Abstract
Objectives of the study were to examine the long-term prognostic power of coronary computed tomography angiography (CCTA) to predict death or myocardial infarction in patients with diabetes mellitus (DM). The prognostic value of CCTA in diabetic patients has been confirmed for short- and intermediate follow-up durations. The slowly progressing nature of coronary artery disease (CAD), however, underlines the necessity to validate CCTA for longer observation periods in this high-risk population. A total of 132 patients with DM and 1781 without DM were examined by CCTA and followed for a median duration of 9.7 (IQR 6.9, 11.2) and 9.9 (IQR 6.9, 11.1) years, respectively. Cox proportional hazards analysis was used for the composite endpoint of death and myocardial infarction. Warranty period was defined as the number of years that an individual stays in a low-risk group with a cumulative probability for the endpoint below 1% and calculated for patients with/without DM and rising degrees of CAD. The study endpoint was reached in 12 (9.1%) patients with and 87 (4.9%) patients without DM (p = 0.024). Quantification of coronary stenosis by CADRADS or CAD severity (normal/non-obstructive/obstructive) was incremental for endpoint prediction with a multivariate (+Morise) χ2 of 3.90 and 3.85, respectively. The lowest annual event rate of 0.19% was noted in non-diabetic patients with no CAD, translating to a warranty period of 5.26 years. The highest annual event rate of 1.73% was found in diabetic patients with obstructive CAD, corresponding to a warranty period of 0.58 years. Compared to patients with no DM and no CAD, the risk of death or myocardial infarction in diabetic patients increased with rising levels of coronary obstruction at multivariate hazard ratios (HR) of 3.28 [95% CI 2.32, 4.64 (p < 0.001)], 3.02 [95% CI 2.19, 4.17 (p < 0.001)] and 9.40 [95% CI 4.90, 18.03 (p < 0.001)] for normal coronary arteries, non-obstructive CAD and obstructive CAD. This study validates the long-term prognostic utility of CCTA-assessed CAD for predicting death or myocardial infarction in a population of patients with DM. The rates of death or myocardial infarction rise with CAD severity in diabetic and non-diabetic patients, identifying the highest risk group of patients with DM and obstructive CAD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Throughout the western and developing world the prevalence of diabetes mellitus (DM) continues to rise and become a major public health issue. Affecting over 8% of the world population, DM has long been considered a coronary artery disease (CAD) equivalent, with cardiovascular disease being the most frequent cause of death in affected patients [1, 2]. This perception has however begun to change and newly proposed guidelines acknowledge a heterogeneous population risk with different treatment recommendations for diabetic patients considered to be at low risk [3, 4]. As metabolic processes differ largely between diabetic and non-diabetic patients, established clinical risk scores that have been derived from predominantly non-diabetic cohorts cannot reliably identify diabetic patients at elevated cardiovascular risk. Early detection of relevant CAD is however paramount in these high-risk patients as it widens the window for optimized treatment and contributes to prognosis improvement.
The incremental value of coronary computed tomography angiography (CCTA) over calcium scoring has been shown as not all plaques are calcified and a relevant part of patients with a calcium score of 0 still have obstructive stenoses [5]. Yet, outcome data of diabetic patients after CCTA are limited by follow-up periods that might not sufficiently grasp the slowly evolving nature of CAD. We therefore decided to investigate the long-term prognostic power of CCTA in oligosymptomatic diabetic patients and identify its incremental predictive value beyond clinical risk scoring.
