Abstract
Ivabradine, a bradycardic agent, has been shown to stably reduce patient’s heart rate (HR) in the setting of acute cardiac care. However, an association between atrial fibrillation (AF) risk and acute ivabradine treatment remains a controversial clinical issue, and has not been thoroughly investigated. Bradycardia and abnormal atrial refractoriness induced by ivabradine treatment may enhance vulnerability to AF induction, especially when vagal nerve is concurrently activated. We aimed to experimentally investigate the effects of acute ivabradine treatment with/without concurrent vagal activation on AF inducibility. In 16 anesthetized dogs, cervical vagal nerves were prepared for electrical stimulation (VS). AF induction rate (AFIR) was determined by atrial burst pacing. HR, atrial action potential duration (APD), atrial effective refractory period (ERP), and AFIR were obtained consecutively at baseline, during delivery of VS (VS alone), after intravenous injection of ivabradine 0.5 mg/kg (n = 8, ivabradine group) or saline (n = 8, saline group), and again during VS delivery (drug+VS). In the ivabradine group, ivabradine alone significantly lowered HR compared to baseline, while ivabradine+VS significantly lowered HR compared to VS alone. Contrary to expectations, there were no significant differences in trends of APD, temporal dispersion of APD, ERP, and AFIR between ivabradine and saline groups. Irrespective of whether ivabradine or saline was injected, VS significantly shortened APD and ERP, and increased AFIR. Interestingly, although bradycardia in response to ivabradine injection was more intense than that to VS alone, AFIR was significantly lower after ivabradine injection than during VS alone. We conclude that, despite its intense bradycardic effect, acute ivabradine treatment does not increase AF inducibility irrespective of underlying vagal activity. This study may constitute support for the safety of using ivabradine in the setting of acute cardiac care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ivabradine, a bradycardic agent, reduces heart rate (HR) by suppressing the “funny” current expressed in sinoatrial pace-making cells [1]. Large clinical trials have documented the efficacy of chronic ivabradine treatment in improving the outcomes of patients with heart failure or angina pectoris [2, 3]. Several small clinical trials also suggested that acute ivabradine treatment enables stable reduction of HR and improves cardiac function in patients with acute myocardial infarction or acute heart failure [4, 5]. However, an increase in atrial fibrillation (AF) risk associated with the chronic ivabradine treatment has been reported, and confirmed by recent meta-analyses [2, 6–8]. On the other hand, an association between AF risk and the acute ivabradine treatment remains a controversial clinical issue. In patients undergoing cardiac surgery, acute ivabradine treatment was associated with a reduced incidence of AF [9]. In patients with acute myocardial infarction, however, ivabradine treatment was associated with an increase in tachyarrhythmia [10].
Ivabradine can induce profound bradycardia in humans [6, 10]. Ivabradine has been shown to induce sinus arrhythmia in mice [11], which resembles a form of sick sinus syndrome in humans. Sinus node dysfunction and AF frequently coexist and interact with each other [12]. The sinoatrial node plays an active role in terminating atrial tachyarrhythmia [13]. This role can be theoretically hampered by ivabradine [14]. Irrespective of the mechanism of impaired sinus node automaticity, profound bradycardia may facilitate AF occurrence by increasing the temporal and spatial dispersion of atrial refractoriness [12, 15–17]. These findings suggest that ivabradine increases the vulnerability to AF induction and sustenance. However, no previous study has examined effects of acute ivabradine treatment on AF inducibility. Only a single experimental study examined the effects of chronic ivabradine treatment with respect to AF inducibility, and reported that ivabradine reduced the induction and duration of AF in a canine model of age-related AF [18].
Functional status of the autonomic nervous system affects the vulnerability to AF induction [19]. Even if the effect of ivabradine alone is insufficient to induce AF, the effect may be enhanced by concurrent activation of the autonomic nervous system, especially the vagal nerve system [19]. Vagal activation may suppress the active role played by the sinoatrial node in terminating atrial tachyarrhythmia [13], and synergistically increase the dispersion of atrial refractoriness owing to the heterogeneous distribution of vagal innervation throughout the atria [19, 20]. In addition, vagal activation shortens the atrial refractory period, thereby accelerating the development of multiple atrial reentry circuits and AF [19]. Vagal activity shows distinctive variation, especially in the setting of acute cardiac care [21, 22] and likely fluctuates also in patients treated with ivabradine. Taken all these together, we hypothesized that acute ivabradine treatment suppresses the sinoatrial function, increases dispersion of atrial refractoriness, thereby increasing AF inducibility, especially when the vagal nerve is concurrently activated.
The purpose of this study was, therefore, to investigate the effects of acute ivabradine treatment with/without concurrent vagal activation on AF inducibility in dogs. To avoid the confounding effects of atrial pathological remodeling or ischemia, and to directly examine the effects of ivabradine, we used dogs with normal hearts in this study.
