Abstract
The improvement of life expectancy created more surgical candidates with severe symptomatic aortic stenosis and age >80. Therefore, the main objective of this observational, retrospective single-centre study is to compare the long-term survival of octogenarians that have undergone surgical aortic valve replacement (AVR) to the survival of the general population of the same age and to establish whether any perioperative characteristics can anticipate a poor long-term result, limiting the prognostic advantage of the procedure at this age. From 2000 to 2014, 264 octogenarians underwent AVR at our institution. Perioperative data were retrieved from our institutional database and patients were followed up by telephonic interviews. The follow-up ranged between 2 months and 14.9 years (mean 4.1 ± 3.1 years) and the completeness was 99.2 %. Logistic multivariate analysis and Cox regression were respectively applied to identify the risk factors of in-hospital mortality and follow-up survival. Our patient population ages ranged between 80 and 88 years. Isolated AVR (I-AVR) was performed in 136 patients (51.5 %) whereas combined AVR (C-AVR) in 128 patients (48.5 %). Elective procedures were 93.1 %. Logistic EuroSCORE was 15.4 ± 10.6. In-hospital mortality was 4.5 %. Predictive factors of in-hospital mortality were the non-elective priority of the procedure (OR 5.7, CI 1.28–25.7, p = 0.02), cardiopulmonary bypass time (OR 1.02, CI 1.01–1.03, p = 0.004) and age (OR 1.36, CI 1.01–1.84, p = 0.04). Follow-up survival at 1, 4, 8 and 12 years was 93.4 % ± 1.6 %, 72.1 % ± 3.3 %, 39.1 % ± 4.8 % and 20.1 % ± 5.7 %, respectively. The long-term survival of these patients was not statistically different from the survival of an age/gender-matched general population living in the same geographic region (p = 0.52). Predictive factors of poor long-term survival were diabetes mellitus (HR 1.55, CI 1.01–2.46, p = 0.05), preoperative creatinine >200 μmol/L (HR 2.07, CI 1.21–3.53, p = 0.007) and preoperative atrial fibrillation (HR 1.79, CI 1.14–2.80, p = 0.01). In our experience, AVR can be safely performed in octogenarians. After a successful operation, the survival of these patients returns similar to the general population. Nevertheless, the preoperative presence of major comorbidities such as diabetes mellitus, renal dysfunction and atrial fibrillation significantly impact on long-term results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
According to the Italian National Institute of Statistics (ISTAT), the life expectancy of an 80-year-old man has reported to have increased from 5.8 to 8.1 years in the period 1974–2013 (ISTAT life tables at http://demo.istat.it/unitav2012/). Recent epidemiologic studies show that the prevalence of aortic stenosis in the octogenarian population can be as high as 9.8 % [1]. Therefore, the number of surgical candidates with severe symptomatic aortic stenosis with an age of 80 years or above has now become significant and is projected to steadily increase.
Transcatheter aortic valve implantation (TAVI) is an appealing alternative to the traditional surgical aortic valve replacement since it allows correction of aortic stenosis in a minimally invasive manner, without performance of sternotomy and institution of cardiopulmonary bypass. However, regardless of either of the techniques adopted to treat aortic stenosis, the perioperative risk is not negligible [2]. Needless to say, the recent update from the PARTNER Trial comparing AVR with TAVI in high risk, mostly octogenarian patients, depicts a 5-year survival that is similar but the incidence of moderate to severe paravalvular leaks is greater in TAVI compared to AVR to the tune of 14-fold [2].
Therefore, it is interesting to establish how the octogenarian performs during the long-term following a successful AVR and if any preoperative characteristic can anticipate a poor result.
Materials and methods
Study design
The primary end point of this retrospective, observational single-centre study is to evaluate the long-term survival of octogenarians who have undergone AVR at Circolo University Hospital, Varese, Italy and to compare this finding with the survival of an age/gender-matched general population living in the same geographic region (Lombardy), using data from the survival tables from the ISTAT. The secondary end point is to establish the predictive factors of poor long-term survival in this cohort.
Patients
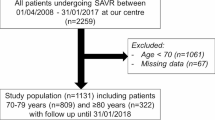
From January 2000 to August 2014, 2342 consecutive patients underwent AVR either as an isolated procedure or as a combined procedure at the Circolo University Hospital: 264 patients from the above-mentioned population were 80 years of age or above, the patient population included in this study. The perioperative clinical data of these patients were derived from our institutional database. The definitions of the variables present in our database were taken from the dataset of the Society of Cardiothoracic Surgery in Great Britain and Ireland (SCTS) Database version 3.8 [3]. No exclusion criteria were applied.