Methods
Study population
Eligible for analysis were all consecutive patients with suspected but not previously diagnosed CAD undergoing CCTA at our institution from 01/10/2004 to 31/10/2008. Exclusion criteria were patients with angina pectoris, patients in an acute life-threatening situation and patients with no stable sinus rhythm during the exam. Written informed consent was obtained before the investigation. Information about age, weight and height of the patient, symptoms, cardiac history and current medication was collected. The following cardiac risk factors were recorded: (1) presence and degree of hypertension (for binary analysis hypertension was defined as a systolic blood pressure of > 140mmHg or administration of antihypertensive therapy); (2) diabetes mellitus (defined as fasting blood glucose level > 7mmol/l or abnormal oral glucose tolerance test as defined by the World Health Organization, use of oral anti-diabetic therapy or subcutaneous insulin therapy); (3) smoking (defined as current smoker or previous smoker within the last year), and (4) positive family history (defined as presence of CAD in first-degree relatives younger than 55 years in males or 65 years in females). In addition, laboratory results for total cholesterol, LDL- and HDL-fraction, and triglycerides were collected. From these data, the Morise score was calculated and reduced by the 2 points attributed for DM in diabetic patients to prevent data overcorrection. The study design was approved by the local ethics committee.
Computed tomography procedure
The detailed scan protocol has been described elsewhere [6]. Different CT hardware has been used during the study period: a 64-slice single-source CT scanner was used from October 2004 to September 2006 and a 64-slice dual-source CT scanner from October 2006 to October 2008 (both Siemens Healthineers, Erlangen, Germany).
Coronary artery segmentation was done according to the simplified American Heart Association classification, using the first 15 of the original 18 segments. Vessel segments > 1.5 mm diameter were evaluated by two physicians with an experience of having read more than 400 cardiac CTs at the time the scan was performed. Disagreements were settled by consensus.
Each stenosis was rated visually according to the following groups: no stenosis (0%), minimal stenosis (1–24%) mild (25–49%), moderate (50–69%), and severe (≥ 70%) stenosis. Segments with artifacts were assigned to the most appropriate group. Calcified plaques were defined as having a signal intensity above the contrasted vessel lumen and further specified as “spotty” if the calcifications showed a maximum diameter of < 3 mm in any direction or “gross” if the calcifications had an extent ≥ 3 mm in any direction.
From the primary analysis the following CCTA scores were calculated: CAD severity as proposed by Ostrom et al. with the categories “normal”, “non-obstructive” and “obstructive” (which was itself divided into “one-vessel obstructive”, “two-vessel obstructive” and “three-vessel obstructive”) [7]. Segment involvement score (SIS): number of segments with any stenosis ≥ 25% or any calcified or non-calcified plaque irrespective of the degree of stenosis. Addition of affected segments results in a score ranging from 0 to 15. CADRADS (Coronary Artery Disease-Reporting and Data System™) as proposed by Cury et al.[8].
Follow-up
Follow-up information was obtained by clinical visits, if available, by detailed questionnaires sent by mail or, if the questionnaires were not returned, by phone contact. All reported events were verified by hospital records or phone contact with the attending physician if possible and adjudicated by two physicians in consensus. A composite of all-cause mortality and myocardial infarction was chosen as endpoint.
Definition of warranty period
In analogy to established practice, low patient risk is defined as a cumulative event rate for a defined endpoint below 1% [9]. In our study, warranty period is defined as the duration in years that an individual can be considered to be at low-risk for death or myocardial infarction, maintaining a cumulative probability for the defined endpoint of below 1%.
