Abstract
Purpose
Thulium:YAG (Tm:YAG) vaporesection has been introduced and efficiency was shown on smaller prostates. Criticism mainly referred to prolonged operation time in larger prostates, which appears to be a potential limitation compared to HoLEP. Aim of the study was to evaluate feasibility and efficiency of Tm:YAG VapoEnucleation in larger prostates.
Methods
VapoEnucleation was performed using a 70 W continuous wave-laser. After enucleation tissue was morcellated within the bladder. Prospectively assessed outcomes were improvement in urodynamic parameter and the intra- and postoperative course. Complications were recorded.
Results
A total of 88 consecutive patients with prostatic enlargement underwent VapoEnucleation. Prostatic volume was 61.3 ± 24.0 cc (30–160). OR-time was 72 min ± 26.6 (35–144) and laser-time 32.4 ± 10.1 min (16.3–59.3). Applied laser energy was 123.7 ± 40.6 kJ (67.8–240.9). An average of 31.7 ± 18.3 g of tissue was retrieved. Pathology revealed four patients with incidental carcinoma. Foley catheter-time was 2 days and the suprapubic tube, if placed, was removed on the third postoperative day on average. Twelve complications were recorded, including bleeding (3), urinary tract infection (6), second-look procedure, due to insufficient deobstruction (2). Re-catherization after successful initial voiding trial was necessary in one patient. Mean peak flow rate improved from 3.5 ± 4.7 to 19.8 ± 11.6 ml/s and post-voiding residual urine decreased from 121.4 ± 339.9 to 22.4 ± 32.7 ml.
Conclusion
The functional outcomes demonstrate efficiency of Tm:YAG VapoEnucleation for patients with larger prostates. From our experience, learning curve in VapoEnucleation is short and complications are minimal. Theoretically, no limitation in prostate size occurs. Long-term follow-up is needed to prove durability.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Purpose
Thulium:YAG (Tm:YAG) vaporesection (simultaneous resection of TUR-P like chips and vaporization of tissue) has recently been introduced for the treatment of benign prostatic obstruction (BPO). The efficacy and safety of the procedure was shown on prostates with smaller volume [1, 2]. However, one main point of criticism and possible pitfall of this method is the prolonged operation time in patients with large volume prostates, which still may require open simple prostatectomy or staged TUR-P. This could be interpreted as a potential disadvantage of the Thulium:YAG laser prostatectomy compared with previously introduced Holmium:YAG laser enucleation of the prostate (HoLEP).
With rising efficacy of medical treatment, such as alpha-blockers surgical treatment is postponed and more patients with larger prostates appear at the point of treatment [3]. Therefore any surgical therapy, trying to compete with standard TUR-P needs to be able to offer sufficient treatment to any patient indepent from the volume of the prostate.
Aim of the current study was to evaluate the feasibility and efficiency of Tm:YAG enucleation (VapoEnucleation), like in HoLEP as transurethral pendant to open simple prostatectomy in patients with larger prostates.
Methods
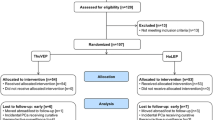
This prospective non-randomized study included our first 88 consecutive patients undergoing VapoEnucleation of the prostate with the 70 W 2 Micron cw Tm:YAG laser (RevoLix®, LISA Laser products, Katlenburg, Germany) using a 550 micron optical core bare-ended, re-usable laser fiber (RigiFib®, LISA Laser products, Katlenburg, Germany). Surgery was perfomed with a 26 Fr. continuous-flow laser resectoscope (Richard Wolf, Knittlingen, Germany) and a mechanical tissue Morcellator in combination with a morcescope (Piranha® Richard Wolf, Knittlingen, Germany). All interventions were carried out using normal saline as irrigation fluid.
