Abstract
Purpose
To compare the effects of class III antiarrhythmic agents (amiodarone vs. ibutilide) on ventricular fibrillation (VF) and hemodynamic status in a canine heart failure (HF) model.
Methods
A total of 12 beagles were used to establish the HF model by rapid pacing for 4 consecutive weeks. These canines were randomly divided into two groups based on the administration of ibutilide and amiodarone. A 12 × 12 unipolar electrode plaque was used for ventricular epicardial mapping, and a 6-electrode plunge needle was inserted for ventricular transmural mapping. The restitution curve was estimated from activation recovery intervals (ARIs) by pacing from the plaque electrodes before and after drug administration. The defibrillation threshold (DFT) and VF activation patterns, including the activation rate, cycle length (VF-CL) and the transmural dispersion of the activation rate, were evaluated and the hemodynamic parameters were mearsured and compared before and after drug administration.
Results
Compared to HF baseline, ibutilide administration has markedly decreased the DFT by 28% (18 ± 2 J vs. 13 ± 2.7 J, P < 0.01) without affecting the canine’s hemodynamics (mean arterial pressure 91 ± 15 mmHg vs. 92 ± 17 mmHg, P > 0.05). Furthermore, VF activation pattern became more organized, and spontaneous termination was observed only after ibutilide administration. Conversely, amiodarone has significantly compromised the hemodynamic status (mean arterial pressure 92 ± 6.1 mmHg vs. 52 ± 11.6 mmHg, P < 0.05), but did not alter the DFT (17 ± 2.3 J vs. 16 ± 2.0 J, P > 0.05). Compared to pre-medication, both ibutilide and amiodarone have significantly prolonged the VERP (178 ± 9.6 ms vs. 208 ± 8.9 ms, P < 0.05; 185 ± 10.5 ms vs. 202 ± 7.5 ms, P < 0.05, respectively) and reduced the dispersion of refractoriness, the maximal slope of restitution curve, and the epicardial dispersion during pacing. Additionally, both drugs have significantly increased the VF-CL and reduced the transmural dispersion of the VF activation rate.
Conclusions
Ibutilide had potential antifibrillatory properties, which was shown by decreasing the DFT and organizing the VF activation in HF, and with no apparent impact on the hemodynamic status. In contrast, intravenous amiodarone administration demonstrated prominent negative effects on the hemodynamic status possibly by affecting the myocardial contractility before and after defibrillation but did not alter the DFT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sudden cardiac death (SCD) due to ventricular fibrillation (VF) is a significant cause of mortality in patients with heart failure (HF). Electrical defibrillation and antiarrhythmic drug administration are used as the primary emergency treatments for SCD patients [1,2,3]. Currently, class III antiarrhythmic drugs, such as amiodarone, are widely used for treating life-threatening ventricular arrhythmias (VAs) in clinic. However, the clinical utility of these agents in acute severe conditions might be limited as they tend to compromise the hemodynamic function, presented as hypotension and lowered myocardial function [4, 5]. Ibutilide is a class III antiarrhythmic drug that is routinely used for the treatment of atrial arrhythmia, and exerts a potential antiarrhythmic effect on VAs in both animal studies as well as clinical observations [6,7,8,9,10]. Our previous animal study showed that ibutilide markedly decreased ventricular defibrillation threshold (DFT) by reducing the complexity of the activation pattern during VF in normal canines [11]. Stambler et al. [12] have demonstrated that ibutilide did not cause clinically important adverse hemodynamic effects, even in patients with depressed cardiac function. However, the mechanism and efficacy of defibrillation might differ as the mechanism of VF maintenance and activation patterns alter in different pathological heart models [13]. Hitherto, this pharmacological approach has only been partially studied in healthy animal hearts, and few studies have examined the detailed mechanism of ibutilide on VF in patients with HF. Furthermore, we hypothesized a potential interaction between the defibrillation efficacy and hemodynamic performance. In the present study, we aimed to investigate the pharmacological modifications of electrophysiological parameters and their effect on the hemodynamic status by ibutilide and amiodarone. Also the potential electrophysiological mechanism underlying the alteration of VF properties in a canine model of pacing-induced HF was explored.
Methods
Animal Preparation
Twelve beagles (weighing 12.5 ± 1.5 kg) were included in the present study. Ketamine (10 mg/kg) and atropine (0.04 mg/kg) were given intramuscularly to anesthetize the animals. After the placement of an endotracheal tube, propofol (1–2 mg/kg/min) intravenously (i.v.) and isoflurane (1–3%) inhalation combined with general anesthesia were administered along with fentanyl (1–2 μg/kg i.v., intermittently repeated as needed) for anesthetization. All surgeries, including pacemaker implantation and electrophysiological studies, were carried out under general anesthesia. The animals were provided with ventilation by placing them in a dorsally recumbent position. In addition, much attention was paid to the degree of muscle tone to maintain good ventilation. Mechanical ventilation (Datex-Ohmeda 7100, General Electric, Inc., Milwaukee, CT, USA) provided a fraction of inspired oxygen (Fi,O2) of 0.5 and a tidal volume of 12 ml/kg, with a breathing frequency of approximately 15 breaths/min. The heart rate (HR), respiratory rate, and peripheral O2 saturation of the animals were monitored during the experiment. Electrocardiogram (ECG) and arterial blood pressure (BP) were also continuously monitored throughout the study. At the end of the experiment, the animals were euthanized by intravenous administration of a lethal dose of sodium pentobarbital (150 mg/kg) under general anesthesia. All possible animal suffering was carefully avoided throughout the experiment.