Materials and methods
Animals
We used 16 mongrel dogs for laboratory use (8 males and 8 females; Kitayama Labes, Gifu, Japan) [23]. The mean body weight was 22 ± 1 kg, and the mean age was 1.7 ± 0.4 years. Physical and ECG examinations by registered veterinary physicians confirmed that the dogs were free from cardiovascular diseases. The investigation conformed to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996). All protocols were approved by the Animal Subjects Committee of the National Cerebral and Cardiovascular Center.
Preparation
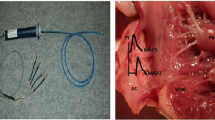
After anesthesia was induced with thiamylal sodium (25 mg kg−1), the animals were intubated endotracheally and ventilated artificially. An appropriate level of anesthesia was maintained by continuous inhalation of 2.0% isoflurane. A catheter-tipped micromanometer (SPC-330A, Millar Instruments, Houston, TX, USA) was inserted via the right femoral artery to measure arterial blood pressure (ABP). A bipolar electrode catheter was inserted via the right jugular vein and attached to the endocardium of the right atrial appendage for pacing using a stimulator (SEN-8203, Nihon Kohden, Tokyo, Japan), which delivered rectangular pulses of 2-ms duration at three times the threshold voltage. The resulting pacing voltage was 2–4 V, and was fixed for individual animals. A Franz catheter (EP Technologies, Palo Alto, CA, USA) was inserted via the right femoral vein and attached to the endocardium of the right atrial lateral wall to record the atrial monophasic action potential (MAP) (filtered at 0.08 and 1000 Hz) [24]. Lead II ECG was recorded from the body surface. Analog signals of ECG, ABP, and MAP were digitized (1000 Hz, 16-bit) by a laboratory computer (LC-72N10, Logitec, Tokyo, Japan), and stored on a hard disk for off-line analysis.
Bilateral cervical vagi were identified and transected at the neck region. Pairs of bipolar electrodes were attached to the cardiac ends of bilateral vagal nerves for electrical stimulation using a stimulator (SEN-8203, Nihon Kohden, Tokyo, Japan) [25]. The duration of electrical pulse was set at 2 ms. We adjusted the amplitude of the pulse in each animal to reduce HR by 20–30% from baseline value at a stimulation frequency of 20 Hz. Eventually, vagal stimulation was conducted at voltages ranging from 4 to 7 V, with voltage fixed for each animal.
Electrophysiological examinations
The duration of MAP at 90% repolarization (APD90) and at 30% repolarization (APD30) were determined during atrial pacing at basic cycle length of 400 ms [25, 26].
For the assessment of the atrial effective refractory period (ERP), the heart was paced with a train of 8 basic (S1) stimuli at cycle length of 400 ms, followed by a premature (S2) stimulus with the coupling interval decreased from 200 to 50 ms in 5-ms steps until capture no longer occurred. The ERP was defined as the longest S1–S2 interval failing to produce a propagated response [25, 26].
We attempted to induce AF by a short burst (3 s) of atrial pacing at 50-ms intervals [25]. Eight attempts were administered. The AF induction rate (AFIR) was defined as the number of induced AF episodes in 8 attempts, expressed as a percentage (%). AF was defined as irregular atrial rates faster than 500 bpm quantified by MAP signals, which were associated with irregular atrioventricular conduction lasting more than 5 s [24–26]. The AF duration was represented by the mean duration of induced AF episodes in each set of attempt. In some attempts, induced irregular atrial beats faster than 500 bpm became regular atrial beats of 400–500 bpm, implying that AF became atrial flutter [26]. In such cases, the duration with mean atrial beats faster than 500 bpm was defined as AF duration.
Experimental protocols
After the initial preparations and surgical procedures were completed, 30 min were allowed for stabilization. Sixteen animals were randomized into two groups: ivabradine (n = 8) and saline (n = 8), and each animal underwent the following four interventions consecutively.
-
1.
Baseline (BASE): In both groups, the hemodynamic parameters; APD, ERP, AFIR and AF duration, were measured at baseline.
-
2.
Vagal stimulation (VS): After BASE, vagal stimulation was started in both groups. A second set of measurements of the hemodynamic and electrophysiological parameters was performed 5 min after initiation of vagal stimulation. After the measurements, vagal stimulation was temporarily suspended.
-
3.
Drug administration (DRUG): In the ivabradine group, an intravenous bolus injection of ivabradine 0.5 mg/kg (Sigma Aldrich) in 10 ml saline was administered via the right femoral vein [27]. In the saline group, only 10 ml of saline was injected. A third set of measurements of the parameters was performed 20 min after administration of ivabradine or saline.
-
4.
Vagal stimulation after drug administration (DRUG+VS): After DRUG intervention, vagal stimulation was re-started in both groups. A fourth set of measurements of the parameters was performed 5 min after initiation of vagal stimulation.
