Abstract
Prevalence of coronary artery disease (CAD) is high in diabetic patients while diagnosis of early stage of CAD remains demanding. This study evaluates prognostic value of coronary computed tomography angiography (CCTA) for long-term outcome to predict cardiac events in oligosymptomatic diabetic patients. A cohort of 108 consecutive diabetic patients without angina pectoris or known CAD, undergoing CCTA was included. 1379 consecutive patients without diabetes were defined as a control group. Coronary artery calcium score (CACS), segment involvement score (SIS) and the segment stenosis score (SSS) were documented. The end point was a composite of cardiac events defined as all-cause death, nonfatal myocardial infarction, or unstable angina requiring hospitalization. Follow up period was 66.0 ± 14.2 month. 98 % of initially enrolled patient were followed. During follow-up period 10 cardiac events within the diabetic cohort and 48 within the non-diabetic cohort were observed. Annual event rate in diabetic and non-diabetic patients was 1.74 and 0.64 % respectively. In diabetic patients a multivariate analysis showed significant prognostic value over Framingham Score for SIS with a hazard ratio (HR) of 2.98 (95 % CI 1.02, 8.72; p = 0.047) and SSS (HR 4.47, 95 % CI 1.21, 16.49; p = 0.025), while CACS did not add prognostic value in this cohort. Annual event rate was 0 % in diabetic patients with SIS = 0 and 3.9 % in diabetic patients with SIS ≥ 8. CCTA allows for improved risk prediction for subsequent cardiac events in oligosymptomatic diabetic patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetes is known to be a major cardiovascular risk factor associated with significantly increased morbidity and mortality and a particularly increased risk of major cardiac events (MACE) [1]. Especially myocardial infarction as a manifestation of highly incident coronary artery disease (CAD) can lead to decreased life expectation and life quality. Major cause for myocardial infarction is plaque rupture [2]. Prevalence of obstructive and non-obstructive plaques is increased in diabetic patients [3, 4]. Within last years, wide choices of treatment options for CAD, either invasive or non-invasive, are available. Furthermore treatment and management of CAD remains focus of many research projects worldwide [5, 6] and substantial reduction of mortalities in manifestations of CAD has been reported [7]. Although typical angina is a key symptom for CAD, its sensitivity in diabetic patients is limited. This might possibly reduce the benefit of modern treatment developments in diabetic patients [8, 9]. Hence early detection of CAD in diabetic patients is important to optimize disease management. Today, coronary computed tomography angiography (CCTA) has emerged as a highly accurate non-invasive method to evaluate CAD [10]. CCTA allows for a non-invasive detection of coronary stenosis as well as presence of calcified and non-calcified plaques. CCTA not only substitutes invasive coronary angiography under certain conditions [11] but it furthermore emerges as a useful prognostic tool for prediction of subsequent cardiac events [12, 13]. As prevalence of CAD in diabetic patients detected by CCTA has been demonstrated before but with shorter follow up [3] our study seeks to evaluate prognostic value of CCTA in oligosymptomatic diabetic patients to predict adverse cardiac events in a 5 years of follow up approach.
Methods
Study population
The study population consists of all consecutive patients undergoing CCTA in our institution between first of December 2003 and first of December 2006 for evaluation of suspected CAD. All patients were screened for enrollment in the study as described before [14]. Exclusion criteria were (1) typical angina pectoris, (2) a history of myocardial infarction including electrocardiographic signs of a silent myocardial infarction, (3) a history of coronary revascularization, either by percutaneous coronary intervention or bypass or otherwise known CAD, (4) absence of stable sinus rhythm during the investigation, and (5) a life-threatening condition. Patients were categorized according to the presence of diabetes, defined as current treatment with insulin or oral hypoglycemic medication or dietetic control of blood glucose levels in patients having elevated fasting blood glucose levels or an abnormal glucose tolerance test based on the World Health Organization criteria [15]. All patients gave written informed consent before examination. A structured questionnaire was answered by patients before examination to gather information about age, patients’ height and weight, history of cardiac disease, and present complaints. Furthermore the following cardiac risk factors were recorded: (1) presence and degree of hypertension, (2) diabetes (see definition above), (3) smoking (defined as current smoker or previous smoker within the last year), and (4) a positive family history (defined as the presence of CAD in first-degree relatives aged 55 years for male or 65 years for female). Framingham risk score was calculated with the established categorical model using LDL cholesterol according to Wilson et al. [16] based on collected data. The local ethics committee approved the study design.