Pacemaker Implantation
To establish HF model, a ventricular pacing lead (5076, Medtronic, Inc., Minneapolis, MN, USA) was positioned at the right ventricular apex via the right internal jugular vein under fluoroscopic visualization, a pacemaker (Kappa 710, Medtronic, Inc. Minneapolis, MN, USA) was placed in the subcutaneous chest pocket, and then connected to the ventricular pacing lead. A dose of prophylactic antibiotic (cefradine, 12.5 mg/kg) was injected intramuscularly before pacemaker implantation, and then for 3 consecutive days after the surgery. Next, a rapid ventricular pacing at 230 beats/min was initiated immediately after implantation. Daily surveillance of vital signs, pacemaker incision healing, appetite, activity, and/or mental status were recorded on each animal’s log chart. Rapid pacing was proceeded for at least 4 weeks and maintained till the day of electrophysiological mapping study.
Echocardiography and Animal Grouping
Transthoracic echocardiography was performed for all the beagles before and 4 weeks after pacemaker implantation. Echocardiographic examination was conducted by placing the beagles in left decubitus position while they were awake. Left ventricular (LV) systolic function was assessed by measuring the left ventricular ejection fraction (LVEF) and the left ventricular end-diastolic diameter (LVEDD). After that, all the animals were randomly divided into two groups to exclude any significant differences between the two groups in HF baseline condition. Echocardiographic data were acquired and analyzed by an independent investigator.
Hemodynamics and ECG Data Measurement
In the present study, before drug administration, HR, systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), and SBP dP/dTmax of the two groups were measured. The average amplitude of QRS complex of the last five clear waveforms on limb leads I, II, and aVF before and after defibrillation were recorded to evaluate the effect of both drugs on cardiac contractility as well as the QTc and R-R intervals. After successful defibrillation, the average of the initial five cardiac cycles was calculated to evaluate the hemodynamics and assess the ECG data. After administration of the two agents, all data were measured again.
MAP was calculated by SBP and DBP.
MAP = (SBP + 2 × DBP)/3;
The SBP dP/dTmax was acquired to assess the myocardial contractility.
Electrophysiological Study
Pacing Protocol
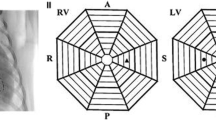
The epicardium was exposed through a median sternotomy, and the heart was supported in a pericardial sling. A 144-electrode (12 × 12, 2-mm spacing) plaque was sutured on the LV lateral epicardium to perform epicardial mapping of the LV, and a 6-unipolar electrode plunge needle (2-mm spacing) was plunged into the LV myocardium at the apex region to record transmural activation. A defibrillation catheter (model 80,993, IBI, St. Jude Medical, Inc., Minneapolis, MN, USA) was placed intravenously, in which the negative electrodes were placed at the right ventricular apex and the positive electrodes in the superior vena cava. The defibrillation technique has been performed as described previously [13].
Measurement of the Ventricular Effective Refractory Period (VERP)
An incremental S1S2 pacing protocol was used to determine the VERP (MicroPaceIII, EPS320 Cardiac Stimulator, Micropace EP, Inc., Santa Ana, CA, USA). All stimuli were delivered at twice the output of the diastolic threshold. The S1S1 interval was 300 ms (8 beats), and the initial S1S2 interval was 250 ms. The S1S2 coupling interval was progressively shortened in steps of 10 ms, starting from 250 ms until the refractoriness was detected. The coupling interval was then increased by 20 ms to restore capturing, and it was subsequently shortened by 2-ms step decrements until the occurrence of ventricular refractoriness. The VERP was defined as the longest S1S2 interval failed to capture.
Restitution Pacing Protocol
The restitution relationship was determined based on programmed pacing. We used 30 beats as the baseline pacing cycle length (PCL) to ensure a stable capture and avoided severe ischemia that might cause a long and fast pacing period [14, 15]. The train of 30 stimulis was repeated at the following intervals: the pacing interval was decreased by 10 ms from 300 ms till an interval at which VF was induced or when the 1:1 capture was lost. Continued pacing was used to maximize the capture at shorter pacing intervals. The 300-ms interval was continued and progressively decreased in 10-ms steps until the target interval was reached. Subsequently, the S1S1 interval was maintained at the target interval for 30 beats. After each pacing protocol, a 5-min rest was given to allow the hemodynamic status of the animal to return to the baseline level.
Activation Recovery Interval (ARI) Measurements
The ARI was considered to be an estimate of the action potential duration (APD) and the refractory period [16]. It was defined as an interval between the greatest down slope of the QRS complex and the following greatest upslope of the T wave on a unipolar electrogram (Fig. 5b).
