Abstract
Introduction
Surgery for craniosynostosis remains a crucial element in successful management. Intervention by both endoscopic and open approaches has been proven effective. Given the differences in timing and indications for these procedures, differences in perioperative outcomes have yet to be thoroughly compared between the two approaches. The aim of the systematic review and meta-analysis was to assess the available evidence of perioperative outcomes between the two approaches in order to better influence the management paradigm of craniosynostosis.
Methods
We followed recommended PRISMA guidelines for systematic reviews. Seven electronic databases were searched to identify all potentially relevant studies published from inception to February 2018 which were then screened against a set of selection criteria. Data were extracted and analyzed using meta-analysis of proportions.
Results
Twelve studies satisfied all the selection criteria to be included, which described a pooled cohort involving 2064 craniosynostosis patients, with 965 (47%) and 1099 (53%) patients undergoing surgery by endoscopic and open approaches respectively. When compared to the open approach, it was found that the endoscopic approach conferred statistically significant reductions in blood loss (MD = 162.4 mL), operative time (MD = 112.38 min), length of stay (MD = 2.56 days), and rates of perioperative complications (OR = 0.58), reoperation (OR = 0.37) and transfusion (OR = 0.09), where all p < 0.001.
Conclusion
Both endoscopic and open approaches for the surgical management of craniosynostosis are viable considerations. The endoscopic approach confers a significant reduction in operative and postoperative morbidity when compared to the open approach. Given that specific indications for either approach should be considered when managing a patient, the difference in perioperative outcomes remain an important element of this paradigm. Future studies will validate the findings of this study and consider long-term outcomes, which will all contribute to rigor of craniosynostosis management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Craniosynostosis, defined as premature closure of a cranial suture, occurs in 1:2000 to 1:2500 living births [2, 4]. Surgical correction is often warranted to achieve a normal head shape and also to prevent risks such as neurocognitive sequelae posed by increased intracranial pressure. Diverse spectrums of surgical techniques have evolved with time to treat craniosynostosis. Strip craniectomy was initially introduced by Lannelongue [18] and Lane [17] in the 1890s with the aim of preserving intellectual function but better cosmesis was found with open calvarial vault reconstruction [24]. More recently, there has been a renewed interest in craniectomy procedures due to availability of minimally invasive endoscopic procedures characterized by lower blood loss, operative time, and length of stay with acceptable long-term anthropometric outcomes since it is performed early in life [5, 8, 10, 26]. Postoperatively, molding helmet therapy is typically required to obtain good long-term cosmetic results with endoscopic treatment [26].
Many series have characterized perioperative outcomes following endoscopic and open repair of craniosynostosis [26]. A consolidated review of complications and reoperations following either technique is lacking in the literature. Also, no large-scale literature review has focused on evaluating these reports to assess quality of evidence comparing the two approaches. We aimed to perform a systematic review and meta-analysis comparing endoscopic and open craniosynostosis correction primarily with the objective of characterizing perioperative outcomes such as blood loss, operative time, length of stay, complication, reoperation, and transfusion rates following the procedure and provide recommendations using the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach [3].
Methods
Literature search strategy
Our systematic review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [21]. The literature search strategy was designed around the PICO format—Is there a difference in surgical outcomes (outcome) between patients undergoing minimally invasive surgery (population of interest) and patients undergoing open surgery (comparison) following craniosynostosis correction (intervention)? Electronic searches were performed using Ovid Medline, PubMed, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, American College of Physicians Journal Club, and Database of Abstracts of Review of Effectiveness from their dates of inception to February 2018 by two independent reviewers (A.G. and V.M.L.). We combined the search terms “craniosynostosis,” “minimally invasive,” “endoscopic,” “open,” “strip craniectomy,” “calvarial reconstruction,” “sagittal,” and “metopic” as either keywords or MeSH terms. In addition, we reviewed the list of references from retrieved articles for identification of potentially relevant studies.