Computed tomography procedure
The scan procedure has been described in detail before [17]. Different CT system configurations were used during the study period: A 16-slice CT system was used from December 2003 to September 2004, a 64-slice single source CT system from October 2004 to September 2006, and a 64-slice dual source CT system from October 2006 to December 2006 (all Siemens Healthcare, Erlangen, Germany). In case of a heart rate higher than 60 bpm, up to four doses of 5 mg of metoprolol were administered intravenously immediately before scanning. If systolic blood pressure was higher than 100 mmHg 0.8 mg nitroglycerin was administered sublingually just before scanning to achieve coronary vasodilatation.
Coronary artery calcium (CACS) was acquired by a non-contrast-enhanced sequential scan and evaluated with a commercially available software package (Siemens CalciumScore, Siemens, Erlangen, Germany) using the Agatston Score with a threshold of 130 HU. Contrast timing was tested by an initial bolus-timing scan using 10–20 ml of contrast (Iomeprol, Imeron 350, Bracco Altana Pharma GmbH, Konstanz, Germany, iodine content 350 mg/ml) followed by a 50 ml saline chaser. The contrast-enhanced scan was obtained using 80–140 ml of contrast individually adapted to the selected table feed and scan range at a rate of 4–6 ml/s followed by 50 ml of saline chaser bolus. Data sets of axial slices, multiplanar reformations, and three perpendicular sets of thin-slab maximum intensity projections orientated along the heart axis (5 mm thickness, 1 mm increment) were reconstructed and investigated for the presence of plaque composition and luminal stenosis.
The coronary artery tree was segmented according to a simplified American Heart Association classification using the first 15 segments of the original 18 [18]. Each vessel segment with a diameter ≥1.5 mm was evaluated visually by two experienced readers. Disagreements were settled by consensus. The degree of stenosis was assessed visually categorizing either no relevant stenosis (25 %), mild (25–49 %), moderate (50–74 %), and severe (≥75 %) stenosis. Segments with artefacts were assigned to the group that seemed most appropriate.
From the primary analysis the following CCTA scores were calculated:
CAD severity as proposed by Chow et al. with the categories ‘normal’, ‘non-obstructive’, ‘one-vessel obstructive’, ‘two-vessel obstructive’ and ‘three-vessel obstructive’. Segment Involvement Score (SIS), as described by Min [12] was defined as number of segments with any stenosis ≥25 % or any calcified, mixed or non-calcified plaques, irrespective of the degree of stenosis. Furthermore segment stenosis score (SSS) was utilized as described before [12, 19].
Follow-up
Follow-up information was obtained by clinical visits, by detailed questionnaires sent by mail, or, if the questionnaire was not returned, by telephone contact. All reported events were verified by hospital records or direct contact with the attending physician as possible and adjudicated by two cardiologists in consensus (Figs. 1, 2).
Event free survival of non-diabetic oligosymptomatic patients. Survival is illustrated in a period of 1800 days for three groups of patients categorized by Segment involvement score (SIS). The continuous line indicates survival of patients with mild or no disease (SIS ≤ 2). The dashed line illustrates survival with moderate disease (SIS 3–7). The dotted line shows survival in patients with extensive disease (SIS ≥ 8)
Event free survival of diabetic oligosymptomatic patients. Survival is illustrated in a period of 1800 days for three groups of patients categorized by Segment involvement score. The continuous line indicates survival of patients with mild or no disease (SIS ≤ 2). The dashed line illustrates survival with moderate disease (SIS 3–7). The dotted line shows survival in patients with extensive disease (SIS ≥ 8)
The endpoint of this study was a composite of all cause death, myocardial infarction and unstable angina requiring hospitalization. Non-fatal myocardial infarction was defined based on the criterion of typical acute chest pain in rest lasting at least 20 min and at least one of the following criteria: ST-segment elevation in at least two limb leads of 0.1 millivolt (mV) or at least 0.2 mV in more than 2 precordial leads or positive cardiac enzymes. Unstable angina pectoris was defined according to the guidelines of the European Society of Cardiology [20] as typical acute chest pain with negative cardiac enzymes, if CAD could not be excluded as the cause of symptoms.
