Abstract
Obstructive sleep apnea (OSA) is associated with the progression of cardiovascular disease (CVD), particularly in the middle-aged population. However, the clinical importance of OSA as a risk for CVD in the elderly population remains controversial. Moreover, evidence for the effectiveness of continuous positive airway pressure (CPAP) treatment for the secondary prevention of CVD in elderly patients is lacking. We assessed whether CPAP treatment improves cardiovascular outcomes in elderly patients with OSA and CVD. In this retrospective cohort study, we enrolled 130 elderly patients aged 65–86 years with moderate to severe OSA (apnea–hypopnea index ≥15/h) and a history of hospitalization due to CVD, who underwent polysomnography between November 2004 and July 2011. Patients were divided into the CPAP group (n = 64) or untreated OSA group (n = 66). The main outcome measures were cardiovascular death and hospitalization due to CVD. During the mean follow-up period of 32.9 ± 23.8 (standard deviation) months, 28 (21.5 %) patients either died or were hospitalized. The Kaplan–Meier curves indicated that event-free survival was significantly lower in the untreated OSA group than in the CPAP group (P < 0.005). A multivariate analysis showed that the risk was significantly increased in the untreated OSA group (hazard ratio 5.13; 95 % confidence interval 1.01–42.0; P < 0.05). Moderate to severe OSA not treated with CPAP was an independent risk factor for relapse of a CVD event, and adequate CPAP treatment improved cardiovascular outcomes in elderly patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a highly prevalent disorder in the general population, characterized by repetitive upper airway obstruction during sleep [1]. The Sleep Heart Health Study showed that the prevalence of moderate to severe sleep-disordered breathing (SDB) was estimated at 10 % in persons aged 40–49 years, and 20–21 % in persons aged ≥70 years [1]. A previous study has shown that the prevalence of sleep apnea tends to increase with age, although its severity decreases [2]. OSA has been widely recognized to promote the progression of cardiovascular disease (CVD), mostly among middle-aged populations [3–20]. On the other hand, some authors observed that SDB among elderly patients was not an independent risk factor for hypertension [21] or mortality [22–26] in aged cohorts, and that age [23, 26] and burden of illness [24, 26] were independent risk factors for mortality. Thus it is commonly known that the prevalence of SDB among elderly persons is also high, but OSA among them differs from that of the middle-aged in some ways [27].
Takama and Kurabayashi [28] reported that the presence of OSA was a strong predictor of fatal cardiovascular events in patients with CVD. The subjects studied in their report were markedly older than those of previously published reports, with a mean age of approximately 70 years. Among patients with CVD, OSA appears to promote poor cardiovascular outcomes in the elderly population. Recently, Martinez-Garcia et al. [29] reported that untreated, severe OSA in elderly patients was associated with an approximately twofold increase in cardiovascular mortality compared with elderly patients without OSA.
In recent years, aging of the population has become one of the most serious problems worldwide, and the secondary prevention of CVD in such a high-risk elderly population is an urgent subject. In middle-aged populations, continuous positive airway pressure (CPAP) treatment is reported to improve cardiovascular outcomes in patients with OSA and CVD [4–6, 16, 30–32]. However, whether CPAP treatment for elderly patients with CVD contributes to a decrease in new cardiovascular events remains unclear. Furthermore, a therapeutic strategy for OSA in this patient population has not yet been established. Therefore, we conducted this study to assess whether CPAP improves cardiovascular outcomes in elderly patients with OSA and CVD.
Patients and methods
Patients
A total of 1,693 patients underwent a fully attended polysomnography at Tokyo Medical University Hospital between November 2004 and July 2011. From this database, we retrospectively selected consecutive elderly patients aged ≥65 years with moderate to severe SDB who had a history of hospitalization due to CVD before polysomnography, and classified them into two groups: a CPAP group and an untreated OSA group. CVD included the following: heart failure; coronary artery disease, such as myocardial infarction and angina pectoris; atrial or ventricular tachyarrhythmia, such as atrial fibrillation/flutter and ventricular tachycardia/fibrillation; ischemic and hemorrhagic stroke; and aortic dissection. Exclusion criteria included patients with central sleep apnea (>50 % apneic events), cancer, chronic kidney disease on hemodialysis, and previous positive airway pressure (PAP) treatment.
Ethical considerations
The present study was conducted in accordance with the recommendations of the Declaration of Helsinki (1975), and the protocol was approved by the ethical review board of Tokyo Medical University. Written informed consent was obtained from all patients to make use of their medical records.
