Abstract
This study was performed to evaluate surgical outcomes in octogenarian patients undergoing valve surgery. Sixty patients (mean age 82.3 ± 1.9 years) who underwent valve surgery were reviewed. Aortic valve disease was found in 65% of the patients. Preoperatively, 20% of the patients were in NYHA class IV. An urgent operation and concomitant coronary artery bypass grafting were performed in ten patients each. A bioprosthetic valve was exclusively used for valve replacement except in two patients. Mitral valve repair was done in seven patients. Operative mortality was 13.3% for the period. No risk factors for operative mortality were detected by multivariate analysis; however, urgent operation, preoperative NYHA class IV, preoperative renal dysfunction, perioperative use of an intra-aortic balloon pumping, and prolonged cardiopulmonary bypass time had significant effects on operative mortality. The actuarial survival rate at 1 and 3 years after surgery was 82.6 and 71.5%, respectively, and 97.6% of late survivors reported that their activity level was equal to or better than the preoperative level. Valve surgery can be performed in octogenarian patients with acceptable mortality, good long-term results, and good quality of life. Early referral to surgery should be important to obtain a better postoperative outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As more and more people live to the age of 80 or older, the indications for cardiac valve surgery in the elderly are expanding considerably [1, 2]. Some 20–40% of the elderly population has symptomatic heart disease, and some of these will become candidates for valve operations [1, 3, 4]. Although excellent functional outcomes with satisfactory long-term survival rates after valve operations, mainly aortic valve replacement, in patients aged 80 years or older have been described in the literature, some practitioners are still hesitant to refer mildly symptomatic elderly patients for surgical intervention [5]. This may be due, in part, to fears that an elderly person would be unable to withstand extracorporeal circulation, concern about the quality of the tissues, worries about multisystemic disease, and incomplete appreciation of the life expectancy of people that have reached the age of 80 years.
To cast further light on these issues, we reviewed our operative and long-term results of valve surgery in patients aged 80 years or older.
Patients and methods
Patients
This study was approved by The Ethics Committee of Kurume University, and individual patient consent was waived. Between January 1994 and June 2008, a total of 1,447 patients underwent heart valve surgery at Kurume University Hospital. Of these, 60 (4.1%) were 80 years or older at the time of surgery, and these patients form the basis of this study. The clinical characteristics of these patients are summarized in Table 1. Patients’ age ranged from 80 to 87 years with a mean age of 82.3 ± 1.9 years. The indication of valve surgery was aortic valve disease, mainly aortic stenosis, in 39 patients (65.0%), mitral valve disease in 15 (25.0%), and combined aortic and mitral valve disease in the remaining 6 (10.0%). The valve pathology that required surgical treatment was calcification in 30 patients and leaflet prolapse or rupture of the chordae tendineae in 22 patients. According to the New York Heart Association (NYHA) functional classification, 37 (61.7%) of the 60 patients were in class III and 12 (20%) were in class IV preoperatively. An urgent operation (defined as surgery performed within 24 h after the first referral to cardiac surgeons) was performed on ten patients (16.7%), and two patients (3.3%) had a history of previous cardiac operation.
Preoperative cardiac co-morbidities and associated extracardiac diseases in the 60 patients are also summarized in Table 1.
Operative technique and postoperative anticoagulant therapy
The surgical approach was through a median sternotomy, and cardiopulmonary bypass (CPB) with moderate systemic hypothermia (28–32°C) was employed in all patients but two who simultaneously underwent hemi-arch replacement. Myocardial protection was achieved with antegrade and retrograde cold blood cardioplegia in all of the patients except for one patient who received aortic valve replacement (AVR) with crystalloid cardioplegia prior to 1995. Operative procedures performed on the 60 patients are shown in Table 2. Standard techniques for implantation of prosthetic valves were employed [6], and aortic root replacement was performed with a composite valved graft. A bioprosthetic valve was used in 51 patients (54 valves) in either the aortic or mitral valve position, and a bileaflet mechanical valve was used in 2 patients because of the patients’ preferences. For mitral valve repair, standard reparative techniques [7] were used on ten patients, and coronary artery bypass grafting (CABG) was concomitantly performed on ten patients. The mean cardiopulmonary bypass time was 179.8 ± 76.1 min (range 95–422 min), and the mean aortic cross-clamp time was 133.4 ± 58.6 min (range 62–341 min).