Statistical analysis
Categorical variables were expressed as frequencies and percentages, continuous variables were expressed as mean ± standard deviation or as median (inter-quartile range) for time intervals. All statistical evaluations are based on the event-free survival for the study endpoint using the Kaplan–Meier method; hazard ratios (for difference between 75 and 25th percentile) and multivariable analyses were calculated with the Cox proportional hazard model.
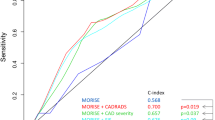
Concordance(C)-indices were calculated from time-to-event data as proposed by Harrell et al. [21].
For explorative testing multiple random subsamples within the non-diabetic group sized similar to the diabetic group were generated and tested for single variables.
Due to non-normal distribution, CACS was entered into the multivariable analysis using its logarithm [log (CASC + 1)]. Owing to the low number of events and considering that only asymptomatic patients or those with atypical chest pain were in focus, correction for clinical risk was done by using the Framingham Risk Score. Statistical significance was accepted for two-sided p value <0.05. The statistical package R version 3.0.3 was used for analysis [22].
Results
Study population and clinical characteristics
A total of 1519 patients met the inclusion criteria. Of these, 1487 patients could be contacted for follow-up, resulting in a follow-up rate of 97.9 %. Overall, there were 108 patients with diabetes. In 34 patients, blood glucose levels were controlled by diet, 56 patients took oral antidiabetic medication, and 18 patients were using insulin. The control group comprised the 1379 patients without known diabetes. The mean duration of follow up was 64.7 ± 15.3 months [median: 66.7 (IQR: 61.0–75.0)] in the diabetic group and 66.1 ± 14.1 months [median: 67.2[IQR: 61.5–74.8)] in the control group, p = 0.357. Diabetic patients were significantly older and more often overweight, and there were more patients with hypertension and hypercholesterolemia among diabetic patients compared with non-diabetic patients, resulting in a significantly higher Framingham risk score. Patients’ sex and the prevalence of dyspnea did not differ significantly between both groups. Overall the pretest risk was significantly higher in diabetic patients. For a detailed description of the patient characteristics, see Table 1. Diabetic patients had significant lower total cholesterol and LDL-levels. While triglycerides were significantly increased there was no relevant difference in HDL between diabetic and non-diabetic patients. Laboratory values for total cholesterol, LDL, HDL and triglycerides are illustrated in Table 2.
Computed tomography results
There are no significant differences in main indication for CCTA in diabetic and non-diabetic patients as shown in Table 3. Of 108 diabetic patients 15 (13.9 %) had completely normal coronary arteries and 38 (35.2 %) had plaques with vessel narrowing less than 50 %. 55 (50.9 %) patients had more than 50 % stenotic plaques. Presence of CAD (plaques and/or obstruction) was 86.1 % (93 patients) in the diabetics and 65.7 % (906 patients) in the non-diabetic group, p < 0.0001; the presence of obstructive CAD (stenosis >50 %) was also significantly higher in diabetic patients (p < 0.0001). Detailed CCTA results are provided in Table 4. Calcified (2.94 vs 1.54, p < 0.0001), mixed (0.85 vs 0.41, p = 0.0023) and non-calcified (1.33 vs 0.795, p = 0.0081) plaques all occurred significantly more often in diabetic patients. SIS, SSS were both significantly increased in diabetic group compared to control (SIS: 5.12 vs 2.78, p < 0.0001; SSS: 10.2 vs 5.24, p < 0.0001). In diabetic patients, the mean CACS of 419 was significantly higher than that in non-diabetic patients (CACS of 164, p = 0.0008). CACS was not available in 81 cases.
Adverse events
In the control group, 48 outcome events were observed (3.4 %); 35 patients died, 10 patients suffered from myocardial infarction and 4 patients were hospitalized because of unstable angina (one patient with unstable angina died later during follow-up). In the group of diabetic patients, 10 study endpoints were observed (9.3 %); 7 patients died, 2 patients suffered from myocardial infarction and 1 patient was hospitalized because of unstable angina. The annual event rate in diabetic group and control group were 1.7 and 0.64 %, respectively (p = 0.0072). Annual event rate was highest in patients with insulin therapy (3.2 %), patients with dietetically and oral antidiabetic medication had annual event rates of 1.7 and 1.3 %, respectively.
