (FGFR2) gene have been described [2]. However, only a few studies have been addressed at understanding the growth process of the skull base in this type of complex craniosynostosis. Two papers have suggested that the foramen magnum (FM) might be smaller in patients with Crouzon’s syndrome [14, 18], but to the best of our knowledge, none has tried to analyze its size and growth pattern in detail.
The aim of this study was to evaluate the FM size and its various diameters in children of different ages with Crouzon’s syndrome and in control children of comparable ages as well as their variations during the early phases of life based on computed tomography (CT) studies.
Patients and methods
Population
The group of patients with Crouzon’s syndrome included 21 children with a genetic confirmation of FGFR2 gene mutation. All the patients presented with craniofacial retrusion and/or a cranial synostosis (mean age, 30.28 months; median, 19 months; standard deviation, 35.72). Sex ratio was 1.1. Twenty out of 21 children had a facial retrusion; 18 out of 21 children had a cranial synostosis.
An age-matched control group was constituted for comparison. It included 23 children admitted at Necker’s Hospital Neurosurgical Pediatric Unit in emergency because of a polytraumatism and who underwent a body CT scan to rule out a cerebral lesion. Children with cranial bone lesions or any brain injury were excluded. Their age at the CT scan study ranged from 1 to 130 months; mean age was 30.22 months, median 22 months, and standard deviation of 32.09. Sex ratio was 1.87.
Computer-aided analysis of the skull
Carestream PACS 11.0 for Windows XP was used for the anatomical measures and CT data treatment. CT scan acquisitions were millimetric. Richards and Jabbour [22] divided the FM into two functional matrices: a dorsal and a ventral one. We used this definition to analyze the FM area and the diameters in Crouzon’s and the control population.
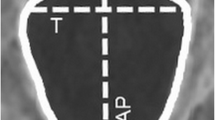
Six axial measurements were defined and analyzed according to Richards and Jabbour [22].
-
Area: the foramen magnum’s area
-
sd: the foramen magnum’s maximal sagittal diameter (sd)
-
sdi: basion-to-anterior bi-interoccipital synchondrosis diameter (sdi)
-
sdio: anterior bi-interoccipital synchondrosis-to-opisthion diameter (sdio)
-
td: the foramen magnum’s maximal transverse diameter (td)
-
tdi: anterior bi-interoccipital synchondrosis width (tdi)
Figure 1 shows these variables on a CT data image.
The growth rate and the total percentage of increase were extrapolated from our data according to the methodology of Richards and Jabbour [22]. To compare Crouzon’s and the control groups, we analyzed the growth rate and the percentage of increase of the first 15 months of life.
For children with Crouzon’s syndrome, we considered the type of exon mutation and the presence of tonsillar prolapsus (TP; defined as cerebellar tonsils herniation >5 mm below the basion–opisthion line) and searched for the presence of an associated hydrocephalus.
Statistical analysis
Head growth occurs in phases. It is neither a linear nor a logarithmic phenomenon [24]. For this reason, a graphical analysis was performed using a lowess (locally weighted scatterplot smoothing) non-parametric regression for each measured value [8, 7]. Best-fit curves were calculated on the scatterplot of each measurement against age using 0.5 as the smoothing parameter. These curves extrapolate the change of the measurements during childhood. All the measurements might not be normally distributed in the pathological condition considered here. We thus used the directional Mann–Whitney–Wilcoxon rank-sum test, which is a non-parametric statistical hypothesis test, to compare the measured parameters in each group using z scores. The alternative hypothesis (control group measurements higher than Crouzon’s) was accepted if the results were considered significant (p ≤ 0.05). For correlations, Pearson chi-square test or likelihood ratio test (for samples <5) were used, with significant results for p ≤ 0.05. All the statistical analyses were performed with R 2.14.1 GUI 1.43 Leopard build 64-bit (5989). The database was exported from IBM SPSS Statistic 20 for mac OS X 10.7.
Results
Tables 1 and 2 show a synopsis of our populations and the results of our analysis, respectively. There were no statistical differences in all these measurements between boys and girls.
Measurements and growth rate
Foramen magnum area
A significant difference was found in the FM area (p = 0.0228, z score = 2). FM area by age of children with Crouzon’s syndrome was stochastically lower than the controls (Fig. 2). The lowess curve of the Crouzon’s group was always situated below the control group line.