Statistical analysis
Categorical variables were expressed as frequencies and percentages, continuous variables are described as means ± standard deviation or as median (interquartile range, IQR) for time intervals. All statistical evaluations are based on the event-free survival for the study endpoint using Kaplan–Meier method. Hazard ratios and multivariable analyses were calculated and performed using the Cox proportional hazards method. The likelihood-ratio test was used to test for significant differences in survival curves. Concordance c-indices were evaluated from time-to-event data as proposed by Harrell et al. [10]. In the multivariate model the incremental c-index for adding the CCTA variable to clinical risk scores was calculated. All statistical tests were performed two-sided and a significance level of 5% was used. The statistical package R version 2.10.1 including the package rms was used for statistical analysis [11, 12]
Results
Study population and patient characteristics
During the study period, 2176 patients with suspected but not previously diagnosed CAD underwent CCTA. In total 175 patients were excluded; 98 patients with stable angina, 5 patients with acute aortic dissection undergoing CCTA as a pre-operative assessment, 1 patient in the setting of acute coronary syndrome and 71 patients who did not have a stable sinus rhythm during the scan. Out of the remaining 2001 patients, 1913 patients could be contacted for follow-up and included into the study (follow-up rate of 96%). There were a total of 132 patients with diabetes mellitus. The control group consisted of 1781 patients without diabetes mellitus. Median follow-up was 9.7 [IQR 6.9, 11.2] years for diabetic patients and 9.9 [IQR 6.9, 11.1] years for non-diabetic patients. Diabetic patients were significantly older, more often overweight and had a higher prevalence of arterial hypertension but showed lower levels of total cholesterol and its LDL-fraction compared to controls. The pre-test score (Morise) was higher for diabetic patients (12.0 ± 2.1 vs. 10.6 ± 2.7, p < 0.001) after subtraction of the 2 diabetes-attributed points. There were no significant differences between sex, smoking status or family history for both groups. Detailed patient baseline characteristics are provided in Table 1.
Endpoints and clinical correlation
Diabetic patients experienced 3 cardiac deaths, 7 non-cardiac deaths and 2 non-fatal myocardial infarctions leading to an occurrence of the endpoint in 12 (9.1%) patients. In comparison, non-diabetic patients experienced 35 cardiac deaths, 42 non-cardiac deaths and 10 non-fatal myocardial infarctions leading to an endpoint occurrence in 87 (4.9%) patients. Overall, diabetic patients were more likely to suffer from the endpoint than non-diabetics (9.1% vs. 4.9%, p = 0.024).
Computed tomography results
CCTA demonstrated more pronounced CAD in diabetics as only 18 patients (13.6%) had normal coronary arteries vs. 533 (29.9%) of non-diabetic patients (p < 0.001). A similar frequency of non-obstructive plaques (CADRADS 1–2) of less than 50% stenosis level was noted in diabetic (42.4%) and non-diabetic (45.5%) patients (p = 0.93); obstructive lesions (CADRADS ≥ 3) of more than 50% stenosis level were significantly more common in diabetics (43.9% vs. 24.5%, p < 0.001). Notably more high-grade stenoses between 70–99% (CADRADS 4a) were present in diabetics (8.3% vs. 3.4%, p = 0.014). Total coronary vessel occlusion as given by CADRADS 5, as well as CADRADS 4b occurred rarely and similarly often in both groups.
The segment involvement score (SIS) was higher for diabetics (SIS 4.96 ± 3.57 vs. 2.89 ± 3.08, p < 0.001) than control. Diabetic patients had notably more plaques with a spotty (2.93 ± 2.49 vs. 1.68 ± 2.15 p < 0.001) or gross (0.97 ± 1.73 vs. 0.39 ± 1.09, p < 0.001) calcification pattern. Detailed CCTA results are given in Table 2.
Predictive power of CCTA parameters
In patients with DM, CADRADS showed the best primary endpoint correlation on univariate analysis (HR 1.74 [95% CI 1.01, 3.02], p = 0.047) and significantly improved outcome prediction over clinical risk on multivariate analysis (HR 1.72 [95% CI 0.98, 3.01], p = 0.048). CAD severity had good predictive power on univariate analysis (HR 1.60 [95% CI 1.02, 2.52], p = 0.040) and just significant incremental power on multivariate analysis (HR 1.59 [95% CI 1.01, 2.51], p = 0.050). Generalized plaque extent, as given by the SIS showed a trend for univariate (HR 2.13 [95% CI 0.83, 5.47], p = 0.12) and multivariate (HR 2.01 [95% CI 0.74, 5.41], p = 0.17) outcome prediction. In patients with DM the amount of spotty or grossly calcified plaques were non-predictive for outcome at respective univariate hazard ratios of 1.51 [95% CI 0.78, 2.93 (p = 0.23)] and 1.17 [95% CI 0.93, 1.49 (p = 0.18)]. A comparable relation of endpoint prediction between spotty calcifications and gross calcifications could be noted in patients with DM (univariate χ2 of 1.47 and 1.77, respectively) and without DM (univariate χ2 of 19.0 and 20.9, respectively).