At the conclusion of the experimental protocols, the dogs were euthanized with an intravenous injection of pentobarbital and potassium chloride.
Data analysis and statistics
We determined HR from the ECG R–R intervals. In each intervention, the HR and ABP data were averaged over 30 s under sinus rhythm. The coefficient of variability (CV = SD/mean × 100) for the ECG R–R intervals (CVRR) during the 30-s period was calculated as a measure of the spontaneous HR variation [28]. Data of APD90 and APD30 were averaged over 5 s under atrial pacing at basic cycle length of 400 ms. CV of APD90 (CVAPD90) during the 5-s pacing period of 12 beats was calculated as a measure of temporal dispersion of APD [29].
All data are presented as mean ± SEM. Data were analyzed using unpaired Student’s t-tests (ivabradine vs saline groups) or a two-way analysis of variance for repeated measures (effects of group, intervention, and their interaction) with Tukey’s post hoc test (pairwise comparison). A P value less than 0.05 was considered statistically significant. Statistical analyses were performed using commercially available software (Statistica, Statsoft, Inc., Tulsa, OK, USA).
Results
All the 16 animals completed the experimental protocols. The stimulation voltage for right atrial pacing used in ivabradine group (3.0 ± 0.1 V) was similar to that used in saline group (3.1 ± 0.1 V) (P = 0.316). The strength of vagal stimulation used in ivabradine group (6.1 ± 0.4 V) was similar to that used in saline group (5.9 ± 0.3 V) (P = 0.745).
Figure 1 shows representative time traces of ECG, ABP and MAP for one animal in the ivabradine group during the four interventions, recorded under sinus rhythm and under atrial pacing at basic cycle length of 400 ms. At VS, HR decreased while APD90, APD30, and ERP were shortened from those observed at BASE. At DRUG, administration of ivabradine also decreased HR from that seen in BASE, but APD90, APD30, and ERP were shortened to a less extent compared to those at VS. At DRUG+VS, HR showed further reduction, while APD90, APD30, and ERP were similar to those seen at VS.
Representative time traces of hemodynamics and monophasic action potentials of one dog in ivabradine group during the four interventions: baseline (BASE), vagal stimulation (VS), intravenous ivabradine (DRUG), and intravenous ivabradine with vagal stimulation (DRUG+VS). Upper row, tracings obtained during sinus rhythm; lower row, tracings obtained during atrial pacing at basic cycle length (BCL) of 400 ms. HR indicates heart rate, ABP arterial blood pressure, MAP monophasic action potential, APD90 duration of MAP determined at 90% repolarization, APD30 duration of MAP determined at 30% repolarization, ERP effective refractory period
Figure 2a shows individual time courses of the ECG R–R intervals under sinus rhythm for eight animals in the ivabradine group during the four interventions. In most recordings, R–R intervals showed minor fluctuations over time, probably due to the artificial ventilation. We observed atrial arrhythmia in 2 dogs after ivabradine administration (dogs #7 and #8 at DRUG), and in 3 dogs under vagal stimulation after ivabradine administration (dogs #3, #6, and #8 at DRUG+VS), in which the R–R intervals showed non-periodic and rather chaotic fluctuations independent of artificial ventilation. ECG traces obtained in dogs #7 and #8 during DRUG, and in dogs #3, #6, and #8 during DRUG+VS indicated varying P-wave morphology (Fig. 2b). In Fig. 2c, we superimposed 4 traces of the P-waves, which were extracted from the ECG trace in dog #6 in Fig. 2b. Black-colored trace indicated normal P-wave morphology, while other 3 traces of the P-wave were characterized by a variety of morphology with different amplitude and/or bifid shape.
a Time traces of the ECG R–R intervals under sinus rhythm for eight animals in the ivabradine group during the four interventions: baseline (BASE), vagal stimulation (VS), intravenous ivabradine (DRUG), and intravenous ivabradine with vagal stimulation (DRUG+VS). Data of each dog is color-coded as shown in the panel. b Time traces of lead II ECG obtained from dogs #7 and #8 during DRUG, from dogs #3, #6, and #8 during DRUG+VS. c Superimposed time traces of the P-waves extracted from the time trace of ECG in dog#6 in b. After extracting the P-waves in 100 ms-long window starting 90 ms before the corresponding R-wave, offset amplitude was adjusted to remove baseline wander, on each P-wave. Color-coded P-wave in c was the P-wave indicated by the corresponding color-coded arrow in b
Figure 3 shows the time traces of MAP of one animal in the ivabradine group during the four interventions. In each intervention, eight attempts were made to induce AF by 3-s burst pacing. At BASE, no AF was induced. At VS, HR was reduced to 90 bpm from 110 bpm seen at BASE, while AF was induced 4 times during the 8 attempts. At DRUG, administration of ivabradine reduced HR to 79 bpm, but no AF was induced. At DRUG+VS, HR was further reduced to 64 bpm, but AF was induced at similar frequency as that at VS.