Sleep study and PAP treatment
SDB was diagnosed in all patients based on the results of overnight polysomnography using a digital polygraph (Alice 4 and 5; Philips Respironics, Murrysville, PA, USA) in our sleep laboratory. Sleep stages and arousals were scored according to standard criteria [33, 34]. Thoracoabdominal movements were monitored by respiratory inductance plethysmography, and oxyhemoglobin saturation was monitored by oximetry. Signals were recorded on a polysomnographic system. Obstructive and central apneas and hypopneas were scored as previously described [35]. The number of apneas and hypopneas per hour of sleep (apnea–hypopnea index (AHI)) was calculated. Moderate to severe SDB was defined as AHI ≥15/h. We defined patients with predominantly central sleep apnea as having an AHI of ≥15/h, of which >50 % were central events. These patients were excluded from further analysis.
Patients with moderate to severe OSA were recommended for CPAP treatment, regardless of their symptoms. All patients who were treated with CPAP had been titrated manually on the second night in the sleep laboratory with full polysomnography to determine the appropriate pressure level for each patient. Thereafter, CPAP treatment was performed at home. Patients who had refused CPAP treatment initially or discontinued it within the first month after initiation were enrolled in the untreated OSA group. Patients who had been treated with CPAP were entered into the CPAP group, but those who had discontinued CPAP treatment between the first month after initiation of CPAP treatment and the day of outcome measures were excluded from the data analyses, because the association between the effect of CPAP treatment and cardiovascular events was unclear. Adherence to CPAP was assessed by reading the time counter on the device.
Outcome measures
The major outcome measures of interest were cardiovascular death or rehospitalization due to heart failure, acute coronary syndrome, arrhythmias, stroke, and aortic dissection between the day of the baseline polysomnography and September 2011. The medical records were reviewed by two investigators. Each event was defined as follows: heart failure was defined as decompensated heart failure, based on the Framingham criteria accompanied by a worsening of clinical signs and symptoms of heart failure; acute coronary syndrome included acute myocardial infarction, regardless of ST-segment elevation, and unstable angina pectoris; arrhythmias included ventricular tachycardia, atrial flutter, and atrial fibrillation that required hospitalization because of a hemodynamic emergency; stroke was defined as ischemic or hemorrhagic stroke which required hospitalization; aortic dissection included acute dissection of the thoracic and/or abdominal aorta. We counted only one event per patient, and once the event occurred the patient’s follow-up was concluded.
Statistical analysis
Continuous data are expressed as mean ± standard deviation (SD), and categorical variables are expressed as frequencies of occurrence and percentages. The baseline characteristics were compared using Student’s t test for continuous variables, and the Chi-square test for categorical variables. A two-sided P value of less than 0.05 was considered to indicate a statistically significant difference. Event-free survival between the groups was compared using the Kaplan–Meier estimates with the log-rank test. The hazard ratio (HR) was calculated using the Cox proportional hazards model. Univariate analysis was based on the proportional hazards model to determine the associations between CVD events and the following pretreatment variables: age; gender; body mass index; past history or presence of hypertension, dyslipidemia, or diabetes; presence of atrial fibrillation; systolic/diastolic blood pressure; heart rate; subjective sleepiness expressed according to the Epworth Sleepiness Scale; left ventricular ejection fraction on echocardiograms; plasma brain natriuretic peptide; plasma norepinephrine; estimated glomerular filtration rate; medications; AHI; and study groups. Variables that were regarded as significant were included in the multivariate analysis. All statistical analyses were performed using a statistical software package (JMP 7; SAS Institute, Cary, NC, USA).
Results
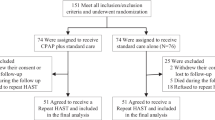
Initially, 146 elderly patients were enrolled in this study; of these, 80 were classified into the CPAP group and 66 into the untreated OSA group. In the CPAP group 16 patients discontinued CPAP treatment, leaving 64 patients for inclusion in the final analyses.