Restitution Properties
The restitution curve of every mapping electrode was created using an exponential function by ARI = a + b × e-DI/c [17, 18]. The diastolic interval (DI) is defined as the difference between the PCL and the last ARI of the paced beat, and a, b, c are model constants that are fitted by a least-square procedure that halts when the difference in the calculated ARI between the two final iterations converges to <10−8. Herein, only the restitution curves with a square of correlation coefficient (R2) >0.8 were used for analysis. The restitution curve slopes were calculated as the first derivatives of the exponential function with each DI, and the maximum slope was identified.
VF Induction
VF was induced either during the restitution pacing protocol described above. Or, if the VF was not induced twice during the pacing protocol, a 30-Hz frequency stimulation delivered from the same electrode was used for VF induction.
VF Activation Rate and VF Cycle Length (VF-CL)
The VF activation rate was calculated by a fast Fourier transform (FFT) analysis by a 2-s trace of VF recordings at each electrode. The highest frequency between 2 and 20 Hz was considered as the activation rate. The VF-CL was estimated as the reciprocal of the VF activation rate.
DFT Determination
After VF induction for 20 s, an electric shock with a biphasic form (6/4 ms) was given (Teletronic Pacing Systems, 4510 Implant Support Device, Teletronics Pty Limited, Homebush, NSW, Australia). The energy leading phase of the shock was initiated at 10 J. Depending on the results of defibrillation, the energy was decreased or increased by steps of 2 J. Failure-to-success or success-to-failure transition energy output was recorded as the first data point. An up-down algorithm was used for three reversals of success-to-failure or failure-to-success. The DFT was calculated by averaging the four shock energies that formed the three reversals [19]. After that, a minimum of 5 min rest was provided after each defibrillation to allow the hemodynamic status to return to normal.
Spatial Heterogeneity
The spatial heterogeneity (dispersion) of the mapped epicardium was evaluated for the following electrophysiological parameters: ARI, the maximal slope of the ARI restitution curve and the VF activation rate. The epicardial dispersion of the activation rate was quantified using the coefficient of variation (CoV, the standard deviation [SD] divided by the mean) from all unipolar electrodes. Transmural dispersion was defined as the difference between the maximum and minimum values of the six unipolar recording sites of the plunge needle.
Drug Administration
In the ibutilide group, after the parameters were measured at HF baseline, the animals received a loading dose of ibutilide (10 μg/kg) intravenously over 10 min. After the initial loading dose, a maintenance infusion of 0.1 mg/kg/h ibutilide was started and maintained until the end of the experiment. The amiodarone group was initially administered with a loading dose (10 mg/kg) intravenously over at least 10 min based on the previous studies [19, 20], followed by a maintenance infusion of 1 mg/kg/h till the end of the experiment.
Statistical Analysis
All results are expressed as means ± SD. The variables were first tested for distribution normality. All quantitative variables were compared using paired t-test for independent variables before and after drug administration. The differences between qualitative variables were analyzed by chi-square test. For all analyses, P < 0.05 was considered to be statistically significant. SPSS 16.0 package (SPSS Inc., Chicago, IL, USA) was used for data analysis.
Results
Echocardiography
After rapid pacing for 4 weeks, the LVEF in all canines showed a significant decrease in both ibutilide (59 ± 7% vs. 26 ± 10%, P < 0.0001) and amiodarone groups (62 ± 5% vs. 28 ± 11%, P < 0.0001) when compared to the baseline, respectively. This was accompanied by a significant increase in the LVEDD (38.4 ± 9.8 mm vs. 68.6 ± 15.6 mm, P < 0.01; 42.8 ± 10 mm vs. 71.3 ± 18.5 mm, P < 0.01, respectively). Thus, the HF model was considered to be successfully established. No significant differences were detected between the two groups in LVEF and LVEDD.
Hemodynamic Effects during Sinus Rhythm
The amiodarone group showed a decline in the BP at different levels during administration of loading dose and subsequent drug maintenance doses, and some dogs even needed an extended loading dose administration time to stabilize their BP. In the ibutilide group, no significant fluctuation of BP was observed throughout the experiment. Compared to HF baseline, the MAP (92 ± 6.1 mmHg vs. 52 ± 11.6 mmHg, P < 0.05) and the SBP dP/dTmax (1.6 ± 0.1 vs. 0.6 ± 0.1, P < 0.01) were significantly decreased after amiodarone administration. Nevertheless, no significant changes were observed on MAP (91 ± 15 mmHg vs. 92 ± 17 mmHg, P = 0.78) and SBP dP/dTmax (1.6 ± 0.1 vs. 1.5 ± 0.3, P = 0.52) after ibutilide application (Fig. 1). Therefore, it was suggested that amiodarone significantly impaired the hemodynamic performance, while ibutilide did not exert similar effect during sinus rhythm.