Time traces of monophasic action potential (MAP) of one animal in ivabradine group, when 3-s burst pacing was delivered to induce AF. The burst pacing (gray bar) was attempted 8 times in each intervention: baseline (BASE), vagal stimulation (VS), intravenous ivabradine (DRUG), and intravenous ivabradine with vagal stimulation (DRUG+VS). Red-colored traces are defined as AF. AFIR indicates AF induction rate
As shown in Fig. 4a, the two-way repeated measures analysis of variance indicated that HR in the ivabradine group was significantly lower than that in the saline group when group averages were compared. The nonparallel trends of HR indicate significant interactions between group and intervention. HR at DRUG was significantly lower in the ivabradine group than in the saline group. Within the ivabradine group, vagal stimulation alone (VS) decreased HR significantly compared to BASE, while ivabradine alone (DRUG) decreased HR significantly compared to VS. Ivabradine with vagal stimulation (DRUG+VS) reduced HR significantly compared to ivabradine alone (DRUG). As shown in Fig. 4b, significant interaction between group and intervention was noted in the trends of CVRR. Within the ivabradine group, CVRR at DRUG+VS was significantly larger than that at BASE. As shown in Fig. 4c, ABP in the ivabradine and saline groups were similar when group averages were compared. When both groups were combined, effect of intervention on the trend of ABP was significant. ABP at VS, DRUG, and DRUG + VS were significantly lower than that at BASE. Non-significant interaction between group and intervention indicated that ivabradine injection did not affect ABP significantly.
a HR, b coefficient of variability of the ECG R–R intervals (CVRR), and c ABP obtained during the four interventions: baseline (BASE), vagal stimulation (VS), drug administration (DRUG), and vagal stimulation after drug administration (DRUG+VS). Error bars indicate SEM. Solid line indicates ivabradine group (n = 8); dashed line, saline group (n = 8). Probability values derived from a two-way analysis of variance for repeated measures are shown. *P < 0.05, † P < 0.01 derived from Tukey’s post hoc test
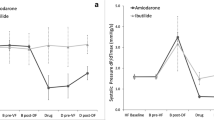
There were no significant differences in APD90 (Fig. 5a), CVAPD90 (Fig. 5b), APD30 (Fig. 5c), ERP (Fig. 5d), AFIR (Fig. 5e), and AF duration (Fig. 5f) between ivabradine and saline groups when group averages were compared. There was no significant effect of intervention or of interaction on the trends of CVAPD90 (Fig. 5b). The parallel trends of APD90 (Fig. 5a), APD30 (Fig. 5c), ERP (Fig. 5d), and AFIR (Fig. 5e) indicate non-significant interactions between groups and interventions. APD90, APD30, and ERP were significantly shortened, and AFIR was significantly increased by vagal stimulation. These vagal effects were similar between the two groups. AFIR at DRUG (ivabradine) in dogs #7 and #8 (Fig. 2) were 25 and 0%, respectively. AFIR at DRUG (ivabradine)+VS in dogs #3, #6, and #8 (Fig. 2) were 38, 25, and 38%, respectively. AF stopped spontaneously within 3 min in all except two animals. In one dog in the saline group, AF induced at BASE was terminated only by delivering electrical shock. In one dog (dog #4 in Fig. 2) in the ivabradine group, AF induced at VS was terminated only by stopping the stimulation. Therefore, data of AF duration obtained in these two dogs were not used. There were no significant differences in AF duration at DRUG and also at DRUG + VS between the two groups (Fig. 5f). AF duration at DRUG (ivabradine) in dog #7 (Fig. 2) was 14.0 ± 7.0 s. AF duration at DRUG (ivabradine)+VS in dogs #3, #6, and #8 (Fig. 2) were 11.2 ± 4.1, 6.8 ± 0.9 and 9.1 ± 2.3 s, respectively.
a APD90, b coefficient of variability of APD90 (CVAPD90), c APD30, d ERP, e AFIR and f AF duration obtained during the four interventions: baseline (BASE), vagal stimulation (VS), drug administration (DRUG), and vagal stimulation after drug administration (DRUG+VS). Error bars indicate SEM. Solid line indicates ivabradine group (n = 8 in a–e, n = 7 in f); dashed line, saline group (n = 8 in a–e, n = 7 in f). Probability values derived from a two-way analysis of variance for repeated measures are shown. *P < 0.05, † P < 0.01 derived from Tukey’s post hoc test
Discussion
To the best of our knowledge, this is the first report on the effects of acute ivabradine treatment, and concurrent vagal activation on AF induction. Contrary to our hypothesis, acute ivabradine administration, both alone and concurrently with vagal nerve activation, did not increase AF inducibility or sustainability. Interestingly, although bradycardia in response to ivabradine administration was more intense than that to vagal stimulation alone, AFIR after ivabradine administration was significantly lower than that during vagal stimulation alone. The present results suggest that at least in subjects with normal hearts, acute ivabradine treatment may not increase the risk of AF induction even when the vagal activity increases drastically.