Patients’ characteristics
The baseline characteristics of the patients were comparable between the groups (Table 1). The CPAP group included a significantly larger number of male patients than the untreated OSA group (P = 0.0003). The diastolic blood pressure in the CPAP group was higher than that in the untreated OSA group (P < 0.05). Other variables such as age, body mass index, history of hypertension, dyslipidemia, diabetes, atrial fibrillation, heart rate, systolic blood pressure, hemoglobin, estimated glomerular filtration rate, plasma brain natriuretic peptide, plasma norepinephrine, left ventricular ejection fraction, and use of angiotensin-converting enzyme inhibitors or angiotensin-II receptor blockers, β-blockers, mineralocorticoid receptor antagonists, and statins as medications were not significantly different between the groups. Regarding the previous history of CVD, there was no statistically significant difference between the groups (Table 2).
With respect to the sleep characteristics (Table 3), the CPAP group had a significantly higher AHI, obstructive apnea index, central apnea index, and arousal index (P < 0.0001, P = 0.0002, P < 0.005, and P = 0.0008, respectively). The median value of nightly CPAP usage in the CPAP group was 5.0 ± 1.7 h and the median value of AHI downloaded from CPAP devices was 4.3 ± 3.0/h.
Impact of CPAP treatment on event-free survival
During the mean follow-up period of 32.9 ± 23.8 months, 28 (21.5 %) patients either died or were rehospitalized because of CVD, the frequencies of CVD events being 7 (10.9 %) patients in the CPAP group and 21 (31.8 %) in the untreated OSA group (P < 0.005). The mortality rate was not significantly different between the groups. However, the total rate of rehospitalization due to CVD was significantly higher in the untreated OSA group (P < 0.01). Furthermore, the rate of rehospitalization due to heart failure was significantly higher in the untreated OSA group than in the CPAP group (P < 0.05, Table 4).
The causes of rehospitalization were not in the same category of CVD as that at baseline. Of 17 heart failure events, 15 patients had a previous history of heart failure; the other 2 patients had no history of heart failure although they had a history of coronary artery disease. Of four arrhythmic events, two patients had a previous history of arrhythmia and the other two had no history of arrhythmia, although one had a history of coronary artery disease and the other had an aortic dissection. There was no recurrence of aortic dissection. The first onsets of aortic dissection were seen in one patient with coronary artery disease and one with heart failure. All stroke events were the recurrences of previous strokes.
The Kaplan–Meier event-free survival curves indicated that event-free survival was significantly lower in the untreated OSA group than in the CPAP group (P < 0.005, log-rank test; Fig. 1). Univariate Cox regression analyses revealed that the following were each associated with CVD events: age; female gender; history of hypertension; use of β-blockers and angiotensin-converting enzyme inhibitors or angiotensin-II receptor blockers; low levels of estimated glomerular filtration rate, hemoglobin, and left ventricular ejection fraction; high levels of brain natriuretic peptide; and untreated OSA (Table 5). In the multivariate Cox regression analysis, female gender (HR 4.20; 95 % confidence interval (CI) 1.13–17.5; P < 0.05) and untreated OSA (HR 5.13; 95 % CI 1.01–42.0; P < 0.05) were independent predictors of CVD events.
Discussion
The main finding of this study was that CPAP treatment significantly reduced CVD events, including rehospitalization due to heart failure, acute coronary syndrome, arrhythmia, stroke, and aortic dissection in elderly patients with moderate to severe OSA and CVD. Concurrently, untreated, moderate to severe OSA was independently associated with CVD events in this population sample. Therefore, adequate CPAP treatment could be an effective strategy for the secondary prevention of CVD in elderly patients with CVD and moderate to severe OSA.
According to previously published reports, the clinical significance of OSA in the elderly is inconclusive. In an observational study involving elderly patients, those with sleep apnea (defined as a respiratory disturbance index of 10 events per hour of sleep) had 2.7 times greater mortality than those without it, but this was not statistically significant (95 % CI 0.95–7.47) [23]. Another study showed that elderly individuals (mean age 72.5 years) with a respiratory disturbance index of ≥30 had significantly shorter survival, but the Cox proportional hazards analysis revealed that only age, CVD, and pulmonary disease, but not respiratory disturbance index, were the independent predictors of death [26]. However, some recent reports have shown that severe OSA was a high risk factor for cardiovascular mortality in elderly patients [28, 29]. Kobayashi et al. [27] proposed that there were some clinical differences between middle-aged-onset OSA and elderly-onset OSA among elderly patients with OSA. Compared with the middle-aged-onset group, the elderly-onset group had lower values of arousal index, maximal negative esophageal pressure, adequate nasal CPAP level, and fewer cardiovascular complications. These results indicate that cardiovascular risks are not uniformly associated with OSA in the elderly population. Unfortunately, we were unable to estimate the onset times of OSA, but we assume that large numbers of subjects in our study would have had a high risk for CVD events, because they had a history of hospitalization due to CVD.