Postoperatively, all patients with a mechanical valve received anticoagulant therapy with warfarin and an antiplatelet agent throughout the follow-up period, and the international normalized ratio was kept in the range of 1.6–2.5. Anticoagulant therapy was also given to the patients with a bioprosthetic valve and to the patients undergoing mitral valve repair within the first 3 months after surgery, and thereafter, it was withdrawn, except in patients with atrial fibrillation.
Follow-up studies
Patient status after hospital discharge was evaluated annually or biannually by cardiologists or cardiac surgeons in our hospital. At the time of this study, the current clinical evaluation was obtained by a review of hospital records and by direct contact or patient questionnaire. Deaths and complications were strictly defined according to published guidelines of The Society of Thoracic Surgeons and The American Association for Thoracic Surgery.
Statistical analysis
Statistical analyses were performed using the JMP, The Statistical Discovery Software (version 5.0.1J, SAS Institute Inc., Cary, NC). Distributions of all relevant variables were expressed either as counts and proportions or as mean ± standard deviation. The effects of nominal risk factors on early mortality were evaluated univariately by chi-square test or Fisher’s exact test. Combinations of risk factors were multivariately evaluated with multiple logistic regression models, using the stepwise method to determine the best predictors.
Results
Operative mortality
Of the 60 patients, 8 died early after valve surgery, giving an operative mortality rate of 13.3%. Of these eight patients, five (8.3%) died within 30 days after valve surgery (30-day mortality), and the remaining three patients (5.0%) died before discharge from the hospital (a hospital death). Causes of the 30-day mortality were low cardiac output syndrome (LOS) and/or multiple organ failure (MOF) in three patients, deterioration of neurological deficits resulting from preoperative septic embolism and persistent sepsis caused by methicillin-resistant Staphylococcus aureus infective endocarditis, and bleeding due to injury of the coronary sinus in one patient each, and causes of hospital deaths in the three patients were pneumonia in two and MOF in one, as shown in Table 3. According to the preoperative NYHA functional classification, all eight patients (16.3%) were in class III or IV, whereas there were no operative deaths in class II.
Late mortality
Of the 60 patients, 52 were discharged from the hospital, and all of these patients were followed up. The follow-up period ranged from 75 days to 11.5 years with a mean follow-up period of 3.4 ± 3.1 years, and the total follow-up period was 176.2 patient-years.
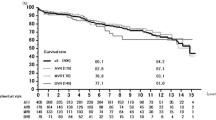
A total of 11 patients died during the follow-up period. Pneumonia or its complication was the cause in four patients, heart failure in two, cerebral bleeding in two, and type A aortic dissection, malignant tumor or senility in one each. Of the two patients who suffered cerebral bleeding, one patient receiving successful mitral valve repair was on anticoagulant therapy with warfarin for three-vessel coronary artery disease that had been treated by single CABG and repair of a ventricular septal perforation 15 years previously, despite a normal sinus rhythm. The other patient also had a normal sinus rhythm, and neither warfarin nor any antiplatelet agents were prescribed because she had received mitral valve replacement (MVR) with a bioprosthetic valve. Cardiac related deaths were found in 2 patients, but no valve-related deaths, including thromboembolism and bleeding events, were observed in these 52 patients. The actuarial survival rates, including operative deaths, were 82.6, 71.5 and 68.0% at 1, 3 and 5 years after surgery, respectively. These actuarial survival rates were almost equal to expected survival rates in normal Japanese population, as shown in Fig. 1.
Among valve-related complications, anticoagulant-related hemorrhage occurred in three patients (intestinal bleeding in two and subarachnoid hemorrhage in one) within 3 months after surgery, and these three patients recovered by conservative therapy without any sequelae. Paravalvular leak was observed in the aortic position in one patient, but it was not serious enough to require reoperation. In addition, cerebral infarction developed 10.6 years after mitral valve repair in one patient who was at the age of 93.