As shown in Fig. 1, MAP obtained in the canine right atrium in this study showed triangular shape with its amplitude (baseline to plateau crest) of around 10 mV. These are compatible to previous findings in canine or human right atrium [30] [31]. Values of baseline APD90 and ERP during atrial pacing at basic cycle length of 400 ms (Figs. 1, 5a, d) are similar to those reported previously in dogs [31, 32]. The results that the values of ERP (Fig. 5d) lied between those of APD90 (Fig. 5a) and APD30 (Fig. 5c) within each intervention are reasonably compatible with the previous finding that ERP is most closely reflected by APD70 [33]. MAP amplitude at VS was slightly less than that at BASE or at DRUG in the animal in Fig. 1, and also in some other animals (data not shown). Suppression of atrial contractile force by VS might reduce the contact pressure between the electrode tip and the endocardial wall during atrial systole [34], thereby slightly reducing the amplitude of MAP [35]. We do not think that these minor changes in MAP amplitude affected the conclusion of this study, because the computation of the electrophysiological parameters was theoretically independent of the absolute amplitude of MAP.
We confirmed that automaticity of the sinoatrial node is indeed suppressed acutely by ivabradine treatment without affecting AF inducibility. Previous experimental and theoretical analyses suggested that ivabradine treatments and vagal activation may prevent the sinoatrial node from terminating atrial tachyarrhythmia by suppressing its automaticity and interrupting the sinoatrial conduction [13, 14]. In mice, ivabradine at doses higher than 10 mg/kg reduced HR by more than 50% and induced a periodic fluctuation of the ECG R–R interval [11], resembling a second-degree sinoatrial block in humans. In this study, we observed non-periodic and rather chaotic atrial arrhythmia in 2 of 8 dogs in response to ivabradine injection alone, and in 3 of 8 dogs given ivabradine and vagal stimulation (Fig. 2). Detailed analysis of the P-wave morphologies in the dogs suggested that the arrhythmia was initiated by shifts in sinoatrial-nodal or shifts to extra sinoatrial-nodal pacemaker localization, i.e., ectopic atrial beats [36]. The atrial arrhythmia observed in this study did not resemble the second-degree sinoatrial block observed previously in mice [11]. In any way, overall, the AFIR and AF duration in these dogs did not increase. Ivabradine injection showed the tendency to increase HR variability, especially under vagal activation (Fig. 4b). Increase in the HR variability after ivabradine injection was caused partly by the emergence of the atrial ectopic beats, and also likely caused by an increase in spontaneous variation in intrinsic sinus beats [28]. However, the degree of the HR variability and that of AF inducibility were not always associated (Figs. 4b vs 5e). We used an ivabradine dose of 0.5 mg/kg in the present study. The dose of ivabradine used in this study and the degree of HR changes following administration seem to be somewhat greater than those relevant to clinical practice [4, 5, 9, 10]. This might promote the occurrence of the atrial ectopic beats. Although use of a higher dose might have induced sinoatrial block and significantly increased AF inducibility, a further increase in ivabradine dose would be irrelevant to clinical practice.
Vagal activation reduces HR by inhibiting the funny current in the sinoatrial node, while shortening APD and ERP in the sinoatrial node and atrial tissue mainly by opening acetylcholine-sensitive outward potassium current, thereby accelerating the development of multiple atrial reentry circuits and AF [19]. The present results indicate that irrespective of the underlying vagal activity, selective inhibition of the funny current by intravenous ivabradine does not affect APD or ERP in the right atrium, which may be one reason why acute ivabradine treatment does not increase AF. Our finding on ERP is in line with a previous study in patients with normal baseline electrophysiology [37], in which a single intravenous administration of ivabradine significantly reduced HR, but did not change ERP of the right atrium. On the other hand, in aged dogs (mean age 8–10 years) with atrial pathological remodeling, Li et al. [18] demonstrated that chronic administration of ivabradine increased ERPs in the atrium and the pulmonary vein. Interestingly, they found that administration of ivabradine increased the spatial dispersion of ERPs, but reduced AF induction. These previous experimental studies, however, did not evaluate the electrophysiological parameters in association with varied vagal activity. We observed that intravenous ivabradine does not significantly increase the temporal dispersion of APD. There has been a paucity of data on temporal dispersion of atrial APD during ivabradine treatment. Only one in vitro study using isolated sinoatrial node cells demonstrated that ivabradine does not significantly increase the temporal dispersion of APD [28]. Increase in temporal dispersion of APD, i.e., dispersion of refractoriness, has been shown to be a major contributor to arrhythmogenesis [29]. The fact that irrespective of the underlying vagal activity, intravenous ivabradine does not increase the temporal dispersion of APD in the right atrium may be another reason why acute ivabradine treatment does not increase AF. Since we did not detect any significant effects of ivabradine on these electrophysiological parameters and AF inducibility, we did not further evaluate the effects of ivabradine on the spatial dispersion of atrial APDs or ERPs using additional preparations and interventions [38].
