Abstract
Purpose
Endoscopic-assisted craniosynostosis surgery is associated with less blood loss and shorter operative times as compared to open surgery. However, in infants who have low circulating blood volumes, the endoscopic approach is still associated with significant blood loss. A major source of blood loss is the bone that is cut during surgery. We discuss the novel use of an ultrasonic bone-cutting device for craniosynostosis surgery, which decreases bone bleeding. This device, which has primarily only been used for spine and skull base surgery, may help reduce blood loss in these infants.
Methods
All patients with single suture craniosynostosis who were operated on with the use of an ultrasonic bone-cutting device were identified. The information retrospectively recorded from patient charts included patient age, suture involved, blood loss, operative times, complications, preoperative hemoglobin, postoperative hemoglobin, length of hospital stay, and follow-up times.
Results
Thirteen patients (12 males, 1 female) underwent surgery with an ultrasonic bone-cutting device during the reviewed period. The average age (±standard deviation) of the patients was 11.8 (±1.6) weeks. Four patients had metopic synostosis and nine patients had sagittal synostosis. The average surgery time was 84 (±13) min. The median (interquartile range) blood loss was 20 (10–70) cc. No patients required blood transfusions. Three patients had dural tears.
Conclusion
We demonstrate the novel use of an ultrasonic bone-cutting device for endoscopic-assisted craniosynostosis surgery. This device limited blood loss while maintaining short operative times for infants with low circulating blood volumes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Craniosynostosis has been described for centuries [14]. Suturectomy or suture release was first introduced as a treatment in the late 1800s [14]. This treatment was largely abandoned because of the high mortality associated with the procedure [14]. In 1971, Tessier [20] developed new techniques to treat craniosynostosis involving removing, remodeling, and stabilizing large segments of the cranium. These treatments, however, were associated with significant blood loss, lengthy operative times, prolonged hospital stays, and significant medical complications [13, 20]. In 1998, Jimenez and Barone [7] developed an endoscopic-assisted approach for suture release followed by orthotic therapy for infants typically <3 months of age. This approach was associated with less blood loss, shorter surgical times, and quicker discharges, without sacrificing cranial remodeling [7].
A significant source of blood loss during endoscopic-assisted suture release surgery occurs during bone removal. In recent years, the development of an ultrasonic bone-cutting device has revolutionized osteotomies in the spine, skull base, and maxillofacial surgeries, among others [4, 5]. This device has the ability to section bone precisely while sparing adjacent soft tissue [4, 5]. Another added benefit is that it may also reduce bone bleeding by promoting coagulation [4, 5]. The reduction in bone bleeding is especially critical for infants with lower circulating blood volumes. We report our early experience with the use of this device for endoscopic-assisted cranial suture release surgery.
Methods
Patient population
All pediatric patients undergoing endoscopic-assisted craniosynostosis surgery with the use of an ultrasonic bone-cutting device (Misonix® BoneScalpel or Depuy Synthes piezoelectric system) were identified from November 2010 to June 2012 (Table 1). The information retrospectively recorded from patient charts included patient age, suture involved, blood loss, operative times, complications, preoperative hemoglobin, postoperative hemoglobin, length of hospital stay, and follow-up times.
Patient selection
Patients 3 months of age or less with single suture craniosynostosis were considered for endoscopic-assisted suture release as previously described [17]. Patients were diagnosed clinically and typically confirmed radiographically with computed tomography scans and/or X-rays.
Surgical technique
Patients were brought to the operating room, induced under general anesthesia, and underwent endotracheal intubation. Patients typically had peripheral intravenous lines, arterial line if possible, and urinary catheter insertions. For metopic sutures, patients were placed supine on a Mayfield horseshoe device, with slight neck flexion. For sagittal sutures, patients were placed in a modified prone or seal position with a Pro Med DORO Multi-Purpose Skull Clamp. All dependent areas were padded with foam.
The surgical procedure is illustrated in Figs. 1 and 2. The surgical site is prepped with a povidone–iodine solution and draped in standard fashion. For metopic sutures, a 3-cm incision is made 1 cm anterior to the anterior fontanelle. For sagittal sutures, two incisions are made: a 3-cm incision is made 1 cm anterior to the lambda and another 3-cm incision was made 1 cm posterior to the anterior fontanelle. A burr hole is made below the incision with a high-speed drill. Bone removal is extended laterally from the burr hole to a width of 3 cm and posteriorly or anteriorly to meet the adjacent fontanelle or suture. The galea is dissected free from the underlying pericranium with the assistance of a 4-mm rigid, 30° angled endoscope (Karl Storz, Germany) equipped with a guard. The galea is dissected the entire length of the suture to be released and with a width >3 cm. The pericranium is left intact in order to mark the bone to be removed for suture release. The pericranium is marked with the use of electrocautery to designate a 3-cm-wide strip of bone overlying the suture.