Effect of ibutilide and amiodarone on hemodynamics before and after drug treatment in pre-VF and post-DF stages. (a) After drug administration, MAP was significantly reduced by amiodarone. (b) Before drug treatment, the SBP dP/dTmax was markedly increased immediately post-DF in both groups. After drug administration, amiodarone has significantly reduced the SBP dP/dTmax in both pre-VF and post-DF stage, suggesting a significant decrease in myocardial contractility. However, ibutilide did not affect the hemodynamic performance when compared to the pre-drug condition. B pre-VF: pre-ventricular fibrillation at baseline. B post-DF: immediate post-defibrillation at baseline. D pre-VF: pre-ventricular fibrillation after drug administration. D post-DF: immediate post-defibrillation after drug administration
Hemodynamic Effects before and after Defibrillation
Amiodarone treatment significantly reduced the SBP dP/dTmax in both pre-VF and post-defibrillation stages (1.6 ± 0.1 vs. 0.6 ± 0.1, P < 0.01; 3.5 ± 0.2 vs. 1.3 ± 0.2, P < 0.01, respectively), suggesting a significant decrease of myocardial contractility. Additionally, majority of the animals required a prolonged period to stabilize the hemodynamics to become normal for sequential experiments after defibrillation. Conversely, no significant changes were detected in the SBP dP/dTmax in both pre-VF and post-defibrillation stages before and after ibutilide application (1.6 ± 0.1 vs. 1.5 ± 0.3, P > 0.05; 3.2 ± 1.3 vs. 3.1 ± 0.8, P > 0.05, respectively), (Fig. 1).
Effects of Two Drugs on HR, QTc, and the Amplitude of QRS
Both drugs showed no evidence of proarrhythmia, such as torsades de pointes (TdP). The most common ECG changes caused by both drugs included slowing of HR and prolongation of QTc. Compared to HF baseline, ibutilide significantly slowed down the HR (145 ± 10 bpm vs. 106 ± 8 bpm, P < 0.01) and prolonged the QTc (285 ± 10 ms vs. 368 ± 11 ms, P < 0.01) 30 min after loading dose administration. Amiodarone treatment significantly reduced the HR (126 ± 32 bpm vs. 107 ± 34 bpm, P < 0.05) and significantly prolonged the QTc (359 ± 40 ms vs. 389 ± 24 ms, P < 0.05), (Table 1). The prolongation of QTc was more pronounced after ibutilide treatment when compared to amiodarone. Compared to the pre-drug condition, amiodarone significantly reduced the QRS amplitude before VF, during VF, and post defibrillation. In contrast, compared to HF baseline, no significant alterations were detected on the amplitude of QRS before VF, during VF, or after defibrillation in the ibutilide group (Fig. 2).
Effect of ibutilide and amiodarone on the amplitude of QRS in different stages. In the left panel, no significant changes were observed on the amplitude of QRS on leads I, II, and aVF before, during VF, or after defibrillation in the ibutilide group when compared to the pre-drug condition. However, the right lane showed that amiodarone has significantly reduced the QRS amplitude before, during VF, and post-DF when compared to the HF baseline. Amio: amiodarone; Ibuti: ibutilide
Effects of Ibutilide and Amiodarone on the DFT and VF Maintenance
Compared to HF baseline, ibutilide treatment has significantly decreased the DFT by 28% (Fig. 3, Table 1). Additionally, VF activation after drug administration was transformed into a more organized pattern (Fig. 4a and b). Four episodes of VF were terminated spontaneously and were restored to sinus rhythm, and the duration of VF was 4.7 ± 1.3 s after induction (Fig. 4c). On the other hand, in the amiodarone group, neither the DFT was significantly altered (Fig. 3, Table 1), nor the VF activation pattern was changed or terminated spontaneously.
Effect of ibutilide and amiodarone on DFT and VERP. The left vertical coordinates represent DFT (black and white histogram), and the right represents VERP (black solid line). Ibutilide reduced the DFT and prolonged the VERP more significantly when compared to the HF at baseline, while amiodarone did not alter the DFT. Moreover, the prolongation of VERP was more pronounced by ibutilide (178–208 ms) as compared to amiodarone (185–202 ms)
Snapshots of VF activation on an epicardial plaque before and after ibutilide administration The VF activation of 144-electrode recording channels on epicardial mapping plaque is presented. (a) VF activated in a chaotic pattern, in which highly unpredictable and disorganized activation sequences were observed before ibutilide administration. (b) Chaotic pattern was observed during initial VF, but the regular pattern emerged as VF progressed after drug administration, and was characterized by highly organized simultaneous activations when compared to the baseline. (c) VF electrically induced by 50 Hz high-frequency stimulation lasted for 4.2 s, which was activated in an organized pattern, spontaneously terminated, and then restored to sinus rhythm after ibutilide administration
Effects of Ibutilide and Amiodarone on VERP, ARI, and Dispersion of Refractoriness
Compared to HF baseline, both ibutilide and amiodarone treatment has significantly prolonged the VERP by 17% and 9%, respectively (Fig. 3, Table 1). Also, both drugs significantly prolonged the ARI and reduced the epicardial dispersion of refractoriness as estimated from the CoV throughout the mapping plaque (Table 1). However, the transmural dispersion of refractoriness remained unaltered as compared to HF baseline, which was estimated from the ARI recorded with the plunge needle (Table 1).
Effects of Ibutilide and Amiodarone on Restitution Properties
The maximal slopes of the restitution curves of all animals were > 1 at HF baseline. Ibutilide and amiodarone treatments have significantly flattened the restitution curves, and the maximal slopes of all restitution curves were < 1 after drug administration. The mean maximal slope of the ARI restitution curve was significantly reduced by 51% after ibutilide administration (Fig. 5a, Table 1) and by 43% (Table 1) after amiodarone administration. Additionally, both drugs reduced the epicardial dispersion of the maximal slope of the ARI restitution curve as compared to HF baseline (Table 1).