Univariate and multivariate analyses for diabetic/non-diabetic patients are given in Tables 3 and 4. Receiver operator characteristic (ROC) analysis for diabetic patients with a marked increase of the area under the curve (AUC) after addition of the best performing CCTA parameters to pre-test risk (Morise) is shown in Fig. 1.
Receiver operator characteristics (ROC) curves for patients with DM in a univariate model based on Morise and a multivariate model after further adjustment to CAD severity, CADRADS and SIS. DM diabetes mellitus, CADRADS Coronary Artery Disease-Reporting and Data System™, CAD coronary artery disease, SIS segment involvement score
Relative risk of diabetic patients
Taking non-diabetic patients with normal coronary arteries as a reference, a gradual risk increase for the endpoint was noted for the non-diabetic group in non-obstructive (HR 2.70 [95% CI 2.02, 3.60], p = 0.008) and obstructive (HR 6.29 [95% CI 3.68, 10.75], p < 0.001) CAD on univariate analysis as well as after correction for clinical risk in non-obstructive (HR 2.43 [95% CI 1.15, 5.13], p = 0.019) and obstructive (HR 5.39 [95% CI 2.57, 11.29], p < 0.001) CAD. Compared to non-diabetic patients with no CAD, diabetic patients had an elevated risk that failed to reach statistical significance if normal coronary arteries (HR 3.28 [95% CI 2.32; 4.64], p = 0.26) or non-obstructive CAD (HR 3.02 [95% CI 2.19; 4.17], p = 0.10) but beyond statistical significance if obstructive CAD (HR 9.40 [95% CI 4.90; 18.03], p < 0.001) was present. After correction for clinical risk the hazard of diabetics stayed significantly elevated for patients with obstructive CAD (HR 7.78 [95% CI 2.93, 20.67], p < 0.001). On multivariate analysis, the presence of normal coronary arteries or non-obstructive CAD in diabetic patients still failed to significantly improve endpoint prediction beyond clinical risk at respective hazard ratios of 2.95 [95% CI 0.37, 23.35 (p = 0.31)] and 2.50 [95% CI 0.67, 9.41 (p = 0.17)].
Hazard analysis of diabetic patients vs. non-diabetic controls as a function of CAD extent is given in Table 5. Kaplan–Meier event-free survival curves for the endpoint as a function of coronary obstruction levels are given in Fig. 2.
While diabetic patients had no heightened risk compared to non-diabetic patients in the absence of spotty calcified plaques (HR 1.46 [95% CI 0.20, 10.95], p = 0.71), there was a marked risk increase of death or myocardial infarction in the presence of any spotty calcified plaque, both in diabetics (HR 4.36 [95% CI 2.07, 9.17], p < 0.001) and non-diabetics (HR 2.88 [95% CI 1.73, 4.78], p < 0.001) alike. On multivariate analysis the elevated risk persisted in both, non-diabetic patients (HR 2.48 [95% CI 1.47, 4.20], p = 0.001) and diabetic patients (HR 3.49 [95% CI 1.62, 7.53], p = 0.0014) (Table 6).
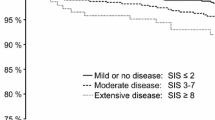
Warranty periods
Differing annual event rates as a function of CAD severity and diabetes status allowed for the calculation of warranty periods, as given in Fig. 3. Shorter warranty periods were noted in diabetics at 1.64, 1.75 and 0.58 years if normal coronary arteries, non-obstructive CAD or obstructive CAD was present compared to 5.26, 2.04 and 0.85 years for non-diabetic patients.