The TAVI programme commenced at Circolo University Hospital in June 2014. Only 2 patients underwent TAVI during the study period, significantly limiting the impact of the TAVI programme as a selection bias for this cohort. This study was approved by our local Ethics Committee (Protocol Number 0014502). All the internet addresses quoted in this manuscript were accessed last in September 2015.
Operative technique and postoperative care
All AVR procedures were performed through a median sternotomy. Cardiopulmonary bypass was instituted by cannulating the ascending aorta and using either a two-stage cannula or bicaval cannulation, according to the type of procedure (isolated or combined AVR). Antegrade and retrograde cold blood cardioplegia was routinely administered for myocardial protection. We approached the aortic valve most commonly through a transverse aortotomy.
Post-operatively, our patient cohort was commenced on warfarin therapy regardless of the type of aortic valve prosthesis implanted, unless there were specific contraindications to the use of warfarin. This was administered with a view of achieving a therapeutic international normalized ratio (INR) between 2.0 and 3.0. Those patients who underwent the implantation of a bioprosthesis were switched over from warfarin therapy to administration of 100 mg of aspirin therapy at 3 months post-operatively, unless they were on warfarin preoperatively or presented postoperatively persistent post-operative atrial fibrillation.
Follow-up
Follow-up was conducted by telephonic interviews. This was carried out to confirm each patient's status and the possible date of death. These telephone interviews were carried out between January and March 2015. Of the 252 patients that were discharged home, 250 were contactable whereas 2 were lost at the follow-up, hence a 99.2 % completeness. The duration of follow-up ranged between 2 months and 14.9 years (mean follow-up 4.1 ± 3.1 years).
Statistical analysis
Continuous variables were presented as mean ± standard deviation and compared using the unpaired t test. Categorical variables were presented as number and percentage and compared using Fisher’s exact test. p values ≤ 0.05 were considered statistically significant.
The analysis of the predictive factors for in-hospital mortality was performed using a logistic regression model: univariable analysis was used as screening method, inserting in the multivariable model only the variables that reached a p ≤ 0.10 at the univariable analysis.
Kaplan–Meier (KM) product limit method was used to calculate survival probability. All-cause mortality events were adopted for all KM curves presented in this study. KM curves were calculated twice, including in-hospital mortality (overall survival curve) and without in-hospital mortality (follow-up only survival curve). The log rank test was adopted to compare KM curves. Data on the survival of the patients living in Lombardy by age and sex were collected online from the publicly accessible National Institute of Statistics (ISTAT) website (http://demo.istat.it/unitav2012/).
The one-sample log rank test method described by Finkelstein and colleagues [4] and their own statistical package available online (http://hedwig.mgh.harvard.edu/biostatistics/node/30) were used to compare the survival of our patients with the expected survival of an age/sex-matched population.
The predictive factors of mortality during the follow-up were identified using Cox proportional hazard model: univariable analysis was used as a screening method inserting in the multivariable Cox model only the variables that reached a p ≤ 0.10 at the univariable analysis.
Stat-View 5.0 (SAS Institute Inc, Cary, NC) was used for all statistical calculations except the already referenced one-sample log rank test [4].
Results
In-hospital results
Preoperative characteristics are presented in Table 1: our patient population age ranged between 80 and 88 years. One hundred and thirty-six (51.5 %) patients underwent an isolated AVR (I-AVR) whereas 128 (48.5 %) patients underwent a combined AVR (C-AVR). I-AVR and C-AVR patients presented slightly different preoperative characteristics. C-AVR patients were younger but had a higher prevalence of ischemic heart disease (12.5 vs. 70.3 %, p < 0.0001) and extra-cardiac arteriopathy (13.2 vs. 22.7 %, p = 0.05). Consequently, they had significantly higher EuroSCOREs. As shown in Table 1, there was a minority of patients (17 patients, 12.5 % or I-AVR group) with an history of ischemic heart disease who did not undergo concomitant CABG, but an isolated aortic valve replacement: in fact they had either a previous CABG (3 patients) or a previous PCI (14 patients) and the preoperative coronary angiogram did not show any new coronary lesion requiring myocardial revascularization.