By extrapolation, we found two growth phases in the FM area in the control group. During the first phase, from birth to the 36th month of life, the FM area had its maximal increase. A phase of stabilization was observed after the 36th month of life. Two growth phases were also found in the area of FM in the Crouzon’s group. However, the first phase was shorter. In fact, the growth rate broke down in the Crouzon’s group after 18 months of age.
Foramen magnum’s maximal sagittal diameter (sd)
A significant difference was observed between the two groups for the sd value by age (p = 0.0287, z = 1.9), with the lowess curve of the Crouzon’s group situated below the control group (Fig. 3).
The growth pattern of the sd in the control group followed two phases: the first one from birth to 30 months of life with a high growth rate and the second after 30 months of life, where sd growth was stabilized. The sd growth in children with Crouzon’s syndrome followed also two phases: sd was consistently increasing from birth to 58 months, and then its growth rate broke down.
Basion-to-anterior bi-interoccipital synchondrosis diameter (sdi)
No significant difference was found for sdi measurement comparing the two groups by age (p = 0.4247, z = −0.19). Interestingly, around the second year of age in the Crouzon’s group, two populations could be distinguished, one with high values and the second with small sdi values. It is probably for that reason that no difference for sdi in the overall group was found between children with Crouzon’s syndrome and the control children (Fig. 4).
Extrapolating our data, the sdi growth in the control group followed two phases. The first one from birth to 15 months of life had a high growth rate and a second phase, after the 15th month, where sdi was still harmoniously increasing but with a low rate. In particular, the sdi growth in Crouzon’s followed two phases, with the first which is a long period of high growth rate for approximately 24 months and then a second period in which its growth rate diminished.
Anterior bi-interoccipital synchondrosis-to-opisthion diameter (sdio)
A significant difference was observed between the two groups for the sdio value by age group (p = 0.0023, z = 2.84). Crouzon’s sdio diameter distribution by age was stochastically lower than the control group (Fig. 5).
In normal children, the sdio growth rate followed two phases: the first from birth to 32 months of life with a high growth rate and the second after the 32th month where sdio still increased, but slowly. In Crouzon’s group, the sdio diameter’s increase followed also two phases: the first from birth to 58 months of life with a high growth rate and the second after the 58th month when the growth rate broke down.
Foramen magnum’s maximal transverse diameter (td)
No significant difference was found for td measurement comparing the two groups (p = 0.063, z = 1.53; Fig. 6). As for the other parameters, extrapolation of the data showed two phases in growth rate in both control and Crouzon’s group. The td in the control group had a high growth rate during a 41-month first phase, and then it broke down in a second phase. In the Crouzon’s group, the td had a high growth rate during a 15-month first phase. Then, in a second phase, the growth rate decreased.
Anterior bi-interoccipital synchondrosis width (tdi)
No significant difference was found for tdi measurements comparing the two groups (p = 0.4801, z = −0.05; Fig. 7). Consequently, the extrapolation of the growth rate for the control and the Crouzon’s groups showed no difference. Two phases could be observed: the first one from birth to 15 months of life and the second one after the 15th month of life.
Analysis of the growth pattern in the first 15 months of life
When comparing the growth rate in the first 15 months of age (first phase of growth for all measured parameters in both groups), we found that Crouzon’s growth rate was actually higher than the controls for several distances.
The growth rate of the FM area in children with Crouzon’s syndrome was 1.32 times higher than that of the control (16.9 vs. 12.8 mm2/month, respectively). The total increase for the area was 1.46 times higher for the Crouzon’s group (220 vs. 151 %, respectively) during the first 15 months. Nevertheless, the FM area of the Crouzon’s group’s absolute values remained lower than the control group.
Also, for the sagittal diameter (sd) and its two components (sdi and sdio), the growth rate was higher in children with Crouzon’s syndrome. In fact, the growth rate of sd during the first 15 months in the Crouzon’s group was 1.21 times higher than the controls (a 0.34 mm/month rate and a 151 % sd increase in the Crouzon’s group and a 0.28 mm/month rate and a 122 % sd increase in the controls) even if the sd absolute values in the Crouzon’s group remained lower than the control group.