Illustration demonstrating the use of the ultrasonic bone-cutting device for a patient with sagittal synostosis. Incisions are made in close proximity to the bregma and lambda (1). Burr holes are made just distal to the bregma and just proximal to the lambda (2). A rigid endoscope (3) and the ultrasonic bone-cutting device (4) are used to perform the suture release at a width of 3 cm. Drawing done by Ian Suk, Johns Hopkins University
Use of the ultrasonic bone-cutting device and cottonoid. a A cottonoid is placed between the bone and the dura to protect the dura. b The ultrasonic device is used to make a cut in the bone above the cottonoid. c Illustration demonstrating this process. Drawing done by Ian Suk, Johns Hopkins University
The suture release begins by dissecting the dura from the overlying bone, and half-inch cottonoids are then placed between the bone and the dura at the edges of the suture release (Fig. 2a). With endoscopic assistance, the ultrasonic bone-cutting device is then used to cut the bone in 3- to 4-cm increments along both edges of the suture release above the cottonoids (Fig. 2b). The bone in between the cuts is removed piecemeal with a Leksell rongeur. The cottonoids are then advanced along the edges of the suture release, and the ultrasonic bone cutting and rongeur bone removal is repeated until the suture is completely released (Fig. 3). For metopic sutures, the suture is released from the anterior fontanelle to the nasofrontal suture. For sagittal sutures, the suture is released from the lambda to the anterior fontanelle. In addition, for these patients, four barrel stave osteotomies are created in the parietal bones laterally using mayo scissors. Once the suture has been released, gel foam soaked in thrombin is placed over the suture removal site. The incision is closed with 3–0 vicryl (Ethicon Inc., Somverville, NJ, USA) galeal stitches and 5–0 caprosyn (Covidien, Mansfield, MA, USA) stitches.
Perioperative care
Patients are extubated and placed on a regularly scheduled acetaminophen regimen for pain. They are admitted either to the intensive care unit or intermediate medical care for monitoring and followed by both a neurosurgery and pediatrics team. Patients typically have their hemoglobin levels drawn prior to the start of surgery, following surgery, and on postoperative day 1. Patients are only transfused if they are symptomatic (i.e., tachycardic, hypotensive) or if the hemoglobin levels fall below 6.0. They are typically discharged on postoperative day 1 if they are hemodynamically stable and tolerating oral diets.
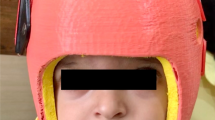
Helmets
Patients are followed at frequent, monthly intervals following surgery with measurements of their cephalic index. The patient is scanned using the infrared STARscanner (Orthoamerica, Orlando, FL, USA) within a week following surgery after swelling has subsided. This information is then used to design a helmet. The patient wears the helmet 23 h per day. New helmets are made and fitted as the infant grows to maintain the desired head shape. The helmets are worn for approximately 9–12 months for sagittal synostosis and 6–9 months for metopic synostosis.
Statistical analysis
Summary data were presented as the mean ± standard deviation for parametric data and as median (interquartile range, IQR) for non-parametric data. Analyses were performed using JMP 9 (SAS Institute, Cary, NC, USA). Values with p < 0.05 were considered statistically significant.
Results
Patient population
Thirteen consecutive patients (12 males, 1 female) underwent endoscopic-assisted suture release with the use of an ultrasonic bone-cutting device during the reviewed period. Nine patients underwent suture release with the use of the Misonix® BoneScalpel and three patients with the Depuy Synthes piezoelectric system. The average age (±standard deviation) of the patients was 11.8 (±1.6) weeks. The average weight was 6.2 (±0.7) kg. Four (31 %) patients had metopic synostosis and nine (69 %) had sagittal synostosis.
Perioperative outcomes
The average surgery time of all patients was 84 (±13) min. The average surgery times for patients with metopic and sagittal synostosis were 74 (±12) and 88 (±11) min, respectively (p = 0.06). The median (IQR) blood loss was 20 (10–70) cc, as estimated by anesthesia. The average starting hemoglobin was 10.5 (±1.3) and the average postoperative hemoglobin was 7.9 (±1.8). The average change in hemoglobin was 3.2 (±1.3). No patients required intraoperative or postoperative blood transfusions. There were no incidences of Doppler changes consistent with air embolism noted.