Warranty period (duration in years to reach a cumulative risk ≥ 1% for death or myocardial infarction) in diabetic patients: 1.64 years for normal coronary arteries, 1.75 years for non-obstructive CAD, 0.58 years for obstructive CAD; in non-diabetic patients 5.26 years for normal coronary arteries, 2.04 years for non-obstructive CAD and 0.85 years for obstructive CAD. CAD coronary artery disease, AER annual event rate
Discussion
For oligosymptomatic patients with DM and no previous history of CAD we could demonstrate that: (1) incremental to clinical risk, CCTA maintains a long-term value to predict death and myocardial infarction, (2) CCTA allows for risk stratification according to CAD severity, (3) even if DM is associated with more protruded CAD, plaque morphology and the associated risks are similar to non-diabetic patients.
To date, reports on cardiovascular prognosis based on non-invasive myocardial imaging are often limited by follow-up periods too short to sufficiently grasp the slowly evolving nature of CAD. Validation of the long-term predictive power of CCTA for death and myocardial infarction is nonetheless paramount in the early management of chronic diseases such as DM. Consistent with previous studies that used shorter observation periods and in some cases softer endpoints (i.e., inclusion of revascularization), our results demonstrate that compared to a non-diabetic population with a similar cardiovascular risk profile, diabetics experience more profound CAD and heightened hazards for death and myocardial infarction with rising degrees of coronary vessel obstruction [5, 13,14,15,16]. Even if the endpoint occured overall more often in diabetic patients, the underlying study demonstrates that identification of high-risk diabetic patients with obstructive CAD is feasible, potentially opening the door for a more targeted and cost-effective use of preventive strategies. Thus, for the longest follow-up reported so far, this study validates the role of CCTA as a non-invasive risk-stratification tool in a diabetic population. Although not reaching statistical significance, it is worthwhile to mention that a non-negligible share of 14% of diabetic patients with no evident CAD still had a higher risk for death or myocardial infarction, contrasting previously published data of shorter follow-up periods that acknowledged excellent prognoses for both, patients with and without DM in the absence of any CAD [13, 14, 17,18,19,20]. On the one hand, the vast evidence of factors promoting endothelial dysfunction and leading to a pro-atherosclerotic environment in diabetic patients allows for the assumption that during a long observation period of 10 years, vascular damage appears even in patients with normal coronary arteries on baseline CCTA [21]. On the other hand, our findings are in agreement to accumulating data that the systemic nature of DM not only deteriorates cardiovascular prognosis, but also leads to an elevated non-cardiac morbidity and mortality [22,23,24,25]. Our findings of potentially impaired prognoses in diabetic patients with no obvious CAD might help elucidate why the FACTOR-64 trial, a forerunner in CCTA-directed therapy, could not significantly improve outcome of diabetic patients compared to guideline-conform therapy, even if a newly introduced intensified therapy regime shortly before study initiation might have reduced the scope of treatment intensification [26].
Previous studies have hinted at the prognostic role of differing plaque compositions in diabetic and non-diabetic patients [27,28,29]. Our findings confirm a higher absolute number of plaques with a spotty or gross calcification pattern in diabetic patients, in line with results gathered by intravascular ultrasound [30]. Considering that CAD is more protruded in patients with DM, as shown in previous studies from our working group, the relative distribution of spotty or grossly calcified plaques was nonetheless similar to non-diabetics [16, 31]. Furthermore, the magnitude with which spotty and gross calcifications correlated with outcome was comparable in patients with and without DM. Hence, our data suggest a higher plaque quantity with comparable plaque qualities in diabetic compared to non-diabetic patients.