Comparing the sdi, the Crouzon’s group had a 0.21 mm/month growth rate and a 197 % sdi increase, whereas the control group had a 0.13 mm/month rate and a 153 % sdi increase. Comparing the sdio, Crouzon’s group showed a 0.32 mm/month growth rate and a 150 % sdio increase, while the control group had a 0.28 mm/month rate and a 122 % sdio increase. In the first 15 months of life, the growth rate in the Crouzon’s group was 1.15 times higher than the control, and the total increase for the sdio was 1.23 times higher than the control group.
Similarly, during the first 15 months of life, Crouzon’s group’s td growth rate was 2.16 times higher than the controls, and the total increase for td was 1.31 times higher for the Crouzon’s group (0.67 mm/month, 168 % increase in the Crouzon’s group and 0.31 mm/month, 128 % increase in the controls). Only the tdi showed a similar growth rate in both groups between 0.31 and 0.41 mm/months, with an increase in tdi of 148 %.
Hydrocephalus and tonsillar prolapse
Three patients had a hydrocephalus (14.28 % of the children with Crouzon’s syndrome). When comparing the measurements of these three hydrocephalic children with the rest of the Crouzon’s group without hydrocephalus, we found that they had a smaller FM area (p = 0.05; Fig. 8), a smaller td diameter (p = 0.03985), a smaller sd diameter (p = 0.023; Fig. 9), and a smaller sdio diameter (p = 0.0173; Fig. 10), but no difference in sdi diameter (p = 0.54; Fig. 11). Association between hydrocephalus and lambdoid sutures status was not statistically significant (p = 0.853). In one case, hydrocephalus was not associated with tonsillar prolapse (TP). No association between hydrocephalus and TP (p = 0.278) was found.
TP was found in eight children (38.10 %) in our series. No difference in all measurements was observed between these children and the remaining patients without TP. Association between TP and lambdoid sutures status was not statistically significant (p = 0.965).
Genetic testing
Twelve children had the FGFR2 mutation localized on the 10th exon and in nine on the 8th exon. The association between the type of exon mutation and hydrocephalus was not statistically significant (p = 0.368); neither were the association between the type of genetic mutation and TP (p = 0.604), facial retrusion (p = 0.237), cranial synostosis (p = 0.368), and the status of the lambdoid sutures (p = 0.697). Mann–Whitney–Wilcoxon rank-sum test showed no influence of the type of mutation in all the measurements.
Discussion
FM ontogenesis is complex. Experimental data show that the basioccipital and the exooccipital bone derive from the fifth first somites [10, 16]. Embryologic data demonstrate that these two bones are derived from the mesoderm [10, 16]. Whereas their cellular origin is known, their ossification mechanisms are still unclear as both endochondral and membranous bone growth can be observed [15]. FM ventrolateral limits are constituted by the basiocciput and its dorsolateral limits by the exoocciput. These two parts are separated by the anterior interoccipital synchondrosis (AIOS), which is directly implicated in FM growth (Fig. 12).
The results of our study indicate that the normal postnatal growth of the foramen magnum (area) can be subdivided into two main phases: the first one, until 3 years of age, is characterized by a rapid growth and the second, until the complete formation of the structure, by a reduced growth rate. When analyzing the differences in the growth pattern of the sagittal and transverse diameters, we found that the latter showed an increase until 41 months of age and then remained stable, whereas the sagittal diameter showed a fast growth rate until 30 months of age and then continued to grow, though with a reduced rate.
According to Richards and Jabbour [22], the sagittal growth of FM follows four main steps: in the fetal period, the main growth is found at the level of the posterior (dorsal) part of FM that increases faster than the anterior (ventral) part. This situation reverses between birth and 6 months of age when the main growth is ventral. After 6 months, the dorsal part of the FM reduces its growth rate, though continuing to develop slowly to arrest at 1 year of age while the ventral part continues to maintain a high growth rate until age 1. This anterior part of the FM will continue to develop at a slow rate until AIOS fusion, which is around 8 years of age [22].