Selection criteria
The inclusion criteria used to screen all identified articles were the following: (1) original studies in human subjects, written in the English language; (2) distinct discernible cohorts of patients undergoing minimally invasive and open craniosynostosis repair in the same study; and (3) greater than 10 patients in each of the two groups. Studies were excluded if (a) lacking direct comparison between minimally invasive and open procedures, (b) no relevant outcomes were reported; and (c) among duplicate studies by the same institution with an accumulated number of patients or extended follow-up, only the most complete and updated reports were selected for quantitative synthesis. Reviews and editorials were also excluded. To minimize methodological heterogeneity, we only included studies which reported use of endoscopic-assisted minimally invasive procedures.
Data extraction and critical appraisal
All data were extracted from article texts, tables, and figures with any estimates made based on the presented data and figures. Two investigators (A.G. and V.M.L.) independently reviewed each included article, any discrepancy resolved by discussion to reach consensus. Primary outcomes of interest consisted of (a) reoperations, (b) perioperative complications (both intraoperative and postoperative complications), and (c) transfusion rates while secondary outcomes included perioperative parameters such as (a) estimated blood loss (EBL), (b) operative time, and (c) length of stay (LOS).
Risk of bias in each study was evaluated using the Newcastle-Ottawa Scale (NOS) [6]. Overall confidence in the estimates for each outcome was assessed based on the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) Working Group system for limitations in study design, evidence directness, consistency, precision of results, and publication bias [3]. The GRADEpro Guideline Development Tool (GDT) was employed to generate a Summary of Findings (SoF) table (https://gradepro.org/). In case a large effect size (defined as RR > 2 for categorical outcomes and standardized mean difference > 0.8 for continuous outcomes) was observed, strength of evidence was upgraded by one level.
Statistical analysis
Odds ratios (OR) and mean differences (MD) were used as summary statistics for dichotomous and continuous outcomes, respectively. Meta-analyses for all outcomes were presented as forest plots with summary statistical estimates, 95% confidence intervals, and relative weights represented by the middle of the square, the horizontal line, and the relative size of the square, respectively. For the overall summary statistic, the mean and 95% confidence interval were represented by the middle and width of the diamond, respectively. The I2 statistic was used to estimate heterogeneity across studies, with values greater than 50% considered as substantial heterogeneity. It can be calculated as I2 = 100% × (Q − df)/Q, with Q defined as Cochrane’s heterogeneity statistics and df defined as degrees of freedom. In the present meta-analysis, we used a random-effects model in order to take into account the methodological variation across studies. Leave-one out sensitivity analysis was performed when cohort size bias was suspected. Each study was sequentially removed, and the overall trend reassessed for any significant change. All p values were two-sided. All statistical analyses were conducted using Review Manager version 5.3.3 (Cochrane Collaboration, Software Update, Oxford, UK).
Results
Study characteristics
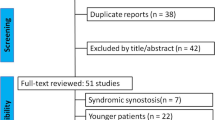
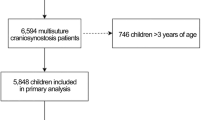
Our search yielded a total of 500 articles following which 278 were selected for screening following removal of duplicates and non-English reports. Following screening, 35 were selected for full-text evaluation and 12 studies [1, 2, 5, 8, 10, 16, 23, 26, 27, 29,30,31] were included in the final qualitative and quantitative synthesis (Fig. 1). All included studies were either retrospective (n = 10) or prospective (n = 2) observational in design. Most of the studies were from the USA (n = 9) while others were published from the Netherlands (n = 2) and Canada (n = 1). Table 1 summarizes characteristics of included studies.