Predictive value of Framingham Score in study group
Mean Framingham Score for diabetic group and control group were 19.0 ± 12.0 and 9.5 ± 7.1, respectively (p < 0.0001). For patients without cardiac event mean Framingham Score was 9.96 ± 7.71. Patients with cardiac events had a mean Framingham Score of 16.3 ± 10.2, HR 1.68 (95 % CI 1.41, 2.01), p < 0.0001.
In the non-diabetic control group the Framingham Score showed good correlation with cardiac events, HR 1.81 (95 % CI 1.46, 2.25), p < 0.0001. Patients in the control group without and with cardiac events had a mean Framingham Score of 9.3 ± 6.8 and 15.1 ± 9.9, respectively.
Framingham Score did not significantly differ in diabetic patients with or without cardiac event HR 1.22 (95 % CI 0.709, 2.09), p = 0.48. Diabetic patients without cardiac event had a Framingham Score of 18.7 ± 12; diabetic patients with cardiac event had a mean Framingham Score of 22.2 ± 10. 2, p = 0.11.
Predictive value of CCTA in diabetic patients
In diabetic patients, SIS and SSS correlated best with clinical events in the univariate and multivariate analysis with a HR of 2.98 (95 % CI 1.02, 8.72; p = 0.047) and 4.47 (95 % CI 1.21, 16.49; p = 0.025), respectively. Annual event rate was 0 % in diabetic patients with SIS = 0. For SIS ≤ 2 and for SIS 3–7 the annual event rates were <1 and 1.2 %, respectively. Patients with SIS ≥8 had an annual event rate of 3.9 %. Regarding plaque characteristics, the extent of calcified plaques showed good correlation with the study endpoint HR 2.0 (95 % CI 1.05, 3.8; p = 0.034). In contrast to the non-diabetic group, CACS had no significant correlation with outcome in the much smaller diabetic group (p = 0.0949. In comparison explorative testing using randomly generated subsamples of similar size in the non-diabetic group yielded on average similar results (p = 0.18). Detailed results of the univariate and multivariate analysis are shown in Tables 5 and 6.
Discussion
Diabetes itself is considered to be a cardiovascular disease equivalent [11]. In this high risk population for CAD main findings of this study are (1) the predictive value of CCTA in oligosymptomatic diabetes sustains for at least 5 years. (2) Oligosymptomatic diabetics are at high risk for major cardiac events and CCTA, particularly SSS and SIS are useful in these patients for further risk stratification beyond clinical risk scoring. (3) Diabetics with low atherosclerotic burden in form of low SIS have excellent prognosis.
As described before, the non-invasive technique CCTA can rule out CAD with high accuracy [11] supported by our results showing low annual event rates in patients with no evidence of atherosclerosis in CCTA in non-diabetic patients as well as in diabetic patients.
Andreini and coworkers demonstrated good prognostic value of CCTA in symptomatic but not oligosymptomatic diabetic patients for obstructive CAD and plaque load. Additionally they report an excellent prognosis for diabetics with no evidence of atherosclerosis in a long term follow up period of 6 years without comparing to a control group [23]. At this time point prognostic CCTA studies in oligosymptomtic diabetic patients with a long term follow up are rare. A recent study by Min et al. [24] showed incremental prognostic value of CCTA over clinical risk factors and CACS in asymptomatic diabetic patients in a multicenter approach. Their results showed that CCTA is able to identify high risk patients in oligosymptomatic diabetics by number of vessels with obstructive CAD. On the other hand they also report in accordance to earlier studies [25] that also oligosymptomatic diabetics with non-obstructive CAD had increased risk for cardiac adverse events. Hence they hypothesize that evaluation of CAD in all diabetics may not uniformly be applicable [24]. They presume that extent of disease, with and without particular emphasis on obstruction, provides risk stratification. Nevertheless the prognostic models in this study all were based on degree of stenosis.