Limitations
Worth mentioning is the fact that this is a single-center study and no information on diabetes subtype (type 1 vs. type 2), duration of disease, treatment regimes, compliance to treatment or blood glucose levels was available. These data were not included into our registry and retrospective determination of blood glucose levels would be of limited value after such a long follow-up. However, the long observation period partially offsets lacking information on disease duration as even a newly diagnosed DM can be expected to accelerate cardiovascular disease after 10 years. The actual population of diabetic patients in this study is comparatively small, potentially reducing the statistical power of our analysis. Even as the overall low event rates of diabetic patients in our cohort might soften the statistical power of our analysis, we are convinced that restrictive endpoint selection in this cohort is of greatest clinical utility. For multivariate analysis, correction has been done for clinical risk only to prevent overfitting of the model.
Conclusions
Beyond clinical risk scoring, CCTA has incremental value for predicting long-term mortality and morbidity in patients with DM. Of clinical relevance is the finding, that especially when obstructive CAD is present, the risk of death and myocardial infarction of diabetic patients significantly exceeds that of their non-diabetic peers. While diabetic patients have a higher burden of CAD, their plaque composition is comparable to non-diabetics.
Abbreviations
- DM:
-
Diabetes mellitus
- CAD:
-
Coronary artery disease
- CCTA:
-
Coronary computed tomography angiography
- SIS:
-
Segment involvement score
- CADRADS:
-
Coronary Artery Disease-Reporting and Data System™
- ROC:
-
Receiver operator characteristics
- SC:
-
Spotty calcification
- GC:
-
Gross calcification
References
Emerging Risk Factors C, Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M, Stehouwer CD, Lewington S, Pennells L, Thompson A, Sattar N, White IR, Ray KK, Danesh J (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375(9733):2215–2222
da Rocha Fernandes J, Ogurtsova K, Linnenkamp U, Guariguata L, Seuring T, Zhang P, Cavan D, Makaroff LE (2016) IDF Diabetes Atlas estimates of 2014 global health expenditures on diabetes. Diabetes Res Clin Pract 117:48–54
Authors Task Force M, Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Lochen ML, Lollgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, Bart van der Worp H, van Dis I, Verschuren WMM, (2016) 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Atherosclerosis 252:207–274
American Diabetes A (2013) Standards of medical care in diabetes–2013. Diabetes Care 36(Suppl 1):S11–66
Min JK, Labounty TM, Gomez MJ, Achenbach S, Al-Mallah M, Budoff MJ, Cademartiri F, Callister TQ, Chang HJ, Cheng V, Chinnaiyan KM, Chow B, Cury R, Delago A, Dunning A, Feuchtner G, Hadamitzky M, Hausleiter J, Kaufmann P, Kim YJ, Leipsic J, Lin FY, Maffei E, Raff G, Shaw LJ, Villines TC, Berman DS (2014) Incremental prognostic value of coronary computed tomographic angiography over coronary artery calcium score for risk prediction of major adverse cardiac events in asymptomatic diabetic individuals. Atherosclerosis 232(2):298–304
Hadamitzky M, Taubert S, Deseive S, Byrne RA, Martinoff S, Schomig A, Hausleiter J (2013) Prognostic value of coronary computed tomography angiography during 5 years of follow-up in patients with suspected coronary artery disease. Eur Heart J 34(42):3277–3285
Ostrom MP, Gopal A, Ahmadi N, Nasir K, Yang E, Kakadiaris I, Flores F, Mao SS, Budoff MJ (2008) Mortality incidence and the severity of coronary atherosclerosis assessed by computed tomography angiography. J Am Coll Cardiol 52(16):1335–1343
Cury RC, Abbara S, Achenbach S, Agatston A, Berman DS, Budoff MJ, Dill KE, Jacobs JE, Maroules CD, Rubin GD, Rybicki FJ, Schoepf UJ, Shaw LJ, Stillman AE, White CS, Woodard PK, Leipsic JA (2016) CAD-RADS(TM) Coronary artery disease—reporting and data system. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American College of Cardiology. J Cardiovasc Comput Tomogr 10(4):269–281.