Cohort description
A total of 2064 patients were included with 965 patients undergoing minimally invasive procedures. Sex distribution was reported in nine studies (n = 1537), out of 68% (n = 1055) were males. A majority of the studies (n = 5) focused on sagittal craniosynostosis only while the rest reported outcomes for metopic (n = 2), lambdoid (n = 1), or multiple different synostotic cranial sutures (n = 4). Eight studies (n = 1673) compared endoscopic procedures to open calvarial vault reconstruction while one study (n = 35) used strip craniectomy and another (n = 300) reported both calvarial vault reconstruction and open strip craniectomy as comparison. Two studies (n = 356) did not specify the type of open craniosynostosis surgery performed. Endoscopic procedures were mostly performed in case of early presentation (age < 6 months) with mean age of cohort ranging between 2.9 and 5.3 months while the mean age for open procedures ranged between 5 and 29.5 months with only study (Thompson et al. [27]) reporting a cohort of patients < 6 months of age (mean age 5 months) undergoing open procedures (after propensity score matching). Table 2 summarizes cohort characteristics.
Primary outcomes
Perioperative complications
A significantly lower complication rate was found with endoscopic procedures than open repair based on six studies (n = 1872). (OR = 0.58, CI = 0.44–0.75, p < 0.001, I2 = 0%) (Fig. 2a).
Reoperations
Compared to open surgery, endoscopic correction was associated with a significantly lower reoperation rate based on three studies (n = 815, OR = 0.37, CI = 0.18–0.75, p = 0.006, I2 = 0%) (Fig. 2b). A total of 12 reoperations were performed in the endoscopic group for cosmetic reasons (n = 6), bone defects (n = 4), CSF leak (n = 1), and recurrent synostosis (n = 1). In the open surgery group, a total of 38 revisions were performed for cosmetic reasons (n = 9), bone defects (n = 8), recurrent synostosis (n = 8), wound infection (n = 4), implant removal (n = 3), raised ICP (n = 2), and hematomas (n = 2).
Transfusion rate
Based on seven studies (n = 1600), endoscopic correction necessitated a significantly lesser transfusion requirement as reflected in the lower transfusion incidence as compared to open procedures (OR = 0.09, CI = 0.03–0.26, p < 0.001, I2 = 84%) (Fig. 2c).
Secondary outcomes
Estimated blood loss (mL)
Blood loss was reported by eight studies (n = 1041), significantly lower surgical blood loss was found with endoscopic surgery than open repair (MD = 162.40, CI = 79.28–245.51, p < 0.001, I2 = 0%) (Fig. 3a).
Operative time (minutes)
Based on nine studies (n = 1812), operative time was considerably shorter with endoscopic repair than open surgery (MD = 112.38, CI = 88.64–136.12, p < 0.001, I2 = 97%) (Fig. 3b).
Length of stay (days)
Analysis of nine studies (n = 1837) reporting length of stay (LOS) revealed a significantly shorter length of hospital stay with endoscopic procedures compared to open surgery (MD = 2.56, CI = 1.89–3.23, p < 0.001, I2 = 97%) (Fig. 3c).
Quality assessment
Study quality was evaluated using the Newcastle-Ottawa Scale (NOS) [6]. A medium to high quality was observed for all studies included in this meta-analysis [Supplemental table 1]. Strength of evidence for all outcomes evaluated using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach was very low. (Table 3). With the exception of complications, strength of evidence for all outcomes was upgraded by one level because of a large effect size (defined as RR > 2 for categorical outcomes and SMD > 0.8 for continuous outcomes).
Discussion
Endoscopic-assisted craniosynostosis surgery was introduced in the 1990s by Jimenez and Barone [12,13,14,15, 19]. It remains a relatively newer technique with limited experience reported in the literature. The main goal is to minimize perioperative morbidity while achieving similar functional and cosmetic outcomes.