In accordance our results indicate that in oligosymptomatic diabetic patients extent of disease (SIS) and extent of disease with additional regard for stenosis (SSS) add prognostic value for long-term outcome over clinical risk scoring. Although comprising high-risk individuals, oligosymptomatic diabetic patients over all had, independently from CCTA, an excellent prognosis which was slightly better than predicted by Framingham Score (annual event rate of 0.6 vs. 0.9 %).
Recently it has been shown in a large randomized clinical trial that treatment based on a screening CCTA in asymptomatic diabetic patients did not reduce MACE compared to a control group [26]. This result may in part be caused by a lower than expected event rate in the control group due to intensified therapy in all patients. In addition the study outcome might be caused by limited identification of high-risk individuals, because patients were characterized by degree of stenosis and CACS. Seemingly these parameters carry limited prognostic value in the subpopulation of oligosymptomatic diabetics. Furthermore, Andreini and colleagues reported reduced diagnostic performance of MDCT to detect obstructive CAD in diabetics [27]. In concordance to these findings our results indicate limited prognostic value of presence of obstructive CAD in oligosymptomatic diabetics during 5 years of follow up. Plaque load in contrast was a better predictor. SIS and SSS seem to improve the effective selectivity of CCTA data to determine a small high-risk sub population within the risk population of diabetic patients. Diabetics with SIS ≤ 2 had had an excellent prognosis, while outcome for patients with SIS ≥ 8 was rather unfavorable and it has to be evaluated in further studies weather diabetic patients with excellent prognosis benefit from secondary prophylaxis.
Taking into account the observation that diabetics have similar plaque composition but overall a higher plaque load [14] it seems that plaque load is the pathophysiological substrate linking coronary injury caused by diabetes with outcome. Apparently the number of plaques that eventually may cause coronary occlusion is more important than the composition or the degree of stenosis of an individual plaque for outcome in oligosymptomatic diabetics. On the other hand the number of calcified plaques was a risk predictor for diabetic patients while it was not in the control group. This might suggest potential differences in the constitution of calcified plaques.
Despite that, detection of high risk patients by SIS and SSS may result in a better assessment in individual coronary risk in oligosymptomatic diabetics in whom Framingham Risk Score has limited power to identify the high-risk subpopulation. Better risk identification by SIS and SSS may result in a more individualized therapy regimen targeting intensified anti-diabetic treatment and cardiovascular prevention therapy to those high risk patients in whom the risk associated with the therapy is clearly overweighed by the potentially benefit. Yet further research in larger studies has to be done.
Limitations
This is an observational single-center study. The results may be affected by characteristics unique to the patients investigated. Furthermore, outcome might be confounded by treatment decisions based on the results of the investigation. Type of diabetes was initially not assessed thus risk analysis regarding type I or II was not done and might add additional information in future studies. In addition, complete information on medication prescription and compliance during the follow-up is not available. Furthermore the small number of events in the diabetic group limits the robustness of all of the outcome analyses, particularly the multivariable analysis. Besides, the number of diabetic patients is small in this unrestricted patient population.
Conclusion
Prevalence of CAD in diabetic patients is high resulting in increased annual event rates, when compared with non-diabetic patients. CCTA provides good prognostic value for oligosymptomatic patients in a long-term follow of 5 years. SIS and SSS add prognostic value beyond clinical risk scores in oligosymptomatic diabetic patients. Especially the potential of non-invasive CCTA to rule out CAD and to identify high-risk patients may help guiding a more individualized therapy and might lead to a possible better outcome in this subgroup, although larger outcome studies are needed.
