Abstract
Purpose
To evaluate the effect of long-term continuous positive airway pressure (CPAP) treatment on disease severity of obstructive sleep apnea (OSA).
Methods
We analyzed results from the Sleep Apnea and Cardiovascular Events (SAVE) study involving participants recruited at the Guangdong Provincial People’s Hospital, China. Participants were aged 45–75 years with a history of cardiac or cerebrovascular disease. OSA was confirmed by home sleep apnea testing (HSAT). Participants were randomized to receive CPAP plus standard cardiovascular care (CPAP group) or standard care alone (UC group) and followed for several years. At the study conclusion, surviving participants were invited to repeat HSAT. Changes in OSA indicators were compared by independent samples t-tests and subgroup analysis was implied among groups stratified by OSA severity.
Results
One hundred two adults were recruited (51 per group) and followed for 48.0 ± 14.5 months. Daily CPAP usage in the CPAP group was 4.1 ± 1.9 h. AHI decreased from baseline to end-of-study in both CPAP and UC groups (− 5.0 (− 12.5,2.0), P = 0.000; − 4.0 (− 12.5,1.5), P = 0.007, respectively), with no between-group difference (P = 0.453). An improvement in nadir SpO2 showed from baseline to end-of-study in the CPAP but not UC group (2.3% ± 6.1%, P = 0.011 and − 0.7% ± 7.6%, P = 0.511, respectively; between-group difference P = 0.032). Subgroup analysis shows that CPAP could improve AHI in patients with moderate OSA (− 8.0 (− 11.8, − 2.8) in CPAP group, − 2.0 (− 0.8,6.0) in UC group, P = 0.022) and improve nadir SpO2 in patients with severe OSA (5.0 (− 0.8, − 0.8,7.0) in CPAP group, 0.0 (− 8.5,2.5) in UC group, P = 0.032).
Conclusion
Long-term CPAP use did not result in clinically significant changes in AHI or ODI overall but showed variable effects stratified by OSA severity.
Clinical Trial Registration
Registry: Clinical Trials.gov, title: Continuous Positive Airway Pressure Treatment of Obstructive Sleep Apnea to Prevent Cardiovascular Disease (SAVE), URL: www.clinicaltrials.gov, identifier: NCT00738179.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a disorder characterized by repetitive partial (hypopnea) or complete (apnea) collapse of the upper airway during sleep [1]. However, the mechanisms involved are not very clear. Continuous positive airway pressure (CPAP), the first-line treatment of OSA, has an immediate positive effect on breathing during sleep [2]. It improves or eliminates obstructive breathing events and nocturnal hypoxemia and reduces arousals [3, 4]. Whether or not these effects are strictly transient, or have, over time, a sustained impact on underlying AHI is unclear.
Loud snoring and severe OSA have been associated with upper airway inflammation and edema, sensorineural injury, and partial muscle denervation [5], as well as an increase in the arousal threshold to respiratory stimuli [6], which may progressively worsen OSA. Several of these abnormalities may be improved with CPAP treatment [5, 6] but it is uncertain if this is sufficient to improve OSA to a clinically significant extent. Several previous studies of patients treated with CPAP for a few months to approximately a year showed a small decrease in the frequency of sleep apnea and hypopnea events (apnea–hypopnea index, AHI) after withdrawal of CPAP compared with the AHI at time of diagnosis [7,8,9,10,11,12]. In one study, approximately 15% of individuals with OSA (AHI > 10 events per hour) who had used CPAP consistently for > 12 months did not experience significant recurrence of AHI after stopping CPAP for 4 days and 2 weeks [13]. However, there have been no randomized controlled studies that allow the effects of several years of CPAP treatment to be ascertained while controlling for other changes that might occur in patients with OSA who are untreated.
The Sleep Apnea and Cardiovascular Endpoints (SAVE) study was an international, multicenter, randomized controlled trial of patients with coexisting CV disease and moderate-to-severe OSA who were randomly allocated to receive CPAP plus usual cardiovascular care or usual cardiovascular care alone and followed for approximately 4 years. This secondary analysis in a subpopulation of SAVE participants provides an opportunity to assess the effect of long-term CPAP treatment on the severity of OSA.