ARI measurements and effect of ibutilide on restitution properties (a) Measurements of ARI and DI. (b) The two restitution curves were obtained from one animal for the same electrode in the HF baseline (solid square) and after ibutilide (solid triangle). The maximal slope of the restitution curve for this animal was 1.40 (before drug). Ibutilide flattened the restitution curve significantly, and the maximal slope of restitution curve was 0.69 (after drug administration)
Effects of Ibutilide and Amiodarone on Transmural Dispersion of the VF Activation Rate
Compared to HF baseline, ibutilide and amiodarone administration significantly reduced the VF activation rate by 18% and 12% and increased the VF-CL by 21% and 19%, respectively (Table 1). In addition, administration of ibutilide and amiodarone demonstrated a significant reduction of the transmural dispersion of the VF activation rate (Table 1).
Discussion
The major findings of the present study are as follows: (1) after ibutilide administration, the DFT was markedly reduced when compared to HF baseline. Also, the VF activation pattern has been more organized and could be terminated spontaneously. Furthermore, there are no adverse hemodynamic effects observed throughout the experiment. However, amiodarone did not alter the DFT, while the MAP, SBP dP/dTmax, and the amplitude of QRS were reduced significantly before and after defibrillation, indicating its impairment on the hemodynamic status and myocardial contractility. (2) ibutilide and amiodarone have significantly prolonged the VERP and ARI and decreased the maximum slope of the ventricular ARI restitution curve as well as its dispersion. and (3) both drugs have significantly ameliorated the dispersion of ventricular refractoriness and reduced the transmural dispersion of the VF activation rate.
Electrophysiological Modification and Defibrillation Efficacy
In our previous study, ibutilide was administered to normal dogs and it significantly decreased the DFT by reducing the complex activation during VF [11]. In this study, we demonstrated that the VERP, ARI, and the dispersion of refractoriness in failing hearts showed significant prolongation when compared to those in the normal hearts. The VF threshold (VFT) was markedly decreased, and the DFT was much higher than that in healthy animals. Taken together, these data indicated a significant increase in the susceptibility to VF among canines with HF. To date, only few studies have focused on the effects of ibutilide on ventricular electrophysiological properties in HF animal models, and so this study was conducted. Ibutilide administration to HF canines revealed similar antifibrillatory effects as in the normal hearts and did not affect the hemodynamic parameters. Additionally, the VF activation rate was reduced in failed hearts when compared to normal hearts, and this phenomenon was further decreased by ibutilide administration with further prolonged VF-CL. These electrophysiological parameters are vital indicators of organized activation pattern of VF, thus facilitating defibrillation.
It has been reported that prolongation of APD and VERP is a primary determinant of drug-induced effects on the efficacy of electrical shock [21]. Amiodarone and ibutilide (class III antiarrhythmic agents) prolonged the repolarization period by blocking the outward Ikr channels. In the present study, VERP and ARI were significantly extended after drug administration. Furthermore, the prolongation of QTc and VERP were more pronounced after ibutilide administration when compared to that of amiodarone administration (Fig. 3). As reentry has been generally agreed to be the primary mechanism for the short-duration VF, and the prolonged refractory period might increase the propagating wavelength, thereby VF maintaining is less likely [22]. In the current study, DFT was shown to be markedly decreased by ibutilide but not amiodarone, as compared to that in HF baseline. In addition, spontaneous restoration to sinus rhythm during VF after ibutilide treatment was observed. Similar beneficial effects of decreased DFT by ibutilide were reported for previously. However, previous studies have demonstrated that amiodarone could increase, cause no change or even decreasing the DFT [19, 20, 23, 24]. Accumulating evidence suggests that ibutilide has markedly enhanced the defibrillation efficacy via plateau sodium current activation and substantially promoted drug-induced spontaneous defibrillation in a canine model [7, 25, 26]. Therefore, we speculated that the marked effect of terminating VF after ibutilide administration was partially due to the additional ability to activate the slow sodium current, leading to the extension of VERP and QTc, and facilitating defibrillation when compared to amiodarone.
According to the nonuniform dispersion of the refractoriness hypothesis, increased dispersion of ventricular repolarization and spatiotemporal heterogeneity might be associated with impaired defibrillation efficacy [27]. Makikallio et al. [28] have revealed that episodes of VF that were spontaneously restored to sinus rhythm, displayed organized local activation dynamics than sustained VF that is terminated only by electric shocks. In the present study, the epicardial dispersion of ARI at different PCLs and the ARI restitution slope were remarkably decreased after the ibutilide application. In addition, the transmural dispersion of VF activation rate was also decreased by the drug, leading to a more organized VF activation pattern. The VF organization hypothesis [21] indicated that an organized fibrillation pattern results in facilitated defibrillation. Therefore, pharmacologically attenuation of the spatiotemporal heterogeneity of the refractoriness promotes VF organization, achieving spontaneous termination of VF and lowering the DFT.