In the present systematic review and meta-analysis, we found superior perioperative performance of minimally invasive endoscopic surgery compared to open surgery. Pooled estimates revealed a lower complication rate following endoscopic procedures. In their retrospective study of 35 patients, van Nunen et al. found that endoscopic surgery simplified anesthesia practice on account of anticipation of increased hemodynamic stability and thereby, reducing the need for invasive monitoring by arterial cannulation [29]. Tobias et al. noted that a lower incidence of venous air embolism was observed with endoscopic surgery primarily attributable to a lower blood loss leading to a lower propensity to have noncompressible veins exposed to air [28]. Intraoperative durotomies have also been found to be lower with endoscopic approaches [2, 5, 10]. Also, of interest to note was the significantly lower reoperation and blood transfusion rate. These results have been shown to be consistent across both nonsyndromic and syndromic cases of craniosynostosis [10]. Most studies support a significantly lower intraoperative complication rate while a modest benefit has been noted in terms of incidence of postoperative complications [10, 26]. Several studies have demonstrated lower hospital costs with endoscopic approaches despite the costs incurred due to postoperative orthotic therapy [5, 8, 11, 30]. This might be indirectly due to a lower length of hospital stay and lesser transfusion requirements as found in this study. The lower perioperative morbidity also avoids the costs associated with stay in an intensive care unit [30]. According to the multicenter evaluation by Thompson et al., a majority of participating centers (60%) did not practice intensive care admissions after endoscopic surgery [27].
While this review focuses primarily on perioperative safety and efficacy, long-term anthropometric outcomes with endoscopic-assisted surgery are also said to be equivalent to open calvarial reconstruction [7, 20, 23, 26]. This is an important consideration in determining the optimal approach in a craniosynostosis patient at presentation. In their retrospective review of 89 patients with sagittal craniosynostosis, Shah et al. [26] found mean cephalic index at the last follow-up to be equivalent between the two groups. However, significantly longer follow-up was noted in the open group compared to the endoscopic group (24 vs 13 months). In another review of 46 patients with sagittal craniosynostosis by Le et al., no significant differences were found in mean cranial index at 24 months between endoscopic and open surgery patients [20]. Surgical technique was not determined to be a significant factor in postrepair anthropometric outcome. Literature on metopic craniosynostosis is largely insufficient to suggest equivalence or non-inferiority of the endoscopic technique over open repair; however, emerging results are encouraging. Nguyen et al. demonstrated similar postoperative measurements following endoscopic and open repair in a series of 28 patients with nonsyndromic metopic craniosynostosis despite worse hypertelorism in the endoscopic group (n = 13) at baseline [23].
Compared to open procedures, endoscopic suturectomies were performed at a significantly younger age with most authors preferring the procedure only at an age of presentation less than 6 months [1, 2, 5, 7,8,9,10, 16, 20, 23, 26, 27, 30]. While surgery at a younger age could potentially be associated with a higher complication rate, the lower blood loss and surgical time with a minimally invasive procedure seemed to compensate for the morbidity of an operative intervention in a young patient. According to available anthropometric evaluations, age of repair is a significant predictor of improvement in cranial measurements [20, 23]. Success of endoscopic correction is often attributed to the younger age of suturectomy, allowing cranial remodeling with brain development [23, 26]. The younger age of intervention warrants postoperative helmet therapy to “mold” the steep calvarial bone growth. In contrast, since open procedures are performed at an older age, postoperative molding therapy is deferred to due to decline in the rate of bone development.
It is important to note, that a successful long-term outcome with endoscopic repair is critically dependent on postoperative molding with helmet (orthotic) therapy to augment cranial index [23, 26], although its exact recommended duration remains under investigation [13, 22, 25]. The addition of orthotic use has not been demonstrated to significantly increase costs [5, 8, 30]. Although complications related to orthotic therapy (such as alopecia) have been said to be insignificant [26], compliance with the regimen remains a significant challenge to be observed. Therefore, caregiver socioeconomic characteristics that determine compliance need to be taken into consideration during preoperative counseling and individually tailored decision-making.