Although the clinical significance of OSA was not assessed by comparing elderly patients with and without OSA in this study, we determined that untreated, moderate to severe OSA was significantly associated with reduced cardiovascular event-free survival rate in elderly patients with CVD and OSA not treated with CPAP compared with those treated with CPAP. CPAP treatment appears to inhibit the development of CVD. CPAP directly reduces the intrathoracic negative pressure and reduces venous return. Accordingly, it reduces the intramural pressure, causes lowering of the pulmonary capillary wedge pressure, and increases cardiac output in patients with heart failure [36–38]. Furthermore, CPAP indirectly reduces sympathetic nervous activity [39–42], oxidative stress [43–46], and inflammation [45, 47] by improving SDB. It is thought that the direct and indirect effects of CPAP contribute to the prevention of coronary plaque rupture, thrombotic formation, arrhythmias, and cardiac dysfunction. A significant reduction of rehospitalization for heart failure in the CPAP group has been observed in this study, which may be explained by the fact that the impact of the direct physical effects of CPAP treatment is greater on patients with heart failure than on patients with other CVD. Because this was a retrospective, observational study, it is unlikely that an observer bias affected the event rate of rehospitalization.
Daida et al. [48] reported that the rate of cardiovascular death (fatal myocardial infarction, fatal stroke, and other cardiovascular death) was 2.7 % in 3597 Japanese ACS patients (mean age 67 years old) during a 2-year follow-up. In our study, mortality was extremely low. Lavie and Lavie [49] reported that elderly patients with moderate sleep apnea had lower mortality than the matched population cohorts, and severe sleep apnea had the same mortality as the matched population cohorts. In another report, Lavie et al. [25] stated that the mortality rates in male patients with sleep apnea decreased with age. They proposed that sleep apnea might activate adaptive pathways in the elderly. The mechanism of this protective effect is unclear, but this effect might have affected our mortality data. Further investigation of this topic is warranted.
Concerning heart failure events, more patients had a history of heart failure in the untreated OSA group, although this was not statistically significant. This might have been a source of bias for the high incidence of hospitalization due to heart failure observed in the untreated OSA group. However, in a subgroup analysis of 54 patients who had a history of heart failure, the recurrence rates of heart failure events were 35.5 % (11/31) in the untreated OSA group and 17.4 % (4/23) in the CPAP group. Another two heart failure events were de novo heart failure from coronary artery disease, both in the untreated OSA group. Therefore, taking the high incidence of heart failure in the untreated OSA group into consideration, CPAP treatment may reduce the rates of occurrence and recurrence of heart failure.
Kasai et al. [6] have reported that compliance to CPAP treatment was an important factor affecting prognosis in patients with heart failure and OSA, but there are only a few previous reports that provide clear data regarding CPAP adherence. In our study, adherence to CPAP treatment was considered to be comparatively strong, because the median value of nightly CPAP device usage was 5.0 h. We did not find any obvious effect of CPAP adherence on the event rates in this study.
One recent investigation has revealed that OSA is a risk factor for cardiovascular death not only in men but also in women, and that adequate CPAP treatment reduces mortality [7]. We enrolled 37 elderly women with moderate to severe OSA in our study. Women tended to not receive CPAP. Among the 37 women with moderate to severe OSA, only 9 (24.3 %) belonged to the CPAP group. On the other hand, 55 (59.1 %) of 93 men with moderate to severe OSA belonged to the CPAP group. To date, SDB has been virtually ignored as a cardiovascular risk in women. However, women had a 4.2-fold increase in CVD events compared with men by multivariate analysis. These facts suggest that CPAP treatment for OSA is very important in preventing CVD events in elderly women as well as in elderly men.
This real-world study indicates the importance for clinicians of recognizing and providing appropriate treatment for OSA, particularly in the elderly population. In our study, although CPAP treatment for OSA did not reveal a significant decrease in mortality, it prevented rehospitalization due to CVD events. We propose that CPAP treatment for elderly patients with OSA and CVD would lead to a better quality of life and would also be beneficial from an economic perspective.