Before surgery, the patients went through detailed urological examination, including transrectal ultrasound (TRUS), digital rectal examination (DRE), assessment of the international prostate symptom score (IPSS) and quality of life score (QoL) as well as the international index of erectile function questionnaire (IIEF-5). Measurement of serum prostate-specific antigen (PSA) and urine analysis was carried out before digital rectal examination and instrumentation was included. In patients with suspect age-specific PSA values or suspect DRE a 12-core needle biopsy of the prostate was carried out. High-risk patients with a history of negative biopsy were councilled to undergo saturation biopsy prior to surgery. Furthermore, post-voiding residual urine (PVR) and mean urinary peak flow rate (Qmax) were reviewed. Indications for surgery were refractory urinary obstruction and indwelling catheter. In addition patients with symptomatic lower urinary tract symptoms (LUTS) were included. Inclusion criteria were Qmax <15 ml/s and IPSS >7. Patients with urodynamically diagnosed neurogenic bladder or know cancer of the prostate were excluded. All laser surgeries were performed by three surgeons.
The technique of VapoEnucleation was similar to the previously described three lobe technique in HoLEP [4]. In a few words, we start the procedure with the marking of the distal resection border close to the apex of the prostate. After performing Turner–Warwick like incisions at 5 and 7o’ clock positions to the surgical capsule down to the previously marked area, we enucleate the entire median lobe. In the following, the first lateral lobe and consequently the second lateral lobe is enucleated and positioned into the bladder for morcellation. The procedure is carried out, using normal saline as irrigation fluid. After finishing the procedure a three-way Foley catheter (22 or 24 French) is placed into the bladder and intermittent or continuous irrigation is provided over night.
A suprapubic tube was placed, either for the purpose of low pressure resection, like in TUR-P and then used for continuous suction during the procedure or in patients with heavily trabeculated bladder and a history of recurrent urinary retention, who may need prolonged time to recover to sufficient voiding postoperatively.
Assessed outcomes were improvement in urodynamic parameter, such as mean peak flow rate (Qmax) and post-voiding residual urine (PVR) as well as the intra- and postoperative course. Complications were recorded. Statistical analysis was performed using Statistical Package for Social Sciences, version 8.0 for Windows (SPSS, Chicago, IL) analytical software. Improvement in Qmax and PVR was calculated using paired samples T test. P < 0.05 was considered statistically significant.
Results
A total of 88 patients with benign prostatic enlargement underwent VapoEnucleation. The mean age was 71.35 ± 8.3 years. Mean preoperative prostatic volume, as measured by transrectal ultrasound (TRUS) was 61.3 ± 24.0 cc (range 30–160 cc). The baseline characteristics of the patients and indications for performing surgery are specified in Table 1.
A total of 30.7% of the patients suffered recurrent urinary retention and had been placed on indwelling urinary catheter prior to surgery, 69.3% of the patients presented with BPO and dissatisfaction with medical treatment.
Mean total operative time, including cystoscopy, enucleation and morcellation was 72 ± 26.6 min (35–144) and laser-time 32.4 ± 10.2 min (16.3–59.3), respectively. Average amount of applied laser energy was 123.7 kJ ± 40.6 (67.8–240.9). An average of 31.7 ± 18.3 g of tissue was retrieved. Here, it has to be kept in mind, that tissue retrieval is underestimated, due to the significant amount of vaporization during the procedure. Giving the procedure a higher volume reduction than the amount of retrieved tissue might suggest. The average Foley catheter-time was 2.1 days and the suprapubic tube, if placed, was removed on the third postoperative day on average. Patients were routinely discharged the day after catheter removal. Three patients (4.2%) were discharged with suprapubic tube in place, since PVR decreased slowly in these patients. All of those, discharged with a suprapubic tube had refractory urinary retention prior to surgery. Operative parameters and postoperative course are summarized in Table 2.
Pathological assessment revealed four patients with incidental adenocarcinoma of the prostate. Total Gleason-Score was 4 or 5 in three patients (two of them chose for radical retropubic prostatectomy, one for active surveillance), one patient (87 years) with a Gleason-Score of 8 underwent androgen deprivation therapy.
Pre- and postoperative blood sodium-measurement showed no statistical significant difference (138 ± 2.6 vs. 137 ± 2.4 mmol/l, P = 0.150).