Limitations
This review was marked by several limitations. First, the impact of age as a confounding factor to determine outcomes between the two groups could not be assessed. However, randomizing patients into endoscopic or open groups would not be ethically possible given the different recommended ages for each procedure. In such a scenario, propensity-matched comparisons could be useful. Only one study in our review [27] employed propensity matching. Second, no prospective randomized comparisons were available with most included studies being single-institutional retrospective reviews, thereby, lowering study quality and strength of evidence, as shown by our overall GRADE estimates. However, large effect sizes were observed for all analyzed outcomes with the exception of complications. Third, the significantly shorter duration of follow-up in patients undergoing endoscopic repair in some studies could have been an important confounding factor for the lower reoperation rate seen in these patients [8, 10]. Fourth, due to limited availability within current literature, long-term anthropometric outcomes could not be quantitatively compared between the two types of procedures. Fifth, the difference in outcomes between the two techniques could not be stratified by the syndromic or nonsyndromic nature of the disease. Sixth, subgroup comparisons could not be performed to account for variations in technique of open repair–total calvarial reconstruction, modified pi repair, etc. Thus, collectively, the current data in the literature remains weak. Nonetheless, strict adherence to the selection criteria, assessment for heterogeneity and subsequent use of remodeling when implicated, exclusion of single-arm case series, and thorough quality assessment with the GRADE tool allows us to provide the most valid comparison within the literature possible to date.
Directions for future investigations
While randomized comparisons would be ideal, but since they are harder to obtain, propensity-matched studies could be a useful alternative to account for age differences between patients undergoing either technique. Despite encouraging early results with anthropometric evaluations, more studies comparing such outcomes between the two techniques with a sufficient duration of follow-up are needed. More studies are also needed to evaluate outcomes following corrections for different types of craniosynostosis, since most of the literature at present is focused on the sagittal type. A longer duration of follow-up evaluation is required with endoscopic surgery to better assess its long-term complication and reoperation profile and allow a fair comparison with open reconstruction. Challenges associated with postoperative orthotic use also need to be investigated. Cost-directed investigations from varied practice settings would also welcome additions to the literature. At present, evidence for efficacy of endoscopic repair is largely available for nonsyndromic variants of craniosynostosis [2], obviating further studies comparing the two types of procedures for syndromic cases as well. Efforts must also be made to identify if there is a learning curve associated with the technique, although none yet has been acknowledged so far [2].
Conclusion
Early correction of craniosynostosis with minimally invasive endoscopic-assisted techniques might be associated with lower perioperative morbidity, transfusion rate, and costs and non-inferior long-term improvement in cranial indices as compared to open surgery. These findings emphasize the need for early referral to a comprehensive craniofacial center in suspected cases of craniosynostosis as perioperative outcomes may be most optimized. Further prospectively randomized or propensity-matched comparisons with adequate duration of follow-up are required to validate these findings and elucidate the role of endoscopic surgery in craniosynostosis correction.