Postoperative NYHA functional class and quality of life assessment
Preoperative mean NYHA functional class in the 60 patients was 3.0 ± 0.6. At the time of follow-up, the NYHA functional class and activity level of 41 survivors were assessed. Postoperatively, 36 (87.8%) of the 41 patients were in NYHA class I, and 5 (12.2%) were in class II, and their activity level [1] was rated as heavy, defined as capable of lifting heavy objects, in 12 patients (29.3%), moderate, defined as the ability to do cleaning, in 20 (48.8%), and light, defined as activities of daily living, in 8 (19.5%), and bedridden in 1 (2.4%) who suffered cerebral infarction at the age of 93. All of the 41 long-term survivors reported that their decision to have valve surgery after the age of 80 had been a good choice.
Discussion
About 20–40% of the population aged 80 years or older has symptomatic cardiovascular disease [1, 3, 4], and the most frequent condition is aortic stenosis resulting from valve calcification [1]. Therefore, the number of valve surgeries for octogenarians is expected to continue to increase in the future.
In this study, the overall operative mortality was 13.3% with a 30-day mortality of 8.3%, decreasing from 31.3% (5 of 16 patients) in the initial 8 years (1994–2001) to 6.8% (3 of 44 patients, AVR; 6.5%, mitral valve surgery; 9.1%) in the last 7 years. In previously reported series, the operative mortality ranged from 4 to 29% in AVR [4] and from 6.5 to 15.5% in mitral valve surgery [2, 8]. Recently, hospital mortality was reported to be 6.5% after AVR and 25% after mitral valve surgery in octogenarians [9]. These results are very close to our operative mortality. Although the operative mortality was higher than that in our patients younger than 80 years, the increase was slight and is not considered to be prohibitive for valve operations in octogenarians, as reported in other studies [4, 9]. These results suggest that valve surgery can be performed with an acceptable risk in patients older than 80 years of age.
In aortic valve surgery, previous studies have demonstrated various independent predictors for operative mortality, such as low left ventricular ejection fraction, urgent or emergent surgery, preoperative NYHA class IV, concomitant CABG, a prolonged CPB time, postoperative renal dysfunction, and perioperative use of intra-aortic balloon pumping (IABP) [1–5]. Similarly, in mitral valve surgery, emergency surgery, preoperative NYHA class IV, angina, mitral valve replacement, concomitant CABG and age over 80 years have been indicated as significant predictors for operative mortality [8, 9]. Furthermore, DiGregorio and colleagues [10] showed that preoperative NYHA class III–IV was significantly associated with prolonged hospital stay and emphasized that favorable preoperative NYHA class has been associated with favorable long-term survival in the elderly population. In our study, no significant risk factors for operative mortality were detected by multivariate logistic regression analysis because of the small number of patients operated on and the low number of operative deaths; however, univariate analysis revealed urgent operation, preoperative NYHA class IV, perioperative use of IABP and prolonged CPB time, in addition to preoperative renal dysfunction, had a significant effect on operative mortality. Concomitant CABG has been a well-documented risk factor for all cardiac valve surgery [2, 11–13], but a recent study [5] has indicated that concomitant CABG was protective of operative mortality and improved long-term survival. Prolongation of CPB time attributed to concomitant CABG, however, may increase the risk of adverse events in octogenarians. Since other therapeutic procedures such as percutaneous coronary interventions are now available, only those with critical coronary lesions or severe angina should undergo concomitant CABG, and less than complete revascularization may be an acceptable alternative in these elderly patients when congestive heart failure is a primary indication of operation [12, 14]. Of our eight patients who died early after surgery, seven had several risk factors simultaneously and were in extremely critical condition preoperatively. These critical patients are defined as “salvage” patients, in whom high operative mortality was reported, even in patients younger than 80 years [15]. Furthermore, a previous study showed that risk reaches 40% when left heart failure, NYHA class IV, emergency surgery, aortic regurgitation and cardiomegaly occur concurrently [16]. These results suggest the importance of early operation on elderly patients with valve disease, avoiding development of advanced heart failure and “salvage” operations.
In the reported series, the actuarial survival rate was 82% at 1 year, 70% at 3 years and 56% at 5 years after AVR [6], and in mitral valve surgery, it was 52.3% at 7 years postoperatively [2]. In the present study, actuarial survival rates, including operative death, were 82.6, 71.5 and 68.0% at 1, 3 and 5 years after surgery, respectively. These survival rates are comparable with those in other studies and show good long-term survival despite advanced age.