Complications were recorded in 12 patients (16.6%) during the immediate and short-term postoperative course, including intra- or postoperative bleeding in three patients (3.4%), symptomatic urinary tract infection in six patients (6.8%) and second-look procedure during the same hospital stay, due to incapability to void in two patients (2.2%). One patient required re-catheterization due to urinary tract infection 2 weeks postoperatively. Two of the patients with intra-or postoperative bleeding required blood transfusions (2.2%).
Improvement in Qmax and decrease in PVR was statistically significant. The preoperative peak urinary flow rate improved from 3.5 ± 4.7 to 19.8 ± 11.6 ml/s (P < 0.001) at discharge and post-voiding residual urine decreased from 121.4 ± 339.9 to 22.4 ± 32.7 ml (P = 0.03) at the day of discharge.
To compare efficacy of VapoEnucleation also in larger prostates, two groups of patients with have been formed. Patients with a prostatic volume of more 60 cc or more where considered large and the peri- and postoperative outcome was compared to patients with a prostatic volume below 60 cc. As expactable, the total OR-time as well as the total laser-time was longer in the group with larger prostates. However, comparing the peri- and postoperative outcome, no statistical differences could be found between both subgroups, showing deobstruction also in patients with larger prostates. The results are displayed in Table 3.
Discussion
Benign prostatic obstruction is one of the most frequent symptoms in daily urologic practice. Established treatment options include transurethral resection of the prostate (TUR-P) using electric current or open simple prostatectomy in larger prostates are well established. However, both methods are associated with relevant morbidity. Open simple prostatectomy, although well known as effective and durable treatment option in BPO is related with significant morbidity and even mortality. Complication rates of 15% in recent series of open prostatectomy are reported. The authors report rates of severe bleeding in approximately 12% of the patients with transfusion rates above 8.2%. Postoperative sepsis was reported to occur in up to 8.6% of the patients undergoing open simple prostatectomy [5]. Transfusion rates up to 26.5% are reported [6].
Another pitfall of open simple prostatectomy is the prolonged catheter-time and consecutively the prolonged time of hospital stay. Catheterization times of 7 days are reported [5].
Therefore alternative treatment options have been introduced. Laser-based treatment modalities promise significant release of obstructive symptoms combined with decreased morbidity. Previously introduced Holmium:YAG laser prostatectomy has been studied intensively. Holmium laser enucleation of the prostate (HoLEP) offers treatment to BPO patients with all sizes of prostatic enlargement. HoLEP, as first described by Gilling et al. [7], is the retrograde transurethral pendant to antegrad open simple prostatectomy. Comparable to the open technique, the enlarged tissue is removed from the pseudocapsule between central and peripheral zone of the prostate and then mechanically morcellated in the bladder. Recently 6-year follow-up results could be published by the group of Gilling. Those patients available for follow-up showed durability in Qmax improvement and sufficient rise in the quality of life and decrease in IPSS. The vast majority (92%) reported satisfaction with the operative result [8]. Catheter times of 1.3 days are reported, which is considerable shorter than in open techniques [3]. Also the rate of blood transfusions is lower, with only 1.3% as reported by Elzayat et al. in the same publication. This data may lead to the conclusion that laser prostatectomy offers efficient treatment of benign prostatic enlargement with a relevant decline in complications simultaneously. However, to date HoLEP only has been established in specified centres around the world, which may be due to the prolonged learning curve of this technique and the prolonged operative time compared to TUR-P or open prostatectomy [9, 10].
Recently introduced Thulium:YAG prostatectomy, using the technique of VapoResection showed efficient and safe relief of symptoms related to benign prostatic obstruction in men with small and medium sized prostates [1]. VapoResection means combination of resection and vaporization of tissue. By combination of these two techniques the operative time of the procedure is reduced [1]. Nevertheless, main criticism passed on the technique of VapoResection was the potential limitation to smaller prostatic glands due to the prolonged operation time in larger prostates, especially when compared to open simple prostatectomy or HoLEP of the prostate. Therefore we assessed to ability to perform a transurethral enucleation technique (VapoEnucleation), like in HoLEP, with the Thulium:YAG laser as well, to dissolve this possible pitfall.