Gibbons RJ, Chatterjee K, Daley J, Douglas JS, Fihn SD, Gardin JM, Grunwald MA, Levy D, Lytle BW, O'Rourke RA, Schafer WP, Williams SV (1999) ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: executive summary and recommendations. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients with Chronic Stable Angina). Circulation 99(21):2829–2848.
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15(4):361–387
Team RDC. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org2013. Accessed 15 July 2018
Harrell FE Jr (2001) Regression Modeling Strategies. Springer, Berlin, pp 53–85
Van Werkhoven JM, Cademartiri F, Seitun S, Maffei E, Palumbo A, Martini C, Tarantini G, Kroft LJ, de Roos A, Weustink AC, Jukema JW, Ardissino D, Mollet NR, Schuijf JD, Bax JJ (2010) Diabetes: prognostic value of CT coronary angiography–comparison with a nondiabetic population. Radiology 256(1):83–92
Blanke P, Naoum C, Ahmadi A, Cheruvu C, Soon J, Arepalli C, Gransar H, Achenbach S, Berman DS, Budoff MJ, Callister TQ, Al-Mallah MH, Cademartiri F, Chinnaiyan K, Rubinshtein R, Marquez H, DeLago A, Villines TC, Hadamitzky M, Hausleiter J, Shaw LJ, Kaufmann PA, Cury RC, Feuchtner G, Kim YJ, Maffei E, Raff G, Pontone G, Andreini D, Chang HJ, Chow BW, Min J, Leipsic J (2016) Long-term prognostic utility of coronary CT angiography in stable patients with diabetes mellitus. JACC Cardiovasc Imaging 9(11):1280–1288.
Rana JS, Dunning A, Achenbach S, Al-Mallah M, Budoff MJ, Cademartiri F, Callister TQ, Chang HJ, Cheng VY, Chinnaiyan K, Chow BJ, Cury R, Delago A, Feuchtner G, Hadamitzky M, Hausleiter J, Kaufmann P, Karlsberg RP, Kim YJ, Leipsic J, Labounty TM, Lin FY, Maffei E, Raff G, Villines TC, Shaw LJ, Berman DS, Min JK (2012) Differences in prevalence, extent, severity, and prognosis of coronary artery disease among patients with and without diabetes undergoing coronary computed tomography angiography: results from 10,110 individuals from the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes): an InteRnational Multicenter Registry. Diabetes Care 35(8):1787–1794
Nadjiri J, Hausleiter J, Deseive S, Will A, Hendrich E, Martinoff S, Hadamitzky M (2016) Prognostic value of coronary CT angiography in diabetic patients: a 5-year follow up study. Int J Cardiovasc Imaging 32(3):483–491
Kang SH, Park GM, Lee SW, Yun SC, Kim YH, Cho YR, Park HW, Suh J, Yang DH, Kang JW, Lim TH, Jung CH, Koh EH, Lee WJ, Kim MS, Lee KU, Park JY (2016) Long-term prognostic value of coronary CT angiography in asymptomatic type 2 diabetes mellitus. JACC Cardiovasc Imaging 9(11):1292–1300
Andreini D, Pontone G, Mushtaq S, Bertella E, Conte E, Baggiano A, Veglia F, Agostoni P, Annoni A, Formenti A, Montorsi P, Ballerini G, Bartorelli AL, Fiorentini C, Pepi M (2013) Prognostic value of multidetector computed tomography coronary angiography in diabetes: excellent long-term prognosis in patients with normal coronary arteries. Diabetes Care 36(7):1834–1841
Raggi P, Shaw LJ, Berman DS, Callister TQ (2004) Prognostic value of coronary artery calcium screening in subjects with and without diabetes. J Am Coll Cardiol 43(9):1663–1669