Three (23 %) patients had dural tears earlier in the series. All three dural tears were repaired primarily. Since consistently placing cottonoids between the dura and bone as described above, we found that the dura remained protected without injury. One patient underwent operative repair of the dural tear to prevent the development of a leptomeningeal cyst as there was a concern the patient may be lost to follow-up after relocating. The average hospital stay was 1.3 (±0.5) days. No patients had infections at a median follow-up time of 4 (1.8–5.7) months.
Discussion
In this series, 13 patients underwent endoscopic-assisted suture release for craniosynostosis with the use of an ultrasonic bone-cutting device. The average operative time was 84 min. The median blood loss was 20 cc; no patients required blood transfusions. There were no incidences of venous air embolisms, and three patients incurred durotomies. The average hospital stay was 1.3 days. There were no infections at a median follow-up time of 4 months.
Endoscopic-assisted suture release surgery has become a viable option for the treatment of craniosynostosis for infants typically <3 months of age. This procedure was first revolutionized by Jimenez and Barone in 1998 [7]. They described the use of a Kerrison rongeur to remove a strip of bone overlying the sagittal suture in four children younger than 3 months of age under endoscopic visualization [7]. All four children had sagittal synostosis, and the average operating time and blood loss were 107 min and 54.2 cc, respectively [7]. This method has been further expanded to treat metopic and coronal synostosis [2, 6, 8, 10]. This procedure has been limited to infants typically <3 months of age because older patients usually have more significant deformational changes that require major craniofacial procedures [1, 3, 9, 12, 17]. Additionally, the bone in older infants has mineralized more, thus making it less malleable to helmet therapy [1, 3, 9, 12, 17]. Younger patients, especially those <3 months of age, have lower circulating blood volumes and are less tolerant to blood loss [18]. Open procedures are associated with significant blood loss from large bicoronal skin incisions, extensive scalp mobilization, bone removal, and long operative times [10, 11, 16]. Endoscopic procedures aim to reduce blood loss by decreasing the length of skin incisions, amount of scalp mobilization, and operative times [10, 11, 16]. Blood loss from bone removal, however, remains constant regardless of open or endoscopic procedure.
A method of decreasing blood loss from bone removal without sacrificing the operating time would further advance endoscopic-assisted surgery for craniosynostosis. In recent years, there has been development of an ultrasonic bone-cutting device [4, 5]. This device was originally designed for bone removal during laminectomy surgery and engages the bone through ultrasonic oscillations, allowing for controlled cuts in the bone [4, 5]. Based on these ultrasonic oscillations, hard tissue or bone is cut and soft tissue is preferentially spared [4, 5]. An added benefit is that this device also coagulates the bone, thus reducing blood loss [4, 5]. Reports of this device have been limited to the spine, skull base, and maxillofacial surgeries [4, 5]. Studies on its efficacy in craniosynostosis surgery have not yet been reported.
The use of this bone-cutting device appears to minimize bleeding from the bone. The median blood loss in this study was only 20 cc, which is on the lower range of reported values [8, 15, 19]. While blood loss in this series was estimated and thus subject to error, none of the patients in this study required any blood transfusions as compared to other endoscopic-assisted studies [8, 15, 19]. This reduced bleeding may also translate into decreased operative times.
A potential complication of this device is unintended durotomy. These occurred in three cases and were able to be repaired with single interrupted sutures, except in one case. These durotomies also occurred early on in our series. We have adapted our technique by placing cottonoids underneath the site of bone cutting. These cottonoids provide a layer of protection to the dura as well as wick away blood. Since adopting this technique, we have had no durotomies. However, it should be noted that even though this instrument typically does not cut soft tissue, dural tears can still happen, especially in young infants with thin dura.
This is the first study to report the use of an ultrasonic bone-cutting device for suture release during craniosynostosis surgery. This device was employed in 13 patients with metopic or sagittal craniosynostosis, with small amount of blood loss and relatively short surgical times. This study, however, was limited to infants with metopic and sagittal craniosynostosis and may not necessarily be applicable to other craniosynostosis subtypes. These infants were also typically <3 months old. However, it seems likely that this ultrasonic bone-cutting device can also be effectively applied to endoscopic coronal craniosynostosis as well as possibly open craniofacial reconstructive surgery in older patients. Further studies are needed to evaluate the role of this device in other craniosynostosis surgeries.