Abbreviations
- GRADE:
-
Grading of Recommendations Assessment
Development and Evaluation
- NOS:
-
Newcastle-Ottawa Scale
- OR:
-
Odds ratio
- RR:
-
Relative risk
- MD:
-
Mean difference
- SMD:
-
Standardized mean difference
References
Abbott MM, Rogers GF, Proctor MR, Busa K, Meara JG (2012) Cost of treating sagittal synostosis in the first year of life. J Craniofac Surg 23:88–93
Arts S, Delye H, van Lindert EJ (2018) Intraoperative and postoperative complications in the surgical treatment of craniosynostosis: minimally invasive versus open surgical procedures. J Neurosurg Pediatr 21:112–118
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S et al (2004) Grading quality of evidence and strength of recommendations. BMJ 328:1490
Bonfield CM, Sharma J, Cochrane DD, Singhal A, Steinbok P (2016) Minimizing blood transfusions in the surgical correction of craniosynostosis: a 10-year single-center experience. Childs Nerv Syst 32:143–151
Chan JWH, Stewart CL, Stalder MW, St Hilaire H, McBride L, Moses MH (2013) Endoscope-assisted versus open repair of craniosynostosis: a comparison of perioperative cost and risk. J Craniofac Surg 24:170–174
Cook DA, Reed DA (2015) Appraising the quality of medical education research methods: the Medical Education Research Study Quality Instrument and the Newcastle-Ottawa Scale-Education. Acad Med 90:1067–1076
Farber SJ, Nguyen DC, Skolnick GB (2017): Anthropometric outcome measures in patients with metopic craniosynostosis. Journal of: Available: https://journals.lww.com/jcraniofacialsurgery/Abstract/2017/05000/Anthropometric_Outcome_Measures_in_Patients_With.32.aspx
Garber ST, Karsy M, Kestle JRW, Siddiqi F, Spanos SP, Riva-Cambrin J (2017) Comparing outcomes and cost of 3 surgical treatments for sagittal synostosis: a retrospective study including procedure-related cost analysis. Neurosurgery 81:680–687
Ghenbot RG, Patel KB, Skolnick GB, Naidoo SD, Smyth MD, Woo AS (2015) Effects of open and endoscopic surgery on skull growth and calvarial vault volumes in sagittal synostosis. J Craniofac Surg 26:161–164
Han RH, Nguyen DC, Bruck BS, Skolnick GB, Yarbrough CK, Naidoo SD, Patel KB, Kane AA, Woo AS, Smyth MD (2016) Characterization of complications associated with open and endoscopic craniosynostosis surgery at a single institution. J Neurosurg Pediatr 17:361–370
Hinojosa J, Esparza J, Muñoz MJ (2007) Endoscopic-assisted osteotomies for the treatment of craniosynostosis. Childs Nerv Syst 23:1421–1430
Jimenez DF, Barone CM (2012) Bilateral endoscopic craniectomies in the treatment of an infant with Apert syndrome. J Neurosurg Pediatr 10:310–314
Jimenez DF, Barone CM (1998) Endoscopic craniectomy for early surgical correction of sagittal craniosynostosis. J Neurosurg 88:77–81
Jimenez DF, Barone CM, Cartwright CC, Baker L (2002) Early management of craniosynostosis using endoscopic-assisted strip craniectomies and cranial orthotic molding therapy. Pediatrics 110:97–104
Jimenez DF, Barone CM, McGee ME, Cartwright CC, Baker CL (2004) Endoscopy-assisted wide-vertex craniectomy, barrel stave osteotomies, and postoperative helmet molding therapy in the management of sagittal suture craniosynostosis. J Neurosurg Pediatr 100:407–417
Keshavarzi S, Hayden MG, Ben-Haim S, Meltzer HS, Cohen SR, Levy ML (2009) Variations of endoscopic and open repair of metopic craniosynostosis. J Craniofac Surg 20:1439–1444
Lane LC (1892) Pioneer craniectomy for relief of mental imbecility due to premature sutural closure and microcephalus. JAMA XVIII:49–50
Lannelongue M (1890) De La Craniectomie Dans La Microcephalie. CR Seances Acad Sci 110:1382
Lee HQ, Hutson JM, Wray AC, Lo PA, Chong DK, Holmes AD, Greensmith AL (2012) Analysis of morbidity and mortality in surgical management of craniosynostosis. J Craniofac Surg 23:1256–1261