We evaluated the effects of acute ivabradine treatment and vagal activation on AF inducibility, but not on spontaneous AF. An increase in the time window due to sinus bradycardia induced by concurrent ivabradine treatment and vagal activation may facilitate AF occurrence by increasing atrial ectopy and also by increasing the pulmonary vein arrhythmogenesis [12, 39, 40]. Suenari et al. [41] demonstrated that acute ivabradine treatment decreased the spontaneous activity in pulmonary vein cardiomyocytes in rabbits. However, they did not evaluate the occurrence of spontaneous AF. We observed multiple atrial ectopic beats in some dogs in the ivabradine group (Fig. 2). However, we did not observe any spontaneous AF during the short observation period of this study. Although beyond the scope of the present study, to evaluate the effects of acute ivabradine treatment on the occurrence of spontaneous AF, different experimental settings including ivabradine administration and more-prolonged instrumentation for vagal stimulation and recording of atrial electrical activity would be necessary [42].
This study may constitute support for the safety of using ivabradine in the setting of acute cardiac care. In this setting, a reduction in HR may be a useful target, because this intervention can reduce myocardial oxygen consumption and improve coronary blood flow [4, 27, 43]. Different from the beta-blockers, ivabradine minimally affects cardiac contractility and systemic hemodynamics while reducing HR [1, 4, 5, 27, 44]. In accordance with the previous studies, we noted in this study that ivabradine significantly reduces HR without affecting ABP (Fig. 4a vs c). That is a hemodynamic advantage, especially in the setting of acute cardiac care. Furthermore, in those settings, induction of AF as a drug side effect can have deleterious effects on hemodynamics. The present results, however, suggest that such concern may not be relevant to acute ivabradine treatment.
Limitations
One limitation of the present study was that the sample size might not be large enough to detect small but significant changes in AF inducibility caused by acute ivabradine treatment. Indeed, increase in the relative risk of AF attributable to chronic ivabradine treatment in clinical trials has been reported to be significant, but not so large, ≈15% [7]. Another limitation was that AF inducibility was examined in the atrium of normal hearts in young anesthetized dogs. Abnormal electrical and structural atrial remodeling and/or atrial ischemia can be a substrate for AF in aged patients with hypertension, heart failure, and/or myocardial infarction [18]. In this study, we avoided the confounding effects of atrial remodeling and/or atrial ischemia to directly examine the effects of acute ivabradine treatment and vagal activation on AF inducibility. However, caution should be exercised in extrapolating the present results to subjects with the extensive pathological changes in the atrium. To address these issues, further studies are required in the future.
Conclusions
Despite its potent bradycardic effect, ivabradine does not increase AF inducibility or sustainability irrespective of underlying vagal activity. The present results suggest that at least in subjects with normal hearts, acute ivabradine treatment may not increase the risk of AF even when the vagal activity increases drastically.
References
DiFrancesco D (2010) The role of the funny current in pacemaker activity. Circ Res 106:434–446
Swedberg K, Komajda M, Böhm M, Borer JS, Ford I, Dubost-Brama A, Lerebours G, Tavazzi L, Investigators SHIFT (2010) Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 376:875–885
Fox K, Ford I, Steg PG, Tendera M, Ferrari R, Investigators BEAUTIFUL (2008) Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial. Lancet 372:807–816
Fasullo S, Cannizzaro S, Maringhini G, Ganci F, Giambanco F, Vitale G, Pinto V, Migliore G, Torres D, Sarullo FM, Paterna S, Di Pasquale P (2009) Comparison of ivabradine versus metoprolol in early phases of reperfused anterior myocardial infarction with impaired left ventricular function: preliminary findings. J Card Fail 15:856–863
Hidalgo FJ, Anguita M, Castillo JC, Rodríguez S, Pardo L, Durán E, Sánchez JJ, Ferreiro C, Pan M, Mesa D, Delgado M, Ruiz M (2016) Effect of early treatment with ivabradine combined with beta-blockers versus beta-blockers alone in patients hospitalised with heart failure and reduced left ventricular ejection fraction (ETHIC-AHF): a randomised study. Int J Cardiol 217:7–11