Methods
Participants
Patients included in this sub-study were those who had provided written informed consent at the Guangdong Provincial People’s Hospital to participate in the SAVE trial (NCT00738179) [14]. Participants were aged 45 to 75 years, and had established CV disease and co-occurring moderate-severe OSA. Patients were excluded if they had severe daytime sleepiness (Epworth Sleepiness Scale [ESS] score > 15), very severe nocturnal hypoxemia (oxygen saturation < 80% for > 10% of the monitoring time), or a predominantly Cheyne-Stokes respiration pattern on home sleep apnea testing (HSAT). Potential participants were required to adhere to a 1-week trial of sham CPAP (REMstar Auto M Series, Philips Respironics, Inc. with pressure set to sub-therapeutic levels) to evaluate willingness and likely ability to adhere to the treatment. Those who recorded a daily average sham CPAP usage ≥ 3 h were included. Full details of the study have been outlined elsewhere [14, 15]. Details of the design have been published previously [16, 17].
HSAT monitoring and scoring
Specially trained persons were responsible for HSAT monitoring at baseline and at the end of the study. HSAT was conducted using a cardiorespiratory polygraphy device (ApneaLink, ResMed, Bella Vista, Sydney, Australia). ApneaLink is a type 3 portable sleep monitoring device. Respiration was monitored with a nasal cannula, chest and abdominal bands, and pulse oximeter. Participants learned how to operate the device at hospital and completed sleep monitoring at their home. Participants in the CPAP group were instructed not to use CPAP on the night of the end-of-study recording. Each study was automatically analyzed, after data were reviewed at a central core sleep laboratory to ensure it met pre-specified duration and quality standards. Obstructive sleep apnea was defined as a reduction ≥ 90% in airflow for ≥ 10 s during sleep with persistent ventilatory efforts while likely Cheyne-Stokes respiration indicative of central sleep apnea was identified by typical crescendo-decrescendo airflow patterns. Hypopnea was defined as a reduction of ≥ 30% airflow for ≥ 10 s, associated with a desaturation > 4% of oxygen. The AHI was calculated as the total number of apneas and hypopneas divided by the total recording time [18]. The oxygen desaturation index (ODI) was defined as the number of ≥ 4% oxygen desaturation events per hour. Moderate to severe OSA was defined as an ODI ≥ 12/h.
Randomization
A special website (http://vmprdinf001.iih.usyd.edu.au/saveuat/pfts.dll?PVN=13) was designed for the randomization and data collection of this study. The randomization software was based in a system named FLEXETRIALS. All eligible subjects were randomly assigned to receive either CPAP therapy plus usual care (CPAP group) or usual care alone (usual-care group). Randomization was performed with the use of a minimization procedure to balance the group assignments according to site, type of cardiovascular disease (cardiac, cerebrovascular, or both), and severity of daytime sleepiness (Epworth Sleepiness Scale score < 11 vs. ≥ 11). This step was unblinded and subjects who met all inclusion/exclusion criteria were entered onto the study in the website by the principal investigator.
CPAP treatment and follow-up
All participants were followed-up at 1, 3, 6, and 12 months and annually thereafter. Participants were also contacted by telephone at 6 months between the annual clinic visits. Additional end-of-study visits were performed between September 2015 and January 2016 on all participants who remained actively enrolled in the trial. CPAP adherence was recorded at each follow up visit and reported as a time-weighted mean value for each participant across their whole study follow-up period.
Statistical analysis
Continuous variables were expressed in the form of the mean ± standard deviation (SD) or median (lower quartile: upper quartile) as appropriate. Categorical variables were presented as percentages. We compared baseline characteristics between CPAP and UC groups using a two-sample independent t-test or nonparametric test as appropriate. The changes in the HSAT indicators from baseline to end of study were compared between treatment groups to clarify the effect of CPAP on AHI, ODI, and measurements of SpO2. Subgroup analysis was further implied to explore the effect of CPAP on different degrees of OSA severity. Data analysis was conducted using SPSS software (SPSS standard version 25.0, SPSS Inc.).
Results
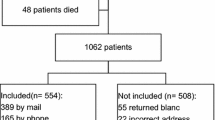
There were 151 participants in the SAVE study at the Guangdong Provincial People’s Hospital site. Forty-nine participants were unable to be included in the present analysis: 7 had died in the observation phase, 10 were lost to follow-up, and 32 refused the HSAT reevaluation, leaving 102 participants (83% male), aged (mean ± SD) 61.9 ± 6.8 years who were followed for 48.0 ± 14.5 months (Fig. 1). Table 1 lists the baseline characteristics of these participants. Figure 2 shows the nightly usage of CPAP during follow-up in the CPAP group. The mean nightly CPAP adherence over the whole duration of follow-up in those allocated to receive the treatment was 4.1 ± 1.9 h. Table 2 describes the changes in AHI, ODI, and other OSA indicators from baseline to end of study. Although there was a decrease in AHI in both CPAP and UC groups (mean (95% CI): − 5.0 (− 12.5,2.0) and − 4.0 (− 12.5,1.5) events per hour, respectively), no statistical difference was evident between the two groups. Similarly, there were no significant differences between treatment groups in ODI though there were significant intra-group differences from baseline to the end of the study. The decrease of AHI was mainly due to a decrease in the apnea index. Long-term CPAP showed a positive effect on nadir SpO2. Supplementary Table S1 lists some anthropometric variables that are known to be related to AHI and ODI. There were small increases in neck and waist circumference in CPAP and UC groups but no between group differences.