The APD restitution hypothesis stated that a steep curve of APD restitution leads to dynamic instability and a flattened restitution curve prevents wave break-up, thereby promoting VF conversion into an organized activation pattern such as monomorphic VT [29]. Our previous study has shown that drugs, such as verapamil and sotalol, showed antifibrillatory effects in vitro, by flattening the restitution relation and suppressing the APD alternans [30, 31]. A major finding of this study was that ibutilide led to a flattened ARI restitution curve with a slope of 1.40–0.69, which improved the defibrillation efficacy and reduced the VF activation pattern complexity.
Hemodynamic Effects and Defibrillation Efficacy
In the current study, the hypotensive response to amiodarone has occurred before defibrillation, as well as immediately after defibrillation, and this was consistent with the findings of previous studies [32, 33], whereas ibutilide showed no impairment on the hemodynamic status throughout the current experiment.
The ventricular chamber was in an overloaded state due to ineffective ejection after induction of VF for 20 s before defibrillation. Therefore, the SBP dP/dTmax immediately after defibrillation should be significantly improved when compared to the pre-defibrillation stage before as well as after drug administration. In the current study, before drug treatment, the SBP dP/dTmax showed marked increase immediately after defibrillation in both groups, while the MAP remained the same. However, after drug administration, amiodarone has significantly reduced the MAP and reduced the SBP dP/dTmax in both pre-VF and post-defibrillation stages (Fig. 1), while ibutilide did not affect the hemodynamic performance when compared to the pre-drug condition. Furthermore, amiodarone also significantly reduced the maximum amplitude of QRS during VF and after defibrillation. Another study showed that the diffused low voltage in the presence of decreased QRS amplitude on the surface ECG is associated with left ventricular dysfunction, which resulted from reduced ventricular contractility [34, 35]. Therefore, decreased amplitude of QRS was considered as depression of myocardial contractility when compared to HF baseline (Fig. 2). Furthermore, acute global ischemia caused a significant increase in the width of the vulnerable window. Due to these marked changes, the upper limit of vulnerability and DFT might be affected by acute myocardial ischemia [36]. In this study, severe hypotension after amiodarone application might lead to a decrease in the coronary perfusion pressure, thereby causing myocardial ischemia. This phenomenon might be partially associated with the finding that amiodarone did not alter the DFT.
In contrast, ibutilide did not significantly affect the hemodynamic performance before and after defibrillation, as well as the amplitude of the QRS complex, indicating it did not exhibit negative inotropic effect. Previous evidence demonstrated that ibutilide did not exert any significant effect on the conduction velocity nor on the hemodynamic parameters in a series of experimental animal studies [25, 37,38,39]. Hence, we postulated that the reduced myocardial perfusion pressure caused by hypotension might impair the defibrillation efficacy in amiodarone canines.
Clinical Implications
Several antiarrhythmic agents might decrease myocardial contractility, compromise hemodynamic performance, and limit their use in patients with VAs, especially for those patients with impaired ventricular function when administered at effective doses intravenously. Hitherto, amiodarone has been proven to be an effective drug in reducing VAs in patients with structural heart disease. However, in clinical settings, intravenous administration of amiodarone can cause hypotension due to vasodilation and decreased myocardial contractility, thereby endangering the patients with damaged cardiac function. Conversely, ibutilide, a selective class III antiarrhythmic agent, provided similar quasi-effects, but without any impairments to the hemodynamic performance. Accumulating evidence showed that pharmacokinetics of ibutilide remains unaltered in patients with LV systolic dysfunction [40]. However, ibutilide administration is associated with a 2–3-fold increased risk of TdP in patients with HF. Both amiodarone and ibutilide showed this side-effect, especially in circumstance of electrolyte disturbances which are frequently observed in HF condition. Overall, the prevalence of such proarrhythmic event might be one of the reasons for the lack of spontaneous TdP in current study. Ibutilide not only significantly reduced the DFT but also led to VF activation organization and promoted the spontaneous termination of VF in this study. More importantly, no adverse hemodynamic effects were observed, while amiodarone significantly impaired the hemodynamic performance. Taken together, it could be deduced that ibutilide is a treatment option for resuscitation in patients with HF in clinical practice, especially for hemodynamically unstable patients with VAs.
Study Limitations
Firstly, we mapped only the regional LV epicardium rather than performing a global biventricular mapping. Hence, the activation patterns during VF might not be thorough. Secondly, only the effects of ibutilide at a fixed dosage were investigated, which yielded a high plasma concentration that altered the cardiac electrophysiological properties. However, the action of antiarrhythmic agents is usually concentration-dependent. Therefore, it is essential to explore different drug concentrations to evaluate the effects of ibutilide on DFT and VF activation patterns dynamically in the future studies. Thirdly, the SBP dP/dTmax was used to assess the cardiac systolic function in the present study. Real-time cardiac ultrasound assessment and/or cardiac catheter to obtain hemodynamic variables, such as pulmonary capillary wedge pressure and cardiac output, should be used to reflect a more detailed myocardial contractility function. However, several previous studies have used the SBP dP/dTmax to evaluate myocardial contractility, and we speculated that the current data could assess the true state of cardiac contractility. Finally, the amiodarone dose used in the present study is parallel to that used in the previous VF study, but the dose is higher than the usual clinical usage. Therefore, the hemodynamic changes by amiodarone are partially caused due to high dose.