Of at least equal importance to the elderly as survival is quality of life. In this study, all of the 41 long-term survivors reported that their decision to receive valve surgery after the age of 80 years had been a good choice. Furthermore, at a mean follow-up of 3.4 years postoperatively, 97.6% of survivors maintained the same preoperative or improved activity level. These findings were similar to those reported in previous studies [11, 17], and no valve-related complications with permanent disability were observed.
In aortic valve surgery, calcification of the aortic valve leading to aortic stenosis is the predominant lesion, and valve replacement is recognized as the sole curative treatment [4]. In this series, a bioprosthetic valve was used for all patients in the aortic position except for two patients. Although minor anticoagulant-related bleeding occurred in 3 patients early after surgery, there were no valve-related deaths or complications, including reoperation for primary tissue failure. These results suggest that bioprosthetic valves are appropriate in octogenarians, particularly in the aortic position. As postoperative anticoagulant therapy for elderly patients with a bioprosthetic valve, a variety of regimens, a combination of warfarin and an antiplatelet, warfarin alone, an antiplatelet alone, or none, has been described [18]. Among these, the usefulness of antiplatelets after AVR with a bioprosthesis has been recently reported in several papers [19], and a prospective study by Gherli and colleagues [20] showed no significant difference in rates of cerebral ischemic events, major hemorrhages or overall survival between patients who received warfarin for the first 3 months and patients treated with aspirin alone. Considering these results and better quality of life resulting from the avoidance of repeated blood tests and dosage adjustments of warfarin, antiplatelet therapy alone after AVR with a bioprosthesis may be sufficient for octogenarian patients without thromboembolic risk factors. We believe that a further study should be performed to make the decision whether to use anticoagulation or antiplatelet therapy, as well as the duration and level of anticoagulation.
Among 15 patients with mitral valve disease, 7 patients (46.7%) underwent mitral valve repair and 8 (53.2%) received MVR with a bioprosthetic valve. In the elderly, the question of whether to select valve repair or valve replacement is controversial because MVR with a bioprosthetic valve has a high structural deterioration-free rate and does not require anticoagulant therapy, and also allows preservation of left ventricular performance by chordal sparing technique. However, mitral valve replacement was considered to be a significant independent risk factor for mortality, and mitral valve repair had a significantly greater cumulative survival compared with MVR [2]. Based on these results, mitral valve repair should be performed whenever possible, even in octogenarians.
Limitations
The present study has some limitations. It has the general limitations of a retrospective study. In addition, the number of patients was very small, and the total follow-up period in our patients was too short to have meaningful statistical analyses or to reach any definite conclusions, and a further study is recommended because of the heterogeneity of the patients in this study. Selection bias in favor of healthier patients by cardiologists and their subsequent referral to surgery could have skewed results toward better outcomes. Controlling for this bias would be difficult, because a large number of surgeons and cardiologists were involved in the care of these patients, and no information about patients who were not offered surgery was available. Nevertheless, most of these patients were of advanced NYHA functional class and had many other comorbidities, suggesting that this subgroup was not highly selected. Finally, the number of variables in the multivariable analyses was limited owing to statistical restrictions. The use of more covariates can sometimes lead to different conclusions.
Conclusions
Valve surgery can be performed in patients 80 years or older with acceptable mortality, good long-term results, and good quality of life. In our study, urgent operation, preoperative NYHA class IV, perioperative use of IABP and prolonged CPB time, in addition to preoperative renal dysfunction, had a significant effect on operative mortality. We believe that once a cardiac valve disease is diagnosed, early referral for surgery should help to avoid hazardous developments and consequently lead to better postoperative outcomes in patients aged 80 years or older.