Intraoperative data are depicted in Table 2: 18 patients (6.8 %) underwent non-elective (urgent or emergency) procedures (I-AVR 4 patients, C-AVR 14 patients). In ten patients the primary diagnosis determining the non-elective status of the procedure was the aortic valve disease while in eight patients the aortic valve disease was a concomitant finding: 5 patients had infective endocarditis (1 I-AVR, 4 C-AVR), 5 presented with pulmonary oedema caused by aortic stenosis (3 I-AVR, 2 C-AVR), 7 C-AVR patients presented with acute coronary syndrome having a concomitant aortic stenosis and finally 1 C-AVR patient had a myxoma and concomitant aortic valve disease.
Thirteen patients (4.9 %) had redo procedures (five in the I-AVR and eight in the C-AVR group). Of these, five had previous CABG (3 I-AVR and 2 C-AVR patients), and the remaining eight had previous AVR: the causes of prosthesis explantation were notably bioprostheses degeneration (4 patients), paravalvular leak (2 patients), and prosthetic valve endocarditis (2 patients). Coronary artery bypass grafting (CABG) was the most commonly associated procedure amongst the C-AVR patients (61.7 %). All of the implanted AVR prostheses were stented. Additionally, all the patients underwent a bioprostheses implantation except one patient from the C-AVR group that underwent implantation of a mechanical valve. Sutureless aortic valve prostheses were still not available at our institution prior to the end of the study period. Hence, none of the patients had this type of rapid deployment valve implanted into them. Cardiopulmonary bypass and cross-clamp times were significantly longer in the C-AVR group.
Postoperative mortality and morbidities are reported in Table 3: whilst in-hospital mortality was reported to be 4.5 % (12 patients), there was no significant difference between the I-AVR and C-AVR groups (3.7 vs. 5.5 %, p = 0.56). No significant difference was noticed upon comparison of the postoperative complications between the two groups. However, the incidence of temporary continuous veno-venous hemofiltration (CVVH) was significantly higher in the C-AVR group (5.1 vs. 15.6 %, p = 0.007).
The postoperative incidence of cerebrovascular accidents (CVA) was 3 % (8 patients). Of these, 4 patients suffered a cerebrovascular accident or stroke with persistent neurological impairment and a computerized tomography (CT) of the brain positive for a new lesion whilst the remaining 4 had a transient ischemic attack that had completely resolved and with a negative CT of the brain.
In-hospital mortality of patients who underwent redo procedures was 15.3 % (2 deaths) versus 3.9 % for the ones undergoing first time surgery (10 deaths), but this difference was not statistically significant (p = 0.11).
Multivariate analysis identified three significant predictive factors of in-hospital mortality. These were non-elective priority of the procedure (urgent or emergency) (OR 5.7, CI 1.28–25.7, p = 0.02), the duration of cardiopulmonary bypass (OR 1.02, CI 1.01–1.03, p = 0.004) and age (OR 1.36, CI 1.01–1.84, p = 0.04). Previous cardiac surgery was found to have an OR of 4.38 with a quasi-significant p value (0.08), but when inserted into the multivariate model it lost significance. The full univariate and multivariate regression models are presented in Appendix A.
Follow-up results
The 12-year survival including in-hospital mortality of octogenarians who underwent AVR at 1, 4, 8 and 12 years was 89.1 % ± 1.9 %, 68.8 % ± 3.3 %, 37.3 % ± 4.7 % and 19.2 % ± 5.5 %, respectively. The 12-year survival excluding in-hospital mortality, therefore, of patients who survived surgery at 1, 4, 8 and 12 years was, instead, 93.4 % ± 1.6 %, 72.1 % ± 3.3 %, 39.1 % ± 4.8 % and 20.1 % ± 5.7 %. In Fig. 1, the latter KM curve was compared with the expected survival of an age/gender-matched population living in the same geographical area, achieving very similar result: in fact, the expected survival of the general population at 1, 4, 8 and 12 years was 92.9 %, 70.1 %, 42.2 % and 20.7 %, respectively. Furthermore, the one-sample log rank test comparing the two curves returned a p value of 0.52. No patient in this series underwent any cardiac reintervention during the follow-up.