The present study had several limitations. First, this was a small, retrospective cohort study. Intervention for OSA was not randomized. Prospective, randomized controlled trials would more strongly support the effectiveness of CPAP treatment for the secondary prevention of CVD in the elderly population. Second, many of the enrolled patients in this study had undergone polysomnography because of suspicion of SDB; therefore, we were unable to enroll a sufficient number of patients without SDB as our controls. Third, because of the small number of cardiovascular deaths, our results ultimately lacked the statistical evidence to more firmly implicate the effects of SDB on mortality in patients with CVD. Fourth, we could not follow the changes in body mass index, diet or exercise practice, and medical therapies during follow-up periods, including the patients’ adherence to the medical therapies. These factors might have biased the final results.
Conclusions
To the best of our knowledge, we have provided the first report that CPAP treatment in elderly patients with OSA and CVD is associated with prevention of future cardiovascular events. We found that CPAP treatment significantly reduced rehospitalization due to CVD, but not cardiovascular death, in elderly patients with OSA and CVD. Although additional research is required, we believe that CPAP treatment promises to be an effective strategy for the secondary prevention of CVD in elderly patients with OSA and CVD.
References
Young T, Shahar E, Nieto FJ, Redline S, Newman AB, Gottlieb DJ, Walsleben JA, Finn L, Enright P, Samet JM, Sleep Heart Health Study Research Group (2002) Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med 162:893–900
Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A (1998) Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med 157:144–148
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea–hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053
Milleron O, Pilliere R, Foucher A, de Roquefeuil F, Aegerter P, Jondeau G, Raffestin BG, Dubourg O (2004) Benefits of obstructive sleep apnoea treatment in coronary artery disease: a long-term follow-up study. Eur Heart J 25:728–734
Cassar A, Morgenthaler TI, Lennon RJ, Rihal CS, Lerman A (2007) Treatment of obstructive sleep apnea is associated with decreased cardiac death after percutaneous coronary intervention. J Am Coll Cardiol 50:1310–1314
Kasai T, Narui K, Dohi T, Yanagisawa N, Ishiwata S, Ohno M, Yamaguchi T, Momomura S (2008) Prognosis of patients with heart failure and obstructive sleep apnea treated with continuous positive airway pressure. Chest 133:690–696
Campos-Rodriguez F, Martinez-Garcia MA, de la Cruz-Moron I, Almeida-Gonzalez C, Catalan-Serra P, Montserrat JM (2012) Cardiovascular mortality in women with obstructive sleep apnea with or without continuous positive airway pressure treatment: a cohort study. Ann Intern Med 156:115–122
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Javier Nieto F, O’Connor GT, Boland LL, Schwartz JE, Samet JM (2001) Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med 163:19–25
Mooe T, Franklin KA, Holmstrom K, Rabben T, Wiklund U (2001) Sleep-disordered breathing and coronary artery disease: long-term prognosis. Am J Respir Crit Care Med 164:1910–1913
Yumino D, Tsurumi Y, Takagi A, Suzuki K, Kasanuki H (2007) Impact of obstructive sleep apnea on clinical and angiographic outcomes following percutaneous coronary intervention in patients with acute coronary syndrome. Am J Cardiol 99:26–30
Wang H, Parker JD, Newton GE, Floras JS, Mak S, Chiu KL, Ruttanaumpawan P, Tomlinson G, Bradley TD (2007) Influence of obstructive sleep apnea on mortality in patients with heart failure. J Am Coll Cardiol 49:1625–1631
Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R, Kirchner HL, Sahadevan J, Redline S (2006) Association of nocturnal arrhythmias with sleep-disordered breathing: The Sleep Heart Health Study. Am J Respir Crit Care Med 173:910–916
Gami AS, Hodge DO, Herges RM, Olson EJ, Nykodym J, Kara T, Somers VK (2007) Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol 49:565–571