Patients were categorized into three subgroups based on disease severity and the effect of long-term CPAP on OSA severity was further exploded. Table 3 shows that long-term CPAP showed a positive effect on AHI in moderate OSA group (− 8.0 (− 11.8, − 2.8) in CPAP group, − 2.0 (− 0.8,6.0) in UC group, P = 0.022) and improve nadir SpO2 in severe OSA group (5.0 (− 0.8, − 0.8,7.0) in CPAP group, 0.0 (− 8.5,2.5) in UC group, P = 0.032). Supplementary Table S2 lists the baseline characteristics of these participants according to subgroups.
Discussion
The main finding of this study was that long-term CPAP treatment had no effect on the underlying severity of sleep disordered breathing as measured by either AHI or ODI. A small reduction in AHI and ODI occurred in both study groups with no between-group differences. However, CPAP did result in a small positive effect on the nadir night-time oxygen saturation. Further subgroup analysis showed that CPAP may have a variable effect according to the severity category of OSA.
These results appear to be at variance with several previously published studies [7,8,9,10,11,12,13] which reported small reductions in the frequency of obstructive breathing events after several months of CPAP. However, these studies were designed as before and after studies and lacked a control group.
We can only speculate as to possible reasons for the small reductions in AHI and ODI observed in both CPAP and UC groups. It could be due to regression to the mean, or, alternatively, a Hawthorne effect whereby participants, simply by virtue of being enrolled in a clinical trial, altered one or more other behaviors (e.g., medication adherence, improvements in alcohol, diet or exercise) that improved OSA severity. However, in the present sub-study population a small increase rather than decrease in weight was observed in the CPAP-treated participants [15]. The decrease of AHI and ODI could also be explained by the natural history of OSA. However, evidence from previous longitudinal studies is highly variable with one study reporting an increase in AHI but no change in SpO2 parameters over 3 years [20]. Another study of 100 patients with OSA followed for 5 years showed no change in AHI [21], and a further study of 152 patients with moderate to severe OSA followed for 7 years showed a decrease in AHI but worsening of sleep oxygenation [22].
Compared with the UC group, the CPAP group showed an improvement in nadir SpO2 (and marginal improvement in time spent below 90% SpO2) despite there being no between-group difference in the frequency of obstructive events. One possibility is that CPAP treatment caused a reduction in the ratio of apnea to hypopnea events such that the decrease in ventilation per event might tend to be less. An increase in the size of the pharynx (awake) [23] and a reduction in the proportion of sleep apneas versus hypopneas [9, 10] have been previously reported following prolonged CPAP treatment. In this study, however, there was no change in the ratio of apneas to hypopneas within or between groups. Another possibility is that the average length of obstructive events was decreased because of a decrease in arousal threshold (i.e., subjects aroused more quickly to an obstruction [6]). Finally, a change in sleep architecture could also explain the results: there are two reports of less REM sleep and more non-REM sleep after withdrawal of long-term CPAP compared with pretreatment sleep studies [8, 10]. Unfortunately, the information recorded by the ApneaLink device did not allow us to explore these latter two possible mechanisms.
Whatever the explanations for the changes observed between and within groups in SpO2 and AHI, it is important to acknowledge that they were very small and are unlikely to be clinically significant. The observed decrease in AHI of 5 events per hour in both groups is well below the agreed minimal clinically significant change in AHI of 15 events per hour [24]. Furthermore, previous studies point to the transient nature of any improvement in the underlying severity of OSA as a result of CPAP treatment [7]. Our results, combined with those of previous studies do not therefore support the proposition that brief “vacations” from CPAP can be safely taken in patients with moderate to severe OSA who are prescribed long-term CPAP treatment. Our study suggests that CPAP treatment alone is unlikely to resolve the physiological abnormalities underpinning OSA, and therefore needs to be prescribed as an indefinite treatment.
Our subgroup analysis found that CPAP only decreased AHI and AI in patients with moderate OSA and increased nadir and mean SpO2 in patients with severe OSA. Few studies have focused on this kind of phenomenon and the possible meanings hidden behind need to be further investigated.