The follow-up survival in I-AVR and C-AVR groups was not significantly different (I-AVR 1 year 96 % ± 1.8 %, 4 year 71.9 % ± 4.7 %, 8 year 34.7 % ± 6.8 %, 12 year 22.3 % + 8.5 % and C-AVR 1 year 90.5 % ± 2.7 % 4 year 72.2 % + 4.7 %, 8 year 42.6 % + 6.8 %, 12 year 19.3 % + 6.8 %, p = 0.90).
Diabetes Mellitus (HR 1.55, CI 1.01–2.46, p = 0.05), preoperative creatinine >200 μmol/L (HR 2.07, CI 1.21–3.53, p = 0.007) and preoperative atrial fibrillation (HR 1.79, CI 1.14–2.80, p = 0.01) were independent predictive factors of 12-year follow-up survival. The univariate and multivariate Cox model is presented in Appendix B.
The respective 12-year survival curves according to the presence of these three preoperative risk factors (atrial fibrillation, preoperative diabetes mellitus and preoperative creatinine of >200 μmol/L) are demonstrated in Figs. 2, 3 and 4.
Discussion
In 1968, Ross and Braunwald showed that the survival of medically managed patients with symptomatic aortic stenosis was 50 % in a period between 2 and 5 years according to what the presenting symptoms were [5]. In 2015, the latest update of the PARTNER Trial comparing TAVI to medical treatment in inoperable patients demonstrated that the 5-year mortality of a cohort of patients (mean age 83 years, STS score 11.7 %) with severe symptomatic aortic stenosis managed medically is 93 % [6]. This would confirm that, despite the advances and the optimization of medical management during the last 40 years, the prognosis of these high-risk patients is still very poor if managed medically alone.
Several studies have been published during the last few years on the short- and mid-term results of isolated AVR and combined AVR in octogenarians, demonstrating an in-hospital mortality that ranges between 0 and 13 % [7, 8]. Our results are within the lower half of this range (3.7 % for I-AVR and 5.5 % for C-AVR) but in line with the recent results on octogenarians from other regional cardiac surgery databases (Reggio Emilia Regional Database, RERIC) although the maximum length of the follow-up reported in this registry was significantly shorter than our series [9].
Despite the in-hospital mortality that we reported being similar when comparing I-AVR and C-AVR, the length of cardiopulmonary bypass, reflecting the straightforwardness of the procedure, was found to be a predictive factor of in-hospital mortality together with the non-elective priority of the procedures. Additionally, age was identified amongst the predictive factors of in-hospital mortality despite the tight range of ages represented in this study (80–88 years). Both simple and logistic EuroSCOREs overestimated the observed operative mortality and were, therefore, not predictive of mortality in octogenarians undergoing AVR. The scarce predictive value of EuroSCORE in octogenarians undergoing AVR was already demonstrated by Leontyev who explained this result outlining that the initial versions (EuroSCORE and logistic EuroSCORE) were in fact modelled on CABG patients [10]. EuroSCORE II seems, instead, to be a more promising tool for a correct risk assessment of octogenarians undergoing AVR, with an area under the curve (AUC) of 0.72 [11].
Our series reports one of the longest follow-ups available in the literature for octogenarians who have undergone aortic valve replacement [7, 8]. The ultimate survival of the entire population at 12 years from the operation was quite low (20.1 ± 5.7 %). However, this was found to be similar to the expected survival of an age/gender-matched population living in Lombardy (Fig. 1). Our survival curve is also similar to the one reported by the Italian Regional Cardiac Surgery Registry [9] that shows a 6-year survival, of octogenarians who have undergone AVR, of 67.5 vs. a 60.7 % survival in our series during the same timeframe.
In our opinion, the similarity between the survival of the general population and patients who have undergone aortic valve replacement is one of the most interesting findings of the study since the same principle does not apply to younger patients.
In fact, Bouhout and co-workers recently published a retrospective series with an analysis designed similar to the one performed in our study. Their series included 450 patients with age ≤65 years who had undergone AVR, demonstrating that 10-year survival of these patients is significantly lower than an age/gender-matched general population [12], This finding is also consistent with another study by Kvidal and co-workers who reported a 4.5 times excess mortality in patients who had undergone AVR, aged <50, when compared with same age general population [13].
In patients who have undergone AVR, valve-specific complications such as haemorrhagic and thrombo-embolic events, prosthetic valve endocarditis or structural dysfunction may all play an important role in the survival difference with the general population, but in the octogenarian population this difference seems to be less obvious [12].