Sampol G, Romero O, Salas A, Tovar JL, Lloberes P, Sagales T, Evangelista A (2003) Obstructive sleep apnea and thoracic aorta dissection. Am J Respir Crit Care Med 168:1528–1531
Martinez-Garcia MA, Campos-Rodriguez F, Soler-Cataluna JJ, Catalan-Serra P, Roman-Sanchez P, Montserrat JM (2012) Increased incidence of nonfatal cardiovascular events in stroke patients with sleep apnoea: effect of CPAP treatment. Eur Respir J 39:906–912
Varol E, Akcay S, Ozaydin M, Ozturk O, Cerci SS, Sahin U (2010) Influence of obstructive sleep apnea on left ventricular mass and global function: sleep apnea and myocardial performance index. Heart Vessels 25:400–404
Naito R, Sakakura K, Kasai T, Dohi T, Wada H, Sugawara Y, Kubo N, Yamashita S, Narui K, Ishiwata S, Ohno M, Ako J, Momomura S (2012) Aortic dissection is associated with intermittent hypoxia and re-oxygenation. Heart Vessels 27:265–270
Saruhara H, Takata Y, Usui Y, Shiina K, Hashimura Y, Kato K, Asano K, Kawaguchi S, Obitsu Y, Shigematsu H, Yamashina A (2012) Obstructive sleep apnea as a potential risk factor for aortic disease. Heart Vessels 27:166–173
Maeno K, Kasai T, Kasagi S, Kawana F, Ishiwata S, Ohno M, Yamaguchi T, Narui K (2013) Relationship between atrial conduction delay and obstructive sleep apnea. Heart Vessels 28:639–645
Haas DC, Foster GL, Nieto FJ, Redline S, Resnick HE, Robbins JA, Young T, Pickering TG (2005) Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation 111:614–621
Phillips BA, Berry DT, Schmitt FA, Magan LK, Gerhardstein DC, Cook YR (1992) Sleep-disordered breathing in the healthy elderly. Clinically significant? Chest 101:345–349
Bliwise DL, Bliwise NG, Partinen M, Pursley AM, Dement WC (1988) Sleep apnea and mortality in an aged cohort. Am J Public Health 78:544–547
Mant A, King M, Saunders NA, Pond CD, Goode E, Hewitt H (1995) Four-year follow-up of mortality and sleep-related respiratory disturbance in non-demented seniors. Sleep 18:433–438
Lavie P, Lavie L, Herer P (2005) All-cause mortality in males with sleep apnoea syndrome: declining mortality rates with age. Eur Respir J 25:514–520
Ancoli-Israel S, Kripke DF, Klauber MR, Fell R, Stepnowsky C, Estline E, Khazeni N, Chinn A (1996) Morbidity, mortality and sleep-disordered breathing in community dwelling elderly. Sleep 19:277–282
Kobayashi M, Namba K, Tsuiki S, Matsuo A, Sugiura T, Inoue Y (2010) Clinical characteristics in two subgroups of obstructive sleep apnea syndrome in the elderly: comparison between cases with elderly and middle-age onset. Chest 137:1310–1315
Takama N, Kurabayashi M (2009) Influence of untreated sleep-disordered breathing on the long-term prognosis of patients with cardiovascular disease. Am J Cardiol 103:730–734
Martinez-Garcia MA, Campos-Rodriguez F, Catalan-Serra P, Soler-Cataluna JJ, Almeida-Gonzalez C, De la Cruz Moron I, Duran-Cantolla J, Montserrat JM (2012) Cardiovascular mortality in obstructive sleep apnea in the elderly: role of long-term continuous positive airway pressure treatment: a prospective observational study. Am J Respir Crit Care Med 186:909–916
Martinez-Garcia MA, Soler-Cataluna JJ, Ejarque-Martinez L, Soriano Y, Roman-Sanchez P, Illa FB, Canal JM, Duran-Cantolla J (2009) Continuous positive airway pressure treatment reduces mortality in patients with ischemic stroke and obstructive sleep apnea: a 5-year follow-up study. Am J Respir Crit Care Med 180:36–41
Parra O, Sanchez-Armengol A, Bonnin M, Arboix A, Campos-Rodriguez F, Perez-Ronchel J, Duran-Cantolla J, de la Torre G, Gonzalez Marcos JR, de la Pena M, Carmen Jimenez M, Masa F, Casado I, Luz Alonso M, Macarron JL (2011) Early treatment of obstructive apnoea and stroke outcome: a randomised controlled trial. Eur Respir J 37:1128–1136
Abe H, Takahashi M, Yaegashi H, Eda S, Tsunemoto H, Kamikozawa M, Koyama J, Yamazaki K, Ikeda U (2010) Efficacy of continuous positive airway pressure on arrhythmias in obstructive sleep apnea patients. Heart Vessels 25:63–69
Rechtschaffen AKA (1968) A manual of standardized terminology, techniques, and scoring system for sleep stages of human subjects. UCLA Brain information Service/Brain Research Institute, Los Angeles
Sleep Disorders Atlas Task Force of the American Sleep Disorders Association (1992) EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep 15:173–184