We acknowledge that this post hoc sub-study of the main SAVE trial has several limitations. First, it was conducted at a single site on a relatively small sample. Greater precision would have been possible had we used more participants’ data from across the recruitment network. However, CPAP participants at this site had considerably higher adherence to CPAP than for the study population as a whole, and the mean follow-up period was longer. The sample size provided ample statistical power to definitively answer whether or not a clinically significant change in OSA was present after sustained CPAP treatment. Second, the study population had established CV disease and was somewhat older compared with patients attending sleep clinics; and patients with very severe nocturnal hypoxemia or a predominantly Cheyne-Stokes respiration pattern were excluded. The study results may not therefore extrapolate to general sleep apnea clinic populations. Lastly, we used a type 3 portable sleep monitoring device in this study. The device was chosen because of the unavailability of polysomnography (PSG) in many recruitment sites and the cost and difficulty of setting up and standardizing PSG measurements across multiple centers and countries. The ApneaLink™ automated screening device provided a reliable and generalizable alternative. It was validated against PSG in a high cardiovascular-risk Chinese population before the SAVE trial and found to have high diagnostic accuracy for moderate to severe OSA [25]. It is unlikely therefore to have influenced the overall findings in this study. Nonetheless, the parameters collected to evaluate the severity of OSA were limited, preventing, for example, an evaluation of whether or not the length of obstructive events changed after CPAP treatment.
In summary, long-term CPAP use in patients with comorbid OSA and cardiovascular disease did not result in clinically significant change in AHI or ODI when compared with patients without CPAP, but showed a small positive effect on nadir SpO2.
Data availability
The detailed participant data are available from the corresponding author upon reasonable request.
References
Lévy P, Kohler M, McNicholas WT, Barbé F, McEvoy RD, Somers VK, Lavie L, Pépin J-L (2015) Obstructive sleep apnoea syndrome. Nat Rev Dis Primers 1:15015
Iftikhar IH, Bittencourt L, Youngstedt SD, Ayas N, Cistulli P, Schwab R, Durkin MW, Magalang UJ (2017) Comparative efficacy of CPAP, MADs, exercise-training, and dietary weight loss for sleep apnea: a network meta-analysis. Sleep Med 30:7–14
Radovanovic D, Rizzi M, Airoldi A, Mantero M, Di Marco F, Raccanelli R, Santus P (2019) Effect of continuous positive airway pressure on respiratory drive in patients with obstructive sleep apnea. Sleep Med 64
Dewan NA, Nieto FJ, Somers VK (2015) Intermittent hypoxemia and OSA: implications for comorbidities. Chest 147:266–274
Saboisky JP, Butler JE, Gandevia SC, Eckert DJ (2012) Functional role of neural injury in obstructive sleep apnea. Front Neurol 3:95
Eckert DJ, Younes MK (2014) Arousal from sleep: implications for obstructive sleep apnea pathogenesis and treatment. J Appl Physiol (Bethesda, Md.: 1985) 116:302–313
Kohler M, Stoewhas A-C, Ayers L, Senn O, Bloch KE, Russi EW, Stradling JR (2011) Effects of continuous positive airway pressure therapy withdrawal in patients with obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 184:1192–1199
Rolfe I, Olson LG, Saunders NA (1991) Long-term acceptance of continuous positive airway pressure in obstructive sleep apnea. Am Rev Respir Dis 144:1130–1133
McEvoy RD, Thornton AT (1984) Treatment of obstructive sleep apnea syndrome with nasal continuous positive airway pressure. Sleep 7:313–325
Young LR, Taxin ZH, Norman RG, Walsleben JA, Rapoport DM, Ayappa I (2013) Response to CPAP withdrawal in patients with mild versus severe obstructive sleep apnea/hypopnea syndrome. Sleep 36:405–412
Kribbs NB, Pack AI, Kline LR, Getsy JE, Schuett JS, Henry JN, Maislin G, Dinges DF (1993) Effects of one night without nasal CPAP treatment on sleep and sleepiness in patients with obstructive sleep apnea. Am Rev Respir Dis 147:1162–1168
Song P, Kim S, Kim D, Joo EY, Hong SB (2012) Long term effects of continuous positive airway pressure in obstructive sleep apnea patients: apnea-hypopnea index and blood pressure changes. Sleep Med Res 3:20–26
Rossi VA, Schwarz EI, Bloch KE, Stradling JR, Kohler M (2014) Is continuous positive airway pressure necessarily an everyday therapy in patients with obstructive sleep apnoea? Eur Respir J 43:1387–1393
McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, Zhang X, Mediano O, Chen R, Drager LF, Liu Z, Chen G, Du B, McArdle N, Mukherjee S, Tripathi M, Billot L, Li Q, Lorenzi-Filho G, Barbe F, Redline S, Wang J, Arima H, Neal B, White DP, Grunstein RR, Zhong N, Anderson CS (2016) CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med 375:919–931
Ou Q, Chen B, Loffler KA, Luo Y, Zhang X, Chen R, Wang Q, Drager LF, Lorenzi-Filho G, Hlavac M, McArdle N, Mukherjee S, Mediano O, Barbe F, Anderson CS, McEvoy RD, Woodman RJ (2019) the effects of long-term CPAP on weight change in patients with comorbid OSA and cardiovascular disease: data from the SAVE trial. Chest 155:720–729
Antic NA, Heeley E, Anderson CS, Luo Y, Wang J, Neal B, Grunstein R, Barbe F, Lorenzi-Filho G, Huang S, Redline S, Zhong N, McEvoy RD (2015) The Sleep Apnea cardioVascular Endpoints (SAVE) Trial: rationale, ethics, design, and progress. Sleep 38:1247–1257
Heeley E, Billot L, Anderson CS, Antic NA, Neal B, McEvoy RD (2016) Statistical analysis plan for the Sleep Apnea cardioVascular Endpoints study: an international randomised controlled trial to determine whether continuous positive airways pressure treatment for obstructive sleep apnea in patients with CV disease prevents secondary cardiovascular events. Int J Stroke 11:148–150
Collop NA, Anderson WM, Boehlecke B, Claman D, Goldberg R, Gottlieb DJ, Hudgel D, Sateia M, Schwab R (2007) Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. J Clin Sleep Med 3:737
Godin G, Shephard RJ (1985) A simple method to assess exercise behavior in the community. Canadian journal of applied sport sciences. Can J Appl Sport Sci 10:141–146
Yesavage JA, Kinoshita LM, Noda A, Lazzeroni LC, Fairchild JK, Friedman L, Sekhon G, Thompson S, Cheng J, Zeitzer JM (2014) Longitudinal assessment of sleep disordered breathing in Vietnam veterans with post-traumatic stress disorder. Nat Sci Sleep 6:123–127
Sforza E, Addati G, Cirignotta F, Lugaresi E (1994) Natural evolution of sleep apnoea syndrome: a five year longitudinal study. Eur Respir J 7:1765–1770
Sforza E, Hupin D, Pichot V, Barthélémy JC, Roche F (2017) A 7-year follow-up study of obstructive sleep apnoea in healthy elderly: The PROOF cohort study. Respirology (Carlton, Vic.) 22:1007–1014
Mortimore IL, Kochhar P, Douglas NJ (1996) Effect of chronic continuous positive airway pressure (CPAP) therapy on upper airway size in patients with sleep apnoea/hypopnoea syndrome. Thorax 51:190–192
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med 15:335–343
Gantner D, Ge JY, Li LH, Antic N, Windler S, Wong K, Heeley E, Huang SG, Cui P, Anderson C, Wang JG, McEvoy D (2010) Diagnostic accuracy of a questionnaire and simple home monitoring device in detecting obstructive sleep apnoea in a Chinese population at high cardiovascular risk. Respirology 15:952–960
Acknowledgements
We gratefully thank the Statistics Office, Information and Statistics Center, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences) for excellent statistical assistance in this work.
Funding
The Sleep Apnea Cardiovascular Endpoints (SAVE) trial was funded by project grants [1006501 and 1060078] from the National Health and Medical Research Council of Australia and by the Respironics Sleep and Respiratory Research Foundation and Philips Respironics. Supplementary funding was provided by Fisher & Paykel Healthcare and the Australasian Sleep Trials Network [enabling grant 343020 from the National Health and Medical Research Council]. In-kind donations were provided by Respironics for the CPAP equipment and by ResMed for the sleep apnea diagnostic devices. This sub-study was supported by a grant [National Natural Science Foundation of China 81870077] to Q. O.
Author information
Authors and Affiliations
Contributions
The study was designed by DM, QO, KL, and YC; data were collected by YC, QO, BC, YX, QW, and ML; data were analyzed by YC and results interpreted by all authors. The manuscript and figures were drafted by YC and critically revised by QO, DM, and KL. QO serves as the guarantor of the paper, taking responsibility for the integrity of the work as a whole, from inception to publication of the article.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Participants signed ethics committee-approved consent forms prior to participation.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cheng, Y., Ou, Q., Chen, B. et al. The changes of AHI after long-term CPAP in patients with comorbid OSA and cardiovascular disease. Sleep Breath 27, 511–518 (2023). https://doi.org/10.1007/s11325-022-02633-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02633-y