Using a methodology similar to Richards and Jabbour’s [22], we found different results as in the control group, we observed a faster and more prolonged development of the FM posterior part. In fact, in our study, the growth of the posterior part of the FM (sdio) in the period from birth to 32 months of life occurred at a rate of 0.28 mm/month before stabilizing. The growth rate of the anterior part (sdi) was of 0.13 mm/month and stabilized at 15 months of life. Our observations suggest that the posterior part of the FM plays a key role in normal FM growth.
Comparative analysis of the FM in Crouzon’s vs. control group
We found a smaller area of the FM in children with Crouzon’s syndrome compared to matched controls (p = 0.0228) in all age groups. In particular, the sagittal diameter was reduced (p = 0.0287). The role of the posterior component of the FM was confirmed, with the posterior sagittal diameter (sdio) being especially affected. Actually, the sdio was smaller in the Crouzon’s group than in the control group (p = 0.0023), whereas the anterior part (sdi) was not statistically affected (p = 0.4247). Moreover, in the first 3 months of life, the td was also reduced in children with Crouzon’s syndrome (p = 0.0367). The td growth seemed also to be shorter in duration compared to normal subjects. The combination of these two alterations of FM growth accounts for the smaller FM area of the subjects with Crouzon’s syndrome. However, the growth of the tdi is almost identical in both groups, suggesting that the bone growth that starts at the level of the AIOS is not affected.
By summarizing our data, we identified two phases of growth in both the control and the Crouzon’s group. In the first phase, all the growth parameters showed a fast increase in both groups and then a reduced growth rate in a second phase. The extrapolated growth rate in children with Crouzon’s syndrome is actually higher than in the control group in the first phase, but the size of the FM area and the sd and sdio diameters in these subjects never reach those of the control group. Furthermore, the growth rate during the second phase seems more important in the control compared to the Crouzon’s group. The combination of these findings might explain the small area of the FM in children with Crouzon’s syndrome.
Hydrocephalus
Hydrocephalus is a common phenomenon in subjects with Crouzon’s syndrome. It is found in 30 up to 70 % of the cases [5, 9, 20, 21]. In our study, only 14.28 % of the genetically confirmed Crouzon’s children had hydrocephalus; thus, the actual incidence of such complication might be lower than originally thought on the basis of previous reports which considered series identified on the grounds of mere morphological and radiological observations.
The physiopathology of hydrocephalus in Crouzon’s syndrome is still unclear. Most authors favor two main hypotheses: (1) the “constrictive” theory which takes into account an increased cerebrospinal fluid (CSF) outflow resistance due to a small posterior fossa with prematurely closed lambdoid sutures [3, 4, 9, 13, 26] and (2) the “venous” theory which identifies an impaired CSF absorption due to an augmented venous pressure secondary to jugular foramen stenosis as the most relevant factor [5, 13, 23].
In the group of patients considered for the present study, three presented with hydrocephalus: two of them with both lambdoid sutures closed while the last child having a hydrocephalus despite both lambdoid sutures open. As 11 children of this group had closed lambdoid sutures without hydrocephalus, the relationship between the state of the lambdoid sutures and the presence of hydrocephalus is not evident in this series.
Concerning the effect of FM size, we have observed that the three patients with hydrocephalus all had a smaller FM area compared to the remaining Crouzon’s children. Indeed, they showed a smaller sagittal diameter, especially in its posterior segment (sdio), compared to the other subjects with Crouzon’s syndrome but without hydrocephalus (p = 0.0173; Fig. 10). These data support the hypothesis of Richards and Jabbour [22] who identified these modifications in FM size as a possible cause of a hemodynamic impact on the vascular structures contained within the posterior part of the FM or in close relation to it (the vertebral arteries situated immediately behind AIOS and the jugular bulbous in the jugular foramen, in relation to the dorsolateral part of FM) as well as of a hydrodynamic impact due to the reduced spaces for CSF circulation.
Our three cases with hydrocephalus in whom the size of FM was particularly reduced further support the hypothesis that perturbations in CSF flow at the level of the craniovertebral junction associated with an impaired venous drainage are likely to be the causes of the occurrence of hydrocephalus. In other words, in children with Crouzon’s syndrome, the hydrocephalus would result from a complex interaction of mechanical, hydrodynamic, and hemodynamic factors. Such mixed pathogenesis would account for the variable results of endoscopic third ventriculostomy observed in these patients [12].