Conclusions
Intravenous ibutilide has significantly reduced the DFT and promoted the VF activation pattern organization without affecting the hemodynamics and cardiac contractility. These findings indicated that ibutilide with antifibrillatory properties of VF alteration, might be an option for adjunctive drug therapy for resuscitation in the clinical management of HF in the future. Yet, intravenous amiodarone administration showed prominent negative effects on the hemodynamic status and myocardial contractility before and after defibrillation and failed to alter the DFT.
References
Ferreira-Gonzalez I, Dos-Subira L, Guyatt GH. Adjunctive antiarrhythmic drug therapy in patients with implantable cardioverter defibrillators: a systematic review. Eur Heart J. 2007;28(4):469–77.
Lorvidhaya P, Addo K, Chodosh A, Iyer V, Lum J, Buxton AE. Sudden cardiac death risk stratification in patients with heart failure. Heart Fail Clin. 2011;7(2):157–74 vii.
Weeks PA, Sieg A, Gass JA, Rajapreyar I. The role of pharmacotherapy in the prevention of sudden cardiac death in patients with heart failure. Heart Fail Rev. 2016;21(4):415–31.
Kosinski EJ, Albin JB, Young E, Lewis SM, LeLand OS Jr. Hemodynamic effects of intravenous amiodarone. J Am Coll Cardiol. 1984;4(3):565–70.
Munoz A, Karila P, Gallay P, et al. A randomized hemodynamic comparison of intravenous amiodarone with and without tween 80. Eur Heart J. 1988;9(2):142–8.
Friedrichs GS, Chi L, Black SC, Manley PJ, Oh JY, Lucchesi BR. Antifibrillatory effects of ibutilide in the rabbit isolated heart: mediation via ATP-dependent potassium channels. J Pharmacol Exp Ther. 1993;266(3):1348–54.
Wesley RC Jr, Farkhani F, Morgan D, Zimmerman D. Ibutilide: enhanced defibrillation via plateau sodium current activation. Am J Phys. 1993;264(4 Pt 2):H1269–74.
Wood MA, Stambler BS, Ellenbogen KA, et al. Suppression of inducible ventricular tachycardia by ibutilide in patients with coronary artery disease. Ibutilide Investigators. Am Heart J. 1998;135(6 Pt 1):1048–54.
Labhasetwar V, Underwood T, Heil RW Jr, Gallagher M, Langberg J, Levy RJ. Epicardial administration of ibutilide from polyurethane matrices: effects on defibrillation threshold and electrophysiologic parameters. J Cardiovasc Pharmacol. 1994;24(5):826–40.
Sendra-Ferrer M, Gonzalez MD. Ibutilide for the control of refractory ventricular tachycardia and ventricular fibrillation in patients with myocardial ischemia and hemodynamic instability. J Cardiovasc Electrophysiol. 2019;30(4):503–10.
Jin Q, Zhou J, Zhang N, et al. Ibutilide decreases defibrillation threshold by the reduction of activation pattern complexity during ventricular fibrillation in canine hearts. Chin Med J. 2012;125(15):2701–7.
Stambler BS, Beckman KJ, Kadish AH, et al. Acute hemodynamic effects of intravenous ibutilide in patients with or without reduced left ventricular function. Am J Cardiol. 1997;80(4):458–63.
Jin Q, Zhou J, Zhang N, et al. Defibrillation threshold varies during different stages of ventricular fibrillation in canine hearts. Heart Lung Circ. 2013;22(2):133–40.
Mahajan A, Shiferaw Y, Sato D, et al. A rabbit ventricular action potential model replicating cardiac dynamics at rapid heart rates. Biophys J. 2008;94(2):392–410.
Koller ML, Riccio ML, Gilmour RF Jr. Dynamic restitution of action potential duration during electrical alternans and ventricular fibrillation. Am J Phys. 1998;275(5 Pt 2):H1635–42.
Dhein S, Muller A, Gerwin R, Klaus W. Comparative study on the proarrhythmic effects of some antiarrhythmic agents. Circulation. 1993;87(2):617–30.
Banville I, Gray RA. Effect of action potential duration and conduction velocity restitution and their spatial dispersion on alternans and the stability of arrhythmias. J Cardiovasc Electrophysiol. 2002;13(11):1141–9.
Watanabe MA, Koller ML. Mathematical analysis of dynamics of cardiac memory and accommodation: theory and experiment. Am J Physiol Heart Circ Physiol. 2002;282(4):H1534–47.
Huang J, Skinner JL, Rogers JM, Smith WM, Holman WL, Ideker RE. The effects of acute and chronic amiodarone on activation patterns and defibrillation threshold during ventricular fibrillation in dogs. J Am Coll Cardiol. 2002;40(2):375–83.
Fain ES, Lee JT, Winkle RA. Effects of acute intravenous and chronic oral amiodarone on defibrillation energy requirements. Am Heart J. 114(1 Pt 1):8–17.