Sin DD, Fitzgerald F, Parker JD, Newton G, Floras JS, Bradley TD (1999) Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am J Respir Crit Care Med 160:1101–1106
Bradley TD, Holloway RM, McLaughlin PR, Ross BL, Walters J, Liu PP (1992) Cardiac output response to continuous positive airway pressure in congestive heart failure. Am Rev Respir Dis 145:377–382
Naughton MT, Rahman MA, Hara K, Floras JS, Bradley TD (1995) Effect of continuous positive airway pressure on intrathoracic and left ventricular transmural pressures in patients with congestive heart failure. Circulation 91:1725–1731
Tkacova R, Rankin F, Fitzgerald FS, Floras JS, Bradley TD (1998) Effects of continuous positive airway pressure on obstructive sleep apnea and left ventricular afterload in patients with heart failure. Circulation 98:2269–2275
Usui K, Bradley TD, Spaak J, Ryan CM, Kubo T, Kaneko Y, Floras JS (2005) Inhibition of awake sympathetic nerve activity of heart failure patients with obstructive sleep apnea by nocturnal continuous positive airway pressure. J Am Coll Cardiol 45:2008–2011
Narkiewicz K, Kato M, Phillips BG, Pesek CA, Davison DE, Somers VK (1999) Nocturnal continuous positive airway pressure decreases daytime sympathetic traffic in obstructive sleep apnea. Circulation 100:2332–2335
Waradekar NV, Sinoway LI, Zwillich CW, Leuenberger UA (1996) Influence of treatment on muscle sympathetic nerve activity in sleep apnea. Am J Respir Crit Care Med 153:1333–1338
Naughton MT, Benard DC, Liu PP, Rutherford R, Rankin F, Bradley TD (1995) Effects of nasal CPAP on sympathetic activity in patients with heart failure and central sleep apnea. Am J Respir Crit Care Med 152:473–479
Svatikova A, Wolk R, Lerman LO, Juncos LA, Greene EL, McConnell JP, Somers VK (2005) Oxidative stress in obstructive sleep apnoea. Eur Heart J 26:2435–2439
Buchner NJ, Quack I, Woznowski M, Stahle C, Wenzel U, Rump LC (2011) Microvascular endothelial dysfunction in obstructive sleep apnea is caused by oxidative stress and improved by continuous positive airway pressure therapy. Respiration 82:409–417
Jelic S, Padeletti M, Kawut SM, Higgins C, Canfield SM, Onat D, Colombo PC, Basner RC, Factor P, LeJemtel TH (2008) Inflammation, oxidative stress, and repair capacity of the vascular endothelium in obstructive sleep apnea. Circulation 117:2270–2278
Schulz R, Mahmoudi S, Hattar K, Sibelius U, Olschewski H, Mayer K, Seeger W, Grimminger F (2000) Enhanced release of superoxide from polymorphonuclear neutrophils in obstructive sleep apnea. Impact of continuous positive airway pressure therapy. Am J Respir Crit Care Med 162:566–570
Yokoe T, Minoguchi K, Matsuo H, Oda N, Minoguchi H, Yoshino G, Hirano T, Adachi M (2003) Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation 107:1129–1134
Daida H, Miyauchi K, Ogawa H, Yokoi H, Matsumoto M, Kitakaze M, Kimura T, Matsubara T, Ikari Y, Kimura K, Tsukahara K, Origasa H, Morino Y, Tsutsui H, Kobayashi M, Isshiki T, PACIFIC investigators (2013) Management and two-year long-term clinical outcome of acute coronary syndrome in Japan: prevention of atherothrombotic incidents following ischemic coronary attack (PACIFIC) registry. Circ J 77:934–943
Lavie P, Lavie L (2009) Unexpected survival advantage in elderly people with moderate sleep apnoea. J Sleep Res 18:397–403
Acknowledgments
The authors thank Ryoko Asanuma for excellent technical support. The authors are indebted to Associate Professor Edward F. Barroga (DVM, PhD) of the Department of International Medical Communications of Tokyo Medical University for the editorial review of the English manuscript. The authors have received no grant support for this study.
Conflict of interest
The authors declare no potential conflicts of interest associated with this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nishihata, Y., Takata, Y., Usui, Y. et al. Continuous positive airway pressure treatment improves cardiovascular outcomes in elderly patients with cardiovascular disease and obstructive sleep apnea. Heart Vessels 30, 61–69 (2015). https://doi.org/10.1007/s00380-013-0451-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-013-0451-x