References
Macisaac RJJG (2011) Intensive glucose control and cardiovascular outcomes in type 2 diabetes. Heart Lung Circ 20:647–654
Davies MJ, Thomas AC (1985) Plaque fissuring-the cause of acute myocardial infarction, sudden ischaemic death, and crescendo angina. Br Heart 53:363
Iwasaki K, Matsumoto T, Aono H, Furukawa H, Samukawa M (2008) Prevalence of subclinical atherosclerosis in asymptomatic diabetic patients by 64-slice computed tomography. Coron Artery Dis 19(3):195–201
Zeina AR, Odeh M, Rosenschein U, Zaid G, Barmeir E (2008) Coronary artery disease among asymptomatic diabetic and nondiabetic patients undergoing coronary computed tomography angiography. Coron Artery Dis 19(1):37–41
Caruba T, Katsahian S, Schramm C, Charles Nelson A, Durieux P, Begue D, Juilliere Y, Dubourg O, Danchin N, Sabatier B (2014) Treatment for stable coronary artery disease: a network meta-analysis of cost-effectiveness studies. PLoS ONE 9(6):e98371. doi:10.1371/journal.pone.0098371
Sluijter JP, Condorelli G, Davidson SM, Engel FB, Ferdinandy P, Hausenloy DJ, Lecour S, Madonna R, Ovize M, Ruiz-Meana M, Schulz R, Van Laake LW, Novel therapeutic strategies for cardioprotection (2014) Novel therapeutic strategies for cardioprotection. Pharmacol Ther. doi:10.1016/j.pharmthera.2014.05.005
Apex AMI Investigators, Armstrong PW, Granger CB, Adams PX, Hamm C, Holmes D Jr, O’Neill WW, Todaro TG, Vahanian A, VdW F (2007) Pexelizumab for acute ST-elevation myocardial infarction in patients undergoing primary percutaneous coronary intervention: a randomized controlled trial. JAMA 3(1):43–53
Kamalesh M, Feigenbaum H, Sawada S (2007) Assessing prognosis in patients with diabetes mellitus–the Achilles’ heel of cardiac stress imaging tests? Am J Cardiol 99(7):1016–1019. doi:10.1016/j.amjcard.2006.10.071
Arenja N, Mueller C, Ehl NF, Brinkert M, Roost K, Reichlin T, Sou SM, Hochgruber T, Osswald S, Zellweger MJ (2013) Prevalence, extent, and independent predictors of silent myocardial infarction. Am J Med 126(6):515–522. doi:10.1016/j.amjmed.2012.11.028
Gao D, Ning N, Guo Y, Ning W, Niu X, Yang J (2011) Computed tomography for detecting coronary artery plaques: a meta-analysis. Atherosclerosis 219(2):603–609. doi:10.1016/j.atherosclerosis.2011.08.022
Abdulla J, Abildstrom SZ, Gotzsche O, Christensen E, Kober L, Torp-Pedersen C (2007) 64-multislice detector computed tomography coronary angiography as potential alternative to conventional coronary angiography: a systematic review and meta-analysis. Eur Heart J 28(24):3042–3050. doi:10.1093/eurheartj/ehm466
Min JK, Shaw LJ, Devereux RB, Okin PM, Weinsaft JW, Russo DJ, Lippolis NJ, Berman DS, Callister TQ (2007) Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol 50(12):1161–1170. doi:10.1016/j.jacc.2007.03.067
Hadamitzky M, Taubert S, Deseive S, Byrne RA, Martinoff S, Schomig A, Hausleiter J (2013) Prognostic value of coronary computed tomography angiography during 5 years of follow-up in patients with suspected coronary artery disease. Eur Heart J 34(42):3277–3285. doi:10.1093/eurheartj/eht293
Hadamitzky M, Hein F, Meyer T, Bischoff B, Martinoff S, Schomig A, Hausleiter J (2010) Prognostic value of coronary computed tomographic angiography in diabetic patients without known coronary artery disease. Diabetes Care 33(6):1358–1363. doi:10.2337/dc09-2104
Diabetes mellitus. Report of a WHO Study Group (1985). World Health Organization technical report series 727:1–113
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB (1998) Prediction of coronary heart disease using risk factor categories. Circulation 97(18):1837–1847
Hausleiter J, Meyer T, Hadamitzky M, Zankl M, Gerein P, Dorrler K, Kastrati A, Martinoff S, Schomig A (2007) Non-invasive coronary computed tomographic angiography for patients with suspected coronary artery disease: the coronary angiography by computed tomography with the use of a submillimeter resolution (CACTUS) trial. Eur Heart J 28(24):3034–3041. doi:10.1093/eurheartj/ehm150
Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB (1975) A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc committee for grading of coronary artery disease, council on cardiovascular surgery, American heart association. Circ J 51(4 Suppl):5–40
Lin F, Shaw LJ, Berman DS, Callister TQ, Weinsaft JW, Wong FJ, Szulc M, Tandon V, Okin PM, Devereux RB, Min JK (2008) Multidetector computed tomography coronary artery plaque predictors of stress-induced myocardial ischemia by SPECT. Atherosclerosis 197(2):700–709. doi:10.1016/j.atherosclerosis.2007.07.002
Task Force for D, Treatment of Non STSEACSoESoC, Bassand JP, Hamm CW, Ardissino D, Boersma E, Budaj A, Fernandez-Aviles F, Fox KA, Hasdai D, Ohman EM, Wallentin L, Wijns W (2007) Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J 28(13):1598–1660. doi:10.1093/eurheartj/ehm161
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15(4):361–387. doi:10.1002/(SICI)1097-0258(19960229)15:4<361:AID-SIM168>3.0.CO;2-4
Team RDC (2008) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria
Andreini D, Pontone G, Mushtaq S, Bertella E, Conte E, Baggiano A, Veglia F, Agostoni P, Annoni A, Formenti A, Montorsi P, Ballerini G, Bartorelli AL, Fiorentini C, Pepi M (2013) Prognostic value of multidetector computed tomography coronary angiography in diabetes: excellent long-term prognosis in patients with normal coronary arteries. Diabetes Care 36(7):1834–1841. doi:10.2337/dc12-2123
Min JK, Labounty TM, Gomez MJ, Achenbach S, Al-Mallah M, Budoff MJ, Cademartiri F, Callister TQ, Chang HJ, Cheng V, Chinnaiyan KM, Chow B, Cury R, Delago A, Dunning A, Feuchtner G, Hadamitzky M, Hausleiter J, Kaufmann P, Kim YJ, Leipsic J, Lin FY, Maffei E, Raff G, Shaw LJ, Villines TC, Berman DS (2014) Incremental prognostic value of coronary computed tomographic angiography over coronary artery calcium score for risk prediction of major adverse cardiac events in asymptomatic diabetic individuals. Atherosclerosis 232(2):298–304. doi:10.1016/j.atherosclerosis.2013.09.025
Lin FY, Shaw LJ, Dunning AM, Labounty TM, Choi JH, Weinsaft JW, Koduru S, Gomez MJ, Delago AJ, Callister TQ, Berman DS, Min JK (2011) Mortality risk in symptomatic patients with nonobstructive coronary artery disease: a prospective 2-center study of 2,583 patients undergoing 64-detector row coronary computed tomographic angiography. J Am Coll Cardiol 58(5):510–519. doi:10.1016/j.jacc.2010.11.078
Muhlestein JB, Lappe DL, Lima JA, Rosen BD, May HT, Knight S, Bluemke DA, Towner SR, Le V, Bair TL, Vavere AL, Anderson JL (2014) Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA 312(21):2234–2243. doi:10.1001/jama.2014.15825
Andreini D, Pontone G, Bartorelli AL, Agostoni P, Mushtaq S, Antonioli L, Cortinovis S, Canestrari M, Annoni A, Ballerini G, Fiorentini C, Pepi M (2010) Comparison of the diagnostic performance of 64-slice computed tomography coronary angiography in diabetic and non-diabetic patients with suspected coronary artery disease. Cardiovasc Diabetol 9:80. doi:10.1186/1475-2840-9-80
Acknowledgments
We are indebted to the medical and technical staff members of the computer tomography laboratory for their invaluable contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Hadamitzky and Dr. Martinoff report receiving unrestricted institutional research grants from Siemens Healthcare. Dr. Hausleiter reports receiving speaker honoraria from Edwards Lifesciences and Abbott Vascular (not related to the current manuscript). The other authors have nothing to disclose. This is an investigator driven study; there is no involvement from outside the departments.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study design was approved by the local ethics committee.
Informed consent
All patients gave written informed consent before examination.
Rights and permissions
About this article
Cite this article
Nadjiri, J., Hausleiter, J., Deseive, S. et al. Prognostic value of coronary CT angiography in diabetic patients: a 5-year follow up study. Int J Cardiovasc Imaging 32, 483–491 (2016). https://doi.org/10.1007/s10554-015-0785-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-015-0785-9