Jacob S, Pidlaoan V, Singh J, Bharadwaj A, Patel MB, Carrillo A. High defibrillation threshold: the science, signs and solutions. Ind Pacing Electrophysiol J. 2010;10(1):21–39.
Tabereaux PB, Dosdall DJ, Ideker RE. Mechanisms of VF maintenance: wandering wavelets, mother rotors, or foci. Heart Rhythm. 2009;6(3):405–15.
Behrens S, Li C, Franz MR. Effects of long-term amiodarone treatment on ventricular-fibrillation vulnerability and defibrillation efficacy in response to monophasic and biphasic shocks. J Cardiovasc Pharmacol. 1997;30(4):412–8.
Zhou L, Chen BP, Kluger J, Fan C, Chow MS. Effects of amiodarone and its active metabolite desethylamiodarone on the ventricular defibrillation threshold. J Am Coll Cardiol. 1998;31(7):1672–8.
Lee KS. Ibutilide, a new compound with potent class III antiarrhythmic activity, activates a slow inward Na+ current in Guinea pig ventricular cells. J Pharmacol Exp Ther. 1992;262(1):99–108.
Reiffel JA, Blitzer M. The actions of ibutilide and class Ic drugs on the slow sodium channel: new insights regarding individual pharmacologic effects elucidated through combination therapies. J Cardiovasc Pharmacol Ther. 2000;5(3):177–81.
Nash MP, Mourad A, Clayton RH, et al. Evidence for multiple mechanisms in human ventricular fibrillation. Circulation. 2006;114(6):536–42.
Makikallio TH, Huikuri HV, Myerburg RJ, et al. Differences in the activation patterns between sustained and self-terminating episodes of human ventricular fibrillation. Ann Med. 2002;34(2):130–5.
Wu TJ, Lin SF, Baher A, et al. Mother rotors and the mechanisms of D600-induced type 2 ventricular fibrillation. Circulation. 2004;110(15):2110–8.
Jin Q, Chen X, Smith WM, Ideker RE, Huang J. Effects of procainamide and Sotalol on restitution properties, dispersion of refractoriness, and ventricular fibrillation activation patterns in pigs. J Cardiovasc Electrophysiol. 2008;19(10):1090–7.
Jin Q, Dosdall DJ, Li L, Rogers JM, Ideker RE, Huang J. Verapamil reduces incidence of reentry during ventricular fibrillation in pigs. Am J Physiol Heart Circ Physiol. 2014;307(9):H1361–9.
Cushing DJ, Cooper WD, Gralinski MR, Lipicky RJ. The hypotensive effect of intravenous amiodarone is sustained throughout the maintenance infusion period. Clin Exp Pharmacol Physiol. 2010;37(3):358–61.
Doshi D, Jayawardana R. Amiodarone-induced life-threatening refractory hypotension. Am J Case Rep. 2015;16:617–20.
Goldberger AL. A specific ECG triad associated with congestive heart failure. Pacing Clin Electrophysiol. 1982;5(4):593–9.
Chinitz JS, Cooper JM, Verdino RJ. Electrocardiogram voltage discordance: interpretation of low QRS voltage only in the limb leads. J Electrocardiol. 2008;41(4):281–6.
Behrens S, Li C, Franz MR. Effects of myocardial ischemia on ventricular fibrillation inducibility and defibrillation efficacy. J Am Coll Cardiol. 1997;29(4):817–24.
Cimini MG, Brunden MN, Gibson JK. Effects of ibutilide fumarate, a novel antiarrhythmic agent, and its enantiomers on isolated rabbit myocardium. Eur J Pharmacol. 1992;222(1):93–8.
Hester JB, Gibson JK, Cimini MG, et al. N-[(omega-amino-1-hydroxyalkyl)phenyl]methanesulfonamide derivatives with class III antiarrhythmic activity. J Med Chem. 1991;34(1):308–15.
Nabih MA, Prcevski P, Fromm BS, et al. Effect of ibutilide, a new class III agent, on sustained atrial fibrillation in a canine model of acute ischemia and myocardial dysfunction induced by microembolization. Pacing Clin Electrophysiol. 1993;16(10):1975–83.
Tisdale JE, Overholser BR, Sowinski KM, et al. Pharmacokinetics of ibutilide in patients with heart failure due to left ventricular systolic dysfunction. Pharmacotherapy. 2008;28(12):1461–70.
Funding
This study was funded by grants from the National Natural Science Foundation of China (No. 81600270) and the Shanghai Science and Technology Committee (No. 16140904602).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests.
Ethical Approval
All animals were acquired from the Shanghai Jiao Tong University Agriculture College (China) and raised under controlled conditions at the Department of Animals for Scientific Research, Shanghai Jiao Tong University School of Medicine. All the study procedures were approved by the Shanghai Jiao Tong University School of Medicine Animal Care and Use Committee in accordance with the recommendations from the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health (eighth edition, 2011).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, N., Luo, Q., Jin, Q. et al. Ibutilide Reduces Ventricular Defibrillation Threshold and Organizes Ventricular Fibrillation Activation in Canine Heart Failure Model. Cardiovasc Drugs Ther 34, 323–334 (2020). https://doi.org/10.1007/s10557-020-06958-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-020-06958-2