Fox K, Ford I, Steg PG, Tardif JC, Tendera M, Ferrari R, SIGNIFY investigators (2015) Bradycardia and atrial fibrillation in patients with stable coronary artery disease treated with ivabradine: an analysis from the SIGNIFY study. Eur Heart J 36:3291–3296
Martin RI, Pogoryelova O, Koref MS, Bourke JP, Teare MD, Keavney BD (2014) Atrial fibrillation associated with ivabradine treatment: meta-analysis of randomised controlled trials. Heart 100:1506–1510
Cammarano C, Silva M, Comee M, Donovan JL, Malloy MJ (2016) Meta-analysis of ivabradine in patients with stable coronary artery disease with and without left ventricular dysfunction. Clin Ther 38:387–395
Abdel-Salam Z, Nammas W (2016) Atrial fibrillation after coronary artery bypass surgery: can ivabradine reduce its occurrence? J Cardiovasc Electrophysiol 27:670–676
Steg P, Lopez-de-Sà E, Schiele F, Hamon M, Meinertz T, Goicolea J, Werdan K, Lopez-Sendon JL, VIVIFY (eValuation of the IntraVenous If inhibitor ivabradine after STsegment elevation mYocardial infarction) investigators (2013) Safety of intravenous ivabradine in acute ST-segment elevation myocardial infarction patients treated with primary percutaneous coronary intervention: a randomized, placebo-controlled, double-blind, pilot study. Eur Heart J Acute Cardiovasc Care 2:270–279
Stieber J, Wieland K, Stöckl G, Ludwig A, Hofmann F (2006) Bradycardic and proarrhythmic properties of sinus node inhibitors. Mol Pharmacol 69:1328–1337
John RM, Kumar S (2016) Sinus node and atrial arrhythmias. Circulation 133:1892–1900
Fedorov VV, Chang R, Glukhov AV, Kostecki G, Janks D, Schuessler RB, Efimov IR (2010) Complex interactions between the sinoatrial node and atrium during reentrant arrhythmias in the canine heart. Circulation 122:782–789
Cacciani F, Zaniboni M (2015) Chronotropic modulation of the source-sink relationship of sinoatrial-atrial impulse conduction and its significance to initiation of AF: a one-dimensional model study. Biomed Res Int 2015:496418
Han J, Millet D, Chizzonitti B, Moe GK (1966) Temporal dispersion of recovery of excitability in atrium and ventricle as a function of heart rate. Am Heart J 71:481–487
Elvan A (2001) Sinoatrial remodeling caused by persistent atrial fibrillation: what is the relationship between postcardioversion sinus node dysfunction and increased atrial vulnerability? J Cardiovasc Electrophysiol 12:807–808
Spach MS, Dolber PC, Heidlage JF (1989) Interactions of inhomogeneities of repolarization with anisotropic propagation in dog atria: a mechanism for both preventing and initiating re-entry. Circ Res 65:1612–1631
Li YD, Ji YT, Zhou XH, Jiang T, Hong YF, Li JX, Xing Q, Xiong J, Yusufuaji Y, Tang BP (2015) Effects of ivabradine on cardiac electrophysiology in dogs with age-related atrial fibrillation. Med Sci Monit 21:1414–1420
Chen PS, Chen LS, Fishbein MC, Lin SF, Nattel S (2014) Role of the autonomic nervous system in atrial fibrillation: pathophysiology and therapy. Circ Res 114:1500–1515
Liu L, Nattel S (1997) Differing sympathetic and vagal effects on atrial fibrillation in dogs: role of refractoriness heterogeneity. Am J Physiol 273:H805–H816
Bonnemeier H, Hartmann F, Wiegand UK, Irmer C, Kurz T, Tölg R, Katus HA, Richardt G (2000) Heart rate variability in patients with acute myocardial infarction undergoing primary coronary angioplasty. Am J Cardiol 85:815–820
Chiladakis JA, Patsouras N, Manolis AS (2003) The Bezold-Jarisch reflex in acute inferior myocardial infarction: clinical and sympathovagal spectral correlates. Clin Cardiol 26:323–328
Uemura K, Inagaki M, Zheng C, Li M, Kawada T, Sugimachi M (2015) A novel technique to predict pulmonary capillary wedge pressure utilizing central venous pressure and tissue Doppler tricuspid/mitral annular velocities. Heart Vessels 30:516–526
Narayan SM, Franz MR (2007) Quantifying fractionation and rate in human atrial fibrillation using monophasic action potentials: implications for substrate mapping. Europace 9:vi89–vi95
Kanki H, Mitamura H, Takatsuki S, Sueyoshi K, Shinagawa K, Sato T, Ogawa S (1998) Postrepolarization refractoriness as a potential anti-atrial fibrillation mechanism of pilsicainide, a pure sodium channel blocker with slow recovery kinetics. Cardiovasc Drugs Ther 12:475–482
Lu Z, Scherlag BJ, Lin J, Niu G, Fung KM, Zhao L, Ghias M, Jackman WM, Lazzara R, Jiang H, Po SS (2008) Atrial fibrillation begets atrial fibrillation: autonomic mechanism for atrial electrical remodeling induced by short-term rapid atrial pacing. Circ Arrhythm Electrophysiol 1:184–192