Olesen KKW, Madsen M, Egholm G, Thim T, Jensen LO, Raungaard B, Botker HE, Sorensen HT, Maeng M (2017) Patients with diabetes without significant angiographic coronary artery disease have the same risk of myocardial infarction as patients without diabetes in a real-world population receiving appropriate prophylactic treatment. Diabetes Care 40(8):1103–1110
Hadi HA, Suwaidi JA (2007) Endothelial dysfunction in diabetes mellitus. Vasc Health Risk Manag 3(6):853–876
Tancredi M, Rosengren A, Svensson AM, Kosiborod M, Pivodic A, Gudbjornsdottir S, Wedel H, Clements M, Dahlqvist S, Lind M (2015) Excess mortality among persons with type 2 diabetes. N Engl J Med 373(18):1720–1732
Zhou XH, Qiao Q, Zethelius B, Pyorala K, Soderberg S, Pajak A, Stehouwer CD, Heine RJ, Jousilahti P, Ruotolo G, Nilsson PM, Calori G, Tuomilehto J, Group DS (2010) Diabetes, prediabetes and cancer mortality. Diabetologia 53(9):1867–1876
Allemann S, Saner C, Zwahlen M, Christ ER, Diem P, Stettler C (2009) Long-term cardiovascular and non-cardiovascular mortality in women and men with type 1 and type 2 diabetes mellitus: a 30-year follow-up in Switzerland. Swiss Med Weekly 139(39–40):576–583
Balkau B, Pyorala M, Shipley M, Forhan A, Jarrett J, Eschwege E, Pyorala K (1997) Non-cardiovascular disease mortality and diabetes mellitus. Lancet 350(9092):1680
Muhlestein JB, Lappe DL, Lima JA, Rosen BD, May HT, Knight S, Bluemke DA, Towner SR, Le V, Bair TL, Vavere AL, Anderson JL (2014) Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA 312(21):2234–2243
Kwon YS, Jang JS, Lee CW, Kim DK, Kim U, Seol SH, Kim DI, Jo YW, Jin HY, Seo JS, Yang TH, Kim DK, Kim DS (2010) Comparison of plaque composition in diabetic and non-diabetic patients with coronary artery disease using multislice CT angiography. Korean Circ J 40(11):581–586
Canpolat U, Aytemir K, Yorgun H, Hazirolan T, Kaya EB, Ates AH, Sunman H, Dural M, Yalcin MU, Tokgozoglu L, Kabakci G, Oto A (2012) Association of type 2 diabetes mellitus with coronary atherosclerotic plaque burden and morphology measured by multidetector computed tomography coronary angiography. Acta Cardiol 67(1):71–77
Pundziute G, Schuijf JD, Jukema JW, van Werkhoven JM, Nucifora G, Decramer I, Sarno G, Vanhoenacker PK, Reiber JH, Wijns W, Bax JJ (2009) Type 2 diabetes is associated with more advanced coronary atherosclerosis on multislice computed tomography and virtual histology intravascular ultrasound. J Nucl Cardiol 16(3):376–383
Kataoka Y, Wolski K, Uno K, Puri R, Tuzcu EM, Nissen SE, Nicholls SJ (2012) Spotty calcification as a marker of accelerated progression of coronary atherosclerosis: insights from serial intravascular ultrasound. J Am Coll Cardiol 59(18):1592–1597
Hadamitzky M, Hein F, Meyer T, Bischoff B, Martinoff S, Schomig A, Hausleiter J (2010) Prognostic value of coronary computed tomographic angiography in diabetic patients without known coronary artery disease. Diabetes Care 33(6):1358–1363
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Rights and permissions
About this article
Cite this article
Finck, T., Will, A., Hendrich, E. et al. Coronary computed tomography angiography as a tool for long-term cardiovascular risk stratification in diabetic patients. Heart Vessels 34, 1086–1095 (2019). https://doi.org/10.1007/s00380-018-01339-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-01339-0