Cerebellar tonsils and Crouzon’s syndrome
In this study, caudal herniation of the cerebellar tonsils (TP) was observed in eight children (38.10 %) with Crouzon’s syndrome. Previous studies reported that TP is present in 72.7 % of children with Crouzon’s syndrome [6]. This difference could be explained, as was mentioned above, by the fact that we only included children with Crouzon’s syndrome, which had a genetically confirmed mutation, and excluded cases of Pfeiffer’s syndrome or Jackson–Weiss or oxycephalic patients. In this study, we did not identify any relationship of TP with hydrocephalus. In fact, TP was associated with hydrocephalus in only two of the eight children with caudal herniation of the cerebellar tonsil (p = 0.271).
The occurrence of TP in craniosynostosis has been considered as a result of the growth of hindbrain structures within a small and incompetent posterior cranial fossa due to an early closure of the lambdoid sutures [19, 25]. In our series, however, only five out of the eight children with TP had closed lambdoid sutures. The remaining three patients had a TP with open lambdoid sutures. Consequently, the association between the lambdoid sutures status and TP was not statistically significant (p = 0.965). With regard to the basal sutures, we observed that their closure occurred around 56 months of age in both the Crouzon’s and the control groups (we found a case of early closure in the control group at 31 months of age).
The pathogenic interpretation of the tonsillar herniation in Crouzon’s syndrome remains complex. It is probably different from that of other types of Chiari malformation type I where the FM is enlarged [1, 17] to a degree depending on the extent to which the tonsils have descended [27]. In our study, children with Crouzon’s syndrome have a FM smaller than the control children, and Crouzon’s children with TP have a FM size comparable to that of the other Crouzon’s children without TP.
Study limitations
This study presents some limitations. The size of the studied populations is small; thus, we used a restrictive statistical analysis (Mann–Whitney–Wilcoxon rank-sum test) which reduces the risk of false-positive statistical significant difference. But we might underestimate some existing differences (overestimating the p values). A further bias may be related to the age of the children with Crouzon’s syndrome because the more severely affected children might be diagnosed and given surgical treatment earlier than the mild cases. Only an extrapolation of the growth pattern was carried out because a longitudinal CT-based analysis of the FM growth in unoperated children with Crouzon’s syndrome is not possible.
Conclusions
Our study is the first, to the best of our knowledge, that attempts to describe the FM characteristics in genetically confirmed Crouzon’s children. We could show a difference in FM size and growth pattern between children with Crouzon’s syndrome and normal subjects. In particular, we have evidenced that Crouzon’s children present a smaller FM area, especially in its posterior part. The genetic type of mutation seems to neither influence FM measurements nor Crouzon complications as hydrocephalus or TP. Considering hydrocephalus, it seems statistically associated with a small posterior FM.
References
Bliesener JA, Schmidt LR (1980) Normal and pathological growth of the foramen occipitale magnum shown in the plain radiography. Pediatr Radiol 10(2):65–69
Carinci F, Pezzetti F, Locci P, Becchetti E, Carls F, Avantaggiato A, Becchetti A, Carinci P, Baroni T, Bodo M (2005) Apert and Crouzon syndromes: clinical findings, genes and extracellular matrix. J Craniofac Surg 16(3):361–368
Cinalli G, Chumas P, Arnaud E, Sainte-Rose C, Renier D (1998) Occipital remodeling and suboccipital decompression in severe craniosynostosis associated with tonsillar herniation. Neurosurgery 42(1):66–71, discussion 71–73