Colin P, Ghaleh B, Monnet X, Hittinger L, Berdeaux A (2004) Effect of graded heart rate reduction with ivabradine on myocardial oxygen consumption and diastolic time in exercising dogs. J Pharmacol Exp Ther 308:236–240
Zaniboni M, Cacciani F, Lux RL (2014) Beat-to-beat cycle length variability of spontaneously beating guinea pig sinoatrial cells: relative contributions of the membrane and calcium clocks. PLoS One 9:e100242
Zaniboni M, Pollard AE, Yang L, Spitzer KW (2000) Beat-to-beat repolarization variability in ventricular myocytes and its suppression by electrical coupling. Am J Physiol Heart Circ Physiol 278:H677–H687
Franz MR (1983) Long-term recording of monophasic action potentials from human endocardium. Am J Cardiol 51:1629–1634
Ashikaga K, Kobayashi T, Kimura M, Owada S, Sasaki S, Iwasa A, Furukawa K, Motomura S, Okumura K (2006) Effects of amiodarone on electrical and structural remodeling induced in a canine rapid pacing-induced persistent atrial fibrillation model. Eur J Pharmacol 536:148–153
Kabell G, Buchanan LV, Gibson JK, Belardinelli L (1994) Effects of adenosine on atrial refractoriness and arrhythmias. Cardiovasc Res 28:1385–1389
Bode F, Kilborn M, Karasik P, Franz MR (2001) The repolarization-excitability relationship in the human right atrium is unaffected by cycle length, recording site and prior arrhythmias. J Am Coll Cardiol 37:920–925
Tsuboi M, Furukawa Y, Nakajima K, Kurogouchi F, Chiba S (2000) Inotropic, chronotropic, and dromotropic effects mediated via parasympathetic ganglia in the dog heart. Am J Physiol Heart Circ Physiol 279:H1201–H1207
Franz MR (1999) Current status of monophasic action potential recording: theories, measurements and interpretations. Cardiovasc Res 41:25–40
Goldberg JM, Lynn-Johnson MH, Neely B (1981) Use of P wave morphology for inferring pacemaker localization along the sulcus terminalis in the dog. J Electrocardiol 14:115–124
Camm AJ, Lau CP (2003) Electrophysiological effects of a single intravenous administration of ivabradine (S 16257) in adult patients with normal baseline electrophysiology. Drugs R D 4:83–89
Roithinger FX, Karch MR, Steiner PR, SippensGroenewegen A, Lesh MD (1999) The spatial dispersion of atrial refractoriness and atrial fibrillation vulnerability. J Interv Card Electrophysiol 3:311–319
Sugimura S, Kurita T, Kaitani K, Yasuoka R, Miyazaki S (2016) Ectopies from the superior vena cava after pulmonary vein isolation in patients with atrial fibrillation. Heart Vessels 31:1562–1569
Jiang Z, Yin H, He Y, Ma N, Tang M, Liu H, Ding F, Mei J (2015) Efficacy and safety of novel epicardial circumferential left atrial ablation with pulmonary vein isolation in sustained atrial fibrillation. Heart Vessels 30:675–681
Suenari K, Cheng CC, Chen YC, Lin YK, Nakano Y, Kihara Y, Chen SA, Chen YJ (2012) Effects of ivabradine on the pulmonary vein electrical activity and modulation of pacemaker currents and calcium homeostasis. J Cardiovasc Electrophysiol 23:200–206
Zhang Y, Ilsar I, Sabbah HN, Ben David T, Mazgalev TN (2009) Relationship between right cervical vagus nerve stimulation and atrial fibrillation inducibility: therapeutic intensities do not increase arrhythmogenesis. Heart Rhythm 6:244–250
De Ferrari GM, Mazzuero A, Agnesina L, Bertoletti A, Lettino M, Campana C, Schwartz PJ, Tavazzi L (2008) Favourable effects of heart rate reduction with intravenous administration of ivabradine in patients with advanced heart failure. Eur J Heart Fail 10:550–555
Colin P, Ghaleh B, Monnet X, Su J, Hittinger L, Giudicelli JF, Berdeaux A (2003) Contributions of heart rate and contractility to myocardial oxygen balance during exercise. Am J Physiol Heart Circ Physiol 284:H676–H682
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This work was supported by JSPS KAKENHI Grant No. 15K01307, and also by Practical Research Project for Life-Style related Diseases including Cardiovascular Diseases and Diabetes Mellitus from Japan Agency for Medical Research and Development.
Rights and permissions
About this article
Cite this article
Uemura, K., Inagaki, M., Zheng, C. et al. Acute ivabradine treatment reduces heart rate without increasing atrial fibrillation inducibility irrespective of underlying vagal activity in dogs. Heart Vessels 32, 484–494 (2017). https://doi.org/10.1007/s00380-016-0922-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-016-0922-y