Two possible mechanisms may explain, in our opinion, this phenomenon. The first and most relevant one is that the mortality per year and consequently the burden of concomitant medical morbidity in the general population aged ≥80 years is fairly significant. ISTAT reports a probability of death per year between 5.7 and 14.1 % for men with an age ranging between 80 and 88 years versus a range between 0.1 and 1.1 % for men aged between 40 and 65 years (ISTAT life tables at http://demo.istat.it/unitav2012/).
The second factor possibly influencing this result could be also the slower bioprosthetic degeneration rates and, therefore, the higher freedom from bioprostheses explantation in the elderly when compared to younger patients as demonstrated by Banbury and co-workers [14].
From this point of view, AVR in octogenarians appears to be a much more efficient procedure than in the younger patients restoring a “back to normal” patient life expectancy.
In this series, three very common preoperative comorbidities as diabetes mellitus, renal dysfunction and atrial fibrillation were found to be predictive of a worse long-term survival. Each of these three preoperative comorbidities are well-known risk factors for the long-term survival in the general population and, therefore, we believe they could possibly impact on survival independently from the diagnosis of aortic stenosis and the occurrence of AVR [15–17]: renal dysfunction, and particularly end-stage renal dysfunction has been demonstrated as a strong risk factor for long-term survival especially in the subgroup of patients undergoing other than CABG procedures [18].
Nevertheless, none of these factors should completely nullify the prognostic advantage achieved from the correction of the aortic stenosis. In our series, the 5-year survival for the octogenarian with atrial fibrillation was 61.3 ± 7.5 %, with diabetes mellitus was 54.2 ± 8.2 % and with a preoperative creatinine >200 μmol/L was 45.5 ± 10 % as depicted in Figs. 2, 3 and 4, respectively. These survival figures appear better than a 93 % mortality at 5 years for patients with aortic stenosis managed medically as shown in the PARTNER Trial [6].
The two main limitations of this study are the retrospective design and the lack of randomization towards conservative treatment, TAVI or alternatively sutureless aortic valve prostheses: the latter type of prosthesis could be a promising device for the octogenarian since it has been recently proven to outperform TAVI in terms not only of in-hospital mortality, paravalvular regurgitation rates and postoperative pacemaker requirements [19].
Nevertheless, given the absence of TAVI as a management option at Circolo University Hospital during nearly all of the study period, these results are unbiased, due to the lack of possibility to refer high-risk patients for TAVI, with a consequent improvement of the risk profile and a mitigation of in-hospital mortality and morbidity in the surgical patients. On the other hand, it is not possible to quantify the number of patients considered inoperable and, therefore, destined to medical management during the same timeframe.
In conclusion, this study has confirmed that both I-AVR and C-AVR can be performed with relatively low risk in the octogenarian, particularly when in an elective setting. Following a successful operation, the long-term survival of these patients returns nearly identical to the general population of the same age. Pre-existing comorbidities such as diabetes mellitus, renal dysfunction or atrial fibrillation significantly impact on long-term prognosis as they reduce, but not completely nullify, the prognostic advantage achieved by the correction of severe aortic stenosis in this age group.
References
Eveborn GW, Schirmer H, Heggelund G, Lunde P, Rasmussen K (2013) The evolving epidemiology of valvular aortic stenosis. the tromsø study. Heart 99:396–400
Mack MJ, Leon MB, Smith CR, Miller DC, Moses JW, Tuzcu EM, Webb JG, Douglas PS, Anderson WN, Blackstone EH, Kodali SK, Makkar RR, Fontana GP, Kapadia S, Bavaria J, Hahn RT, Thourani VH, Babaliaros V, Pichard A, Herrmann HC, Brown DL, Williams M, Akin J, Davidson MJ, Svensson LG, PARTNER 1 trial investigators (2015) 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385(9986):2477–2484