Le M-B, Patel K, Skolnick G, Naidoo S, Smyth M, Kane A et al (2014) Assessing long-term outcomes of open and endoscopic sagittal synostosis reconstruction using three-dimensional photography. J Craniofac Surg 25:573–576
Liberati A, Tetzlaff J, Altman DG, Group P 2009 Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Available: http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000097, 6, e1000097
Murad G, Clayman M, Seagle MB, White S: Endoscopic-assisted repair of craniosynostosis. Neurosurgical:2005 Available: http://thejns.org/doi/abs/10.3171/foc.2005.19.6.7
Nguyen DC, Patel KB, Skolnick GB, Naidoo SD, Huang AH, Smyth MD, Woo AS (2015) Are endoscopic and open treatments of metopic synostosis equivalent in treating trigonocephaly and hypotelorism? J Craniofac Surg 26:129–134
Panchal J, Marsh JL, Park TS, Kaufman B, Pilgram T, Huang SH (1999) Sagittal craniosynostosis outcome assessment for two methods and timings of intervention. Plast Reconstr Surg 103:1574–1584
Seymour-Dempsey K, Baumgartner JE, Teichgraeber JF, Xia JJ, Waller AL, Gateno J (2002) Molding helmet therapy in the management of sagittal synostosis. J Craniofac Surg 13:631–635
Shah MN, Kane AA, Petersen JD, Woo AS, Naidoo SD, Smyth MD (2011) Endoscopically assisted versus open repair of sagittal craniosynostosis: the St. Louis Children’s Hospital experience. J Neurosurg Pediatr 8:165–170
Thompson DR, Zurakowski D, Haberkern CM, Stricker PA, Meier PM, Bannister C, Benzon H, Binstock W, Bosenberg A, Brzenski A, Budac S, Busso V, Capehart S, Chiao F, Cladis F, Collins M, Cusick J, Dabek R, Dalesio N, Falcon R, Fernandez A, Fernandez P, Fiadjoe J, Gangadharan M, Gentry K, Glover C, Goobie S, Gries H, Griffin A, Groenewald CB, Hajduk J, Hall R, Hansen J, Hetmaniuk M, Hsieh V, Huang H, Ingelmo P, Ivanova I, Jain R, Koh J, Kowalczyk-Derderian C, Kugler J, Labovsky K, Martinez JL, Mujallid R, Muldowney B, Nguyen KP, Nguyen T, Olutuye O, Soneru C, Petersen T, Poteet-Schwartz K, Reddy S, Reid R, Ricketts K, Rubens D, Skitt R, Sohn L, Staudt S, Sung W, Syed T, Szmuk P, Taicher B, Tetreault L, Watts R, Wong K, Young V, Zamora L, Pediatric Craniofacial Collaborative Group (2018) Endoscopic versus open repair for craniosynostosis in infants using propensity score matching to compare outcomes: a multicenter study from the pediatric craniofacial collaborative group. Anesth Analg 126:968–975
Tobias JD, Johnson JO, Jimenez DF, Barone CM, McBride DS Jr (2001) Venous air embolism during endoscopic strip craniectomy for repair of craniosynostosis in infants. Anesthesiology 95:340–342
van Nunen DPF, Stubenitsky BM, Woerdeman PA, Han KS, Breugem CC, Mink van der Molen AB et al (2016) Minimally invasive strip craniectomy simplifies anesthesia practice in patients with isolated sagittal synostosis. J Craniofac Surg 27:1985–1990
Vogel TW, Woo AS, Kane AA, Patel KB, Naidoo SD, Smyth MD (2014) A comparison of costs associated with endoscope-assisted craniectomy versus open cranial vault repair for infants with sagittal synostosis. J Neurosurg Pediatr 13:324–331
Zubovic E, Woo AS, Skolnick GB, Naidoo SD, Smyth MD, Patel KB (2015) Cranial base and posterior cranial vault asymmetry after open and endoscopic repair of isolated lambdoid craniosynostosis. J Craniofac Surg 26:1568–1573
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No funding sources or conflicts of interest to disclose.
Electronic supplementary material
Supplemental table 1
(DOCX 78.7 kb)
Rights and permissions
About this article
Cite this article
Goyal, A., Lu, V.M., Yolcu, Y.U. et al. Endoscopic versus open approach in craniosynostosis repair: a systematic review and meta-analysis of perioperative outcomes. Childs Nerv Syst 34, 1627–1637 (2018). https://doi.org/10.1007/s00381-018-3852-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3852-4