Conclusion
Endoscopic-assisted suture release surgery for craniosynostosis has become a standard approach for infants who present early with single suture craniosynostosis. This approach is associated with decreased blood loss and shorter operative times than open surgery, with similar cranial remodeling results after cranial orthosis. However, blood loss in young infants with this endoscopic approach is still significant, with frequent need for blood transfusions. We report the novel use of an ultrasonic bone-cutting device to facilitate bone cutting with minimal blood loss. This device, which has been primarily limited to spine and skull base surgery, may also be effectively used for craniosynostosis.
References
Barone CM, Jimenez DF (1999) Endoscopic craniectomy for early correction of craniosynostosis. Plast Reconstr Surg 104:1965–1973, discussion 1974–1965
Barone CM, Jimenez DF (2004) Endoscopic approach to coronal craniosynostosis. Clin Plast Surg 31:415–422, vi
Berry-Candelario J, Ridgway EB, Grondin RT, Rogers GF, Proctor MR (2011) Endoscope-assisted strip craniectomy and postoperative helmet therapy for treatment of craniosynostosis. Neurosurg Focus 31:E5
Beziat JL, Bera JC, Lavandier B, Gleizal A (2007) Ultrasonic osteotomy as a new technique in craniomaxillofacial surgery. Int J Oral Maxillofac Surg 36:493–500
Bruggers S, Sindwani R (2009) Evolving trends in powered endoscopic sinus surgery. Otolaryngol Clin North Am 42:789–798, viii
Cartwright CC, Jimenez DF, Barone CM, Baker L (2003) Endoscopic strip craniectomy: a minimally invasive treatment for early correction of craniosynostosis. J Neurosci Nurs 35:130–138
Jimenez DF, Barone CM (1998) Endoscopic craniectomy for early surgical correction of sagittal craniosynostosis. J Neurosurg 88:77–81
Jimenez DF, Barone CM, Cartwright CC, Baker L (2002) Early management of craniosynostosis using endoscopic-assisted strip craniectomies and cranial orthotic molding therapy. Pediatrics 110:97–104
Jimenez DF, Barone CM (2007) Early treatment of anterior calvarial craniosynostosis using endoscopic-assisted minimally invasive techniques. Childs Nerv Syst 23:1411–1419
Jimenez DF, Barone CM (2010) Endoscopic techniques for craniosynostosis. Atlas Oral Maxillofac Surg Clin North Am 18:93–107
Johnson JO, Jimenez DF, Barone CM (2000) Blood loss after endoscopic strip craniectomy for craniosynostosis. J Neurosurg Anesthesiol 12:60
MacKinnon S, Rogers GF, Gregas M, Proctor MR, Mulliken JB, Dagi LR (2009) Treatment of unilateral coronal synostosis by endoscopic strip craniectomy or fronto-orbital advancement: ophthalmologic findings. J Aapos 13:155–160
Marchac D, Renier D, Broumand S (1994) Timing of treatment for craniosynostosis and facio-craniosynostosis: a 20-year experience. Br J Plast Surg 47:211–222
Mehta VA, Bettegowda C, Jallo GI, Ahn ES (2010) The evolution of surgical management for craniosynostosis. Neurosurg Focus 29:E5
Meier PM, Goobie SM, DiNardo JA, Proctor MR, Zurakowski D, Soriano SG (2011) Endoscopic strip craniectomy in early infancy: the initial five years of anesthesia experience. Anesth Analg 112:407–414
Persing J, Babler W, Winn HR, Jane J, Rodeheaver G (1981) Age as a critical factor in the success of surgical correction of craniosynostosis. J Neurosurg 54:601–606
Proctor MR (2012) Endoscopic cranial suture release for the treatment of craniosynostosis—is it the future? J Craniofacial Surg 23:225–228
Riley AA, Arakawa Y, Worley S, Duncan BW, Fukamachi K (2010) Circulating blood volumes: a review of measurement techniques and a meta-analysis in children. ASAIO J 56:260–264
Shah MN, Kane AA, Petersen JD, Woo AS, Naidoo SD, Smyth MD (2011) Endoscopically assisted versus open repair of sagittal craniosynostosis: the St. Louis Children’s Hospital experience. J Neurosurg Pediatr 8:165–170
Tessier P (1971) Relationship of craniostenoses to craniofacial dysostoses, and to faciostenoses: a study with therapeutic implications. Plast Reconstr Surg 48:224–237
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chaichana, K.L., Jallo, G.I., Dorafshar, A.H. et al. Novel use of an ultrasonic bone-cutting device for endoscopic-assisted craniosynostosis surgery. Childs Nerv Syst 29, 1163–1168 (2013). https://doi.org/10.1007/s00381-013-2043-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-013-2043-6