Cinalli G, Renier D, Sebag G, Sainte-Rose C, Arnaud E, Pierre-Kahn A (1995) Chronic tonsillar herniation in Crouzon’s and Apert’s syndromes: the role of premature synostosis of the lambdoid suture. J Neurosurg 83(4):575–582
Cinalli G, Sainte-Rose C, Kollar EM, Zerah M, Brunelle F, Chumas P, Arnaud E, Marchac D, Pierre-Kahn A, Renier D (1998) Hydrocephalus and craniosynostosis. J Neurosurg 88(2):209–214
Cinalli G, Spennato P, Sainte-Rose C, Arnaud E, Aliberti F, Brunelle F, Cianciulli E, Renier D (2005) Chiari malformation in craniosynostosis. Childs Nerv Syst 21(10):889–901
Cleveland WS (1979) Robust locally weighted regression and smoothing scatterplots. J Am Stat Assoc 74(368):829–836
Cleveland WS, Devlin SJ (1988) Locally weighted regression: an approach to regression analysis by local fitting. J Am Stat Assoc 83(403):596–610
Collmann H, Sörensen N, Krauss J (2005) Hydrocephalus in craniosynostosis: a review. Childs Nerv Syst 21(10):902–912
Couly GF, Coltey PM, Le Douarin NM (1993) The triple origin of skull in higher vertebrates: a study in quail–chick chimeras. Development 117(2):409
Crouzon O (1912) Dysostose cranio-faciale héréditaire. Bull Mem Soc Med Hop Paris 33:545–555
Di Rocco F, Jucá CE, Arnaud E, Renier D, Sainte-Rose C (2010) The role of endoscopic third ventriculostomy in the treatment of hydrocephalus associated with faciocraniosynostosis. J Neurosurg Pediatr 6(1):17–22
Francis PM, Beals S, Rekate HL, Pittman HW, Manwaring K, Reiff J (1992) Chronic tonsillar herniation and Crouzon’s syndrome. Pediatr Neurosurg 18(4):202–206
Goodrich JT (2005) Skull base growth in craniosynostosis. Childs Nerv Syst 21(10):871–879
Helms JA, Amasha RR, Leucht P (2007) Bone voyage: an expedition into the molecular and cellular parameters affecting bone graft fate. Bone 41(4):479–485
Huang R, Zhi Q, Patel K, Wilting J, Christ B (2000) Contribution of single somites to the skeleton and muscles of the occipital and cervical regions in avian embryos. Anat Embryol 202(5):375–383
Kruyff E, Jeffs R (1966) Skull abnormalities associated with the Arnold Chiari malformation. Acta Radiol Diagn (Stockh) 5:9–24
Milhorat TH, Nishikawa M, Kula RW, Dlugacz YD (2010) Mechanisms of cerebellar tonsil herniation in patients with Chiari malformations as guide to clinical management. Acta Neurochir (Wien) 152(7):1117–1127
Nishikawa M, Sakamoto H, Hakuba A, Nakanishi N, Inoue Y (1997) Pathogenesis of Chiari malformation: a morphometric study of the posterior cranial fossa. J Neurosurg 86(1):40–47
Noetzel MJ, Marsh JL, Palkes H, Gado M (1985) Hydrocephalus and mental retardation in craniosynostosis. J Pediatr 107(6):885–892
Proudman TW, Clark BE, Moore MH, Abbott AH, David DJ (1995) Central nervous system imaging in Crouzon’s syndrome. J Craniofac Surg 6(5):401–405
Richards GD, Jabbour RS (2011) Foramen magnum ontogeny in Homo sapiens: a functional matrix perspective. Anat Rec (Hoboken) 294(2):199–216
Sainte-Rose C, LaCombe J, Pierre-Kahn A, Renier D, Hirsch JF (1984) Intracranial venous sinus hypertension: cause or consequence of hydrocephalus in infants? J Neurosurg 60(4):727–736
Sgouros S, Natarajan K, Hockley AD, Goldin JH, Wake M (1999) Skull base growth in childhood. Pediatr Neurosurg 31(5):259–268
Stovner LJ, Bergan U, Nilsen G, Sjaastad O (1993) Posterior cranial fossa dimensions in the Chiari I malformation: relation to pathogenesis and clinical presentation. Neuroradiology 35(2):113–118
Thompson DN, Harkness W, Jones BM, Hayward RD (1997) Aetiology of herniation of the hindbrain in craniosynostosis. An investigation incorporating intracranial pressure monitoring and magnetic resonance imaging. Pediatr Neurosurg 26(6):288–295
Tubbs RS, Shoja MM, Ardalan MR, Shokouhi G, Loukas M (2008) Hindbrain herniation: a review of embryological theories. Ital J Anat Embryol 113(1):37–46
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Coll, G., Arnaud, E., Selek, L. et al. The growth of the foramen magnum in Crouzon syndrome. Childs Nerv Syst 28, 1525–1535 (2012). https://doi.org/10.1007/s00381-012-1805-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-012-1805-x