References
Chappini B, Camurri N, Loforte A, Di Marco L, di Bartolomeo R, Marinell G (2004) Outcome after aortic valve replacement in octogenarians. Ann Thorac Surg 78:85–89
Nagendran J, Norris C, Maitland A, Koshal A, Toss DB (2005) Is mitral valve surgery safe in octogenarians? Eur J Cardiothorac Surg 28:83–87
Johnson WM, Smith JM, Woods SE, Hendy MP, Hiratsuka LF (2005) Cardiac surgery in octogenarians. Does age alone influence outcomes? Arch Surg 140:1089–1093
Langanay T, De Latour B, Ligier K, Derieux T, Agnino A, Verhoye J-P, Corbineau H, Chaperon J, Leguerrier A (2004) Surgery for aortic stenosis in octogenarians: influence of coronary disease and other comorbidities on hospital mortality. J Heart Valve Dis 13:545–553
Melby SJ, Zierer A, Kaiser SP, Guthrie TJ, Keune JD, Schuessler RB, Pasque MK, Lawton JS, Moazami N, Moon MR, Damiano RJ (2007) Aortic valve replacement in octogenarians: risk factors for early and late mortality. Ann Thorac Surg 83:1651–1657
Aoyagi S, Oryoji A, Nishi Y, Tanaka K, Kosuga K, Oishi K (1994) Long-term results of valve replacement with the St. Jude Medical valve. J Thorac Cardiovasc Surg 108:1021–1029
Carpentier A (1983) Cardiac valve surgery—the “French correction.”. J Thorac Cardiovasc Surg 86:323–337
Grossi EA, Zakow PK, Sussman M, Galloway AC, Delianides J, Baumann G, Colvin SB (2000) Late results of mitral valve reconstruction in the elderly. Ann Thorac Surg 70:1224–1226
Ngaage DL, Cowen ME, Griffin S, Guvendik L, Cale AR (2008) Are initial valve operations in octogenarians still high-risk in the current era? J Heart Valve Dis 17:227–232
DiGregorio V, Zehr KJ, Orszulak TA, Mullany CJ, Daly RC, Dearani JA, Schaff HV (2004) Results of mitral surgery in octogenarians with isolated nonrheumatic mitral regurgitation. Ann Thorac Surg 78:807–814
Kohl P, Kerzmann A, Honore C, Comte L, Limet R (2007) Aortic valve surgery in octogenarians: predictive factors for operative and long-term results. Eur J Cardiothorac Surg 31:600–606
Naagendran J, Norris C, Maitland A, Koshal A, Ross DB (2005) Is mitral valve surgery safe in octogenarians? Eur J Cardiothorac Surg 28:83–87
Bloomstein LZ, Gielchinsky I, Bernstein AD, Parsonnet V, Saunders C, Karanam R, Graves B (2001) Aortic valve replacement in geriatric patients: determinants of in-hospital mortality. Ann Thorac Surg 71:597–600
Anselmino M, Biondi-Zoccai G, Moretti C, Sheiban I (2008) Percutaneous coronary intervention on left main coronary artery trifurcation. Heart Vessels 23:279–281
Ricci M, Macedo FIB, Suarez MR, Brown M, Alba J, Salerno TA (2009) Multiple valve surgery with beating heart technique. Ann Thorac Surg 87:527–531
Logeais Y, Langanay T, Roussin R, Leguerrier A, Rioux C, Chaperon J, de Place C, Mabo P, Pony JC, Daubert JC, Laurent M, Almange C (1994) Surgery for aortic stenosis in elderly patients. A study of surgical risk and predictive factors. Circulation 90:2891–2898
Urso S, Sadaba R, Greco E, Pulitani I, Alvarez L, Juaristi A, Goiti JJ (2007) One hundred aortic valve replacements in octogenarians: outcomes and risk factors for early mortality. J Heart Valve Dis 16:139–144
Colli A, Verhoye J-P, Heijmen R, Strauch JT, Hyde JAJ, Pagano D, Antunes M, Koertke H, Ohri SK, Bail DHL, Leprince P, Van Straten BHM, Gherli T (2008) Antithrombotic therapy after bioprosthetic aortic valve replacement: ACTION registry survey results. Eur J Cardiothorac Surg 33:531–536
Armendi JI, Mestres C-A (2008) Antithrombotic therapy after bioprosthetic aortic valve replacement. Eur J Cardiothorac Surg 33:529–530
Gherli T, Colli A, Fragnito C, Nicolini F, Borrello B, Saccani S, D’Amico R, Beghi C (2004) Comparing warfarin with aspirin after biological aortic valve replacement: a prospective study. Circulation 110:496–500
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aoyagi, S., Fukunaga, S., Arinaga, K. et al. Heart valve surgery in octogenarians: operative and long-term results. Heart Vessels 25, 522–528 (2010). https://doi.org/10.1007/s00380-010-0009-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-010-0009-0