Bridgewater B, Keogh BE, Kinsman R, Walton P (2009) The society for cardiothoracic surgery in Great Britain & Ireland: the sixth national adult cardiac surgical database report. Dendrite Clinical Systems Ltd., Henley-on-Thames, pp 486–493
Finkelstein DM, Muzikansky A, Schoenfeld DA (2003) Comparing survival of a sample to that of a standard population. J Natl Cancer Inst 95:1434–1439
Ross J Jr, Braunwald E (1968) Aortic stenosis. Circulation 38:61–67
Kapadia SR, Leon MB, Makkar RR, Tuzcu EM, Svensson LG, Kodali S, Webb JG, Mack MJ, Douglas PS, Thourani VH, Babaliaros VC, Herrmann HC, Szeto WY, Pichard AD, Williams MR, Fontana GP, Miller DC, Anderson WN, Akin JJ, Davidson MJ, Smith CR, PARTNER trial investigators (2015) 5-year outcomes of transcatheter aortic valve replacement compared with standard treatment for patients with inoperable aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385(9986):2485–2491
Vasques F, Lucenteforte E, Paone R, Mugelli A, Biancari F (2012) Outcome of patients aged ≥80 years undergoing combined aortic valve replacement and coronary artery bypass grafting: a systematic review and meta-analysis of 40 studies. Am Heart J 164:410–418
Vasques F, Messori A, Lucenteforte E, Biancari F (2012) Immediate and late outcome of patients aged 80 years and older undergoing isolated aortic valve replacement: a systematic review and meta-analysis of 48 studies. Am Heart J 163:477–485
Di Eusanio M, Fortuna D, Cristell D, Pugliese P, Nicolini F, Pacini D, Gabbieri D, Lamarra M, RERIC (Emilia Romagna Cardiac Surgery Registry) Investigators (2012) Contemporary outcomes of conventional aortic valve replacement in 638 octogenarians: insights from an Italian Regional Cardiac Surgery Registry (RERIC). Eur J Cardiothorac Surg 41:1247–1252
Leontyev S, Walther T, Borger MA, Lehmann S, Funkat AK, Rastan A, Kempfert J, Falk V, Mohr FW (2009) Aortic valve replacement in octogenarians: utility of risk stratification with EuroSCORE. Ann Thorac Surg 87(5):1440–1445
Vanhuyse F, Maureira P, Folliguet T, Villemot JP (2013) Predictive value of five risk scores to predict outcomes after aortic valve replacement in octogenarians. J Heart Valve Dis 22:517–523
Bouhout I, Stevens LM, Mazine A, Poirier N, Cartier R, Demers P, El-Hamamsy I (2014) Long-term outcomes after elective isolated mechanical aortic valve replacement in young adults. J Thorac Cardiovasc Surg 148:1341–1346
Kvidal P, Bergström R, Hörte LG, Ståhle E (2000) Observed and relative survival after aortic valve replacement. J Am Coll Cardiol 35:747–756
Banbury MK, Cosgrove DM, White JA, Blackstone EH, Frater RW, Okies JE (2001) Age and valve size effect on the long-term durability of the Carpentier-Edwards aortic pericardial bioprosthesis. Ann Thorac Surg 72:753–757
Lip GY, Clementy N, Pericart L, Banerjee A, Fauchier L (2015) Stroke and major bleeding risk in elderly patients aged ≥75 years with atrial fibrillation: the Loire Valley atrial fibrillation project. Stroke 46:143–150
Leal J, Gray AM, Clarke PM (2009) Development of life-expectancy tables for people with type 2 diabetes. Eur Heart J 30:834–839
Warnock DG, Muntner P, McCullough PA, Zhang X, McClure LA, Zakai N, Cushman M, Newsome BB, Kewalramani R, Steffes MW, Howard G, McClellan WM, Investigators REGARDS (2010) Kidney function, albuminuria, and all-cause mortality in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. Am J Kidney Dis 56:861–871
Nicolini F, Fragnito C, Molardi A, Agostinelli A, Campodonico R, Spaggiari I, Beghi C, Gherli T (2011) Heart surgery in patients on chronic dialysis: is there still room for improvement in early and long-term outcome? Heart Vessels 26:46–54
Biancari F, Barbanti M, Santarpino G, Deste W, Tamburino C, Gulino S, Immè S, Di Simone E, Todaro D, Pollari F, Fischlein T, Kasama K, Meuris B, Dalén M, Sartipy U, Svenarud P, Lahtinen J, Heikkinen J, Juvonen T, Gatti G, Pappalardo A, Mignosa C, Rubino A (2015) Immediate outcome after sutureless versus transcatheter aortic valve replacement. Heart Vessels. doi:10.1007/s00380-014-0623-3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cappabianca, G., Ferrarese, S., Musazzi, A. et al. Predictive factors of long-term survival in the octogenarian undergoing surgical aortic valve replacement: 12-year single-centre follow-up. Heart Vessels 31, 1798–1805 (2016). https://doi.org/10.1007/s00380-016-0804-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-016-0804-3