In contrast to the pulsed Ho:YAG laser, the energy of the Thulium:YAG laser is delivered in a continuous wave mode and offers a high ablation capacity combined with an excellent hemostasis [11]. The incision in tissue is clear and smooth. Thereby the surgeon is able to cut at the desired point and is not as depended to find the exact layer of the surgical capsule between adenoma and peripheral zone as surgical pathway at the very beginning of the procedure. This may lead to a significantly steeper learning curve [12], since the surgeon has the ability to correct the layer of resection during the procedure. However, the complete enucleation of the adenoma at the surface of the surgical pseudocapsule remains the goal of the procedure also in VapoEnucleation.
This study presents the first results on Tm:YAG VapoEnucleation, showing significant short-term relieve of obstructive symptoms in patients with symptomatic benign prostatic obstruction. The preliminary surgical results are comparable to those reported in HoLEP [8, 13] although the initial learning curve of implementing a new technique is included in the reported 88 patients. Reported complications were minor within the immediate and short-term peri- and postoperative period. Urinary tract infections were accounting for 50% of the occurring complications. Bleeding complications and transfusion rate are considerably lower than in open prostatectomy offering the patient increased safety. With the introduction of VapoEnucleation virtually no size limit occurs in treating symptomatic BPO with the Thulium:YAG laser. However, although feasibility could be shown by the above presented results, further follow-up will be needed, to also proof improvement in symptoms, as measured with IPSS and long-term reduction of prostatic volume.
Conclusion
The immediate functional outcomes demonstrate efficacy of Tm:YAG VapoEnucleation. From our experience learning curve in VapoEnucleation seems short and associated complications are minimal. Technically no limitation in prostatic size occurs, allowing to treat also patients with large prostates endoscopically with this laser device. Long-term follow-up is needed, to prove durability of these promising results.
References
Bach T, Herrmann TR, Ganzer R, Burchardt M, Gross AJ (2007) RevoLix vaporesection of the prostate: initial results of 54 patients with a one year follow-up. World J Urol 25:257–262. doi:10.1007/s00345-007-0171-x
Xia SJ, Zhuo J, Sun XW, Han BM, Shao Y, Zhang YN (2008) Thulium laser versus standard transurethral resection of the prostate: a randomized prospective trial. Eur Urol 53:382–389. doi:10.1016/j.eururo.2007.05.019
Elzayat EA, Elhilali MM (2005) Holmium laser enucleation of the prostate (HoLEP): the endourologic alternative to open prostatectomy. Eur Urol 49:87–91. doi:10.1016/j.eururo.2005.08.015
Gilling P (2008) Holmium laser enucleation of the prostate (HoLEP). BJU Int 101:131–142
Serretta V, Morgia G, Fondacaro L, Curto G, Lo Bianco A, Pirritano D et al (2002) Open prostatectomy for benign prostatic enlargement in southern Europe in the late 1990s: a contemporary series of 1800 interventions. Urology 60:623–627. doi:10.1016/S0090-4295(02)01860-5
Mearini E, Marzi M, Mearini L, Zucchi A, Porena M (1998) Open prostatectomy in benign prostatic hyperplasia: 10-year experience in Italy. Eur Urol 34:480–485. doi:10.1159/000019787
Gilling PJ, Kennett K, Das AK, Thompson D, Fraundorfer MR (1998) Holmium laser enucleation of prostate (HoLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J Endourol 12:457–459
Gilling PJ, Aho TF, Framptom CM, King CJ, Fraundorfer MR (2008) Holmium laser enucleation of the prostate: results at 6 years. Eur Urol 53:744–749. doi:10.1016/j.eururo.2007.04.052
Elzayaz EA, Elhilali MM (2006) Laser treatment of symptomatic benign prostatic hyperplasia. World J Urol 24:410–417. doi:10.1007/s00345-006-0063-5
Seki N, Mocida O, Kinukawa N, Sagiyama K, Nato S (2003) Holmium laser enucleation for prostatic adenoma: analysis of learning curve over the curse of 70 consecutive cases. J Urol 170:1847–1850. doi:10.1097/01.ju.0000092035.16351.9d
Wendt-Nordahl G, Huckele S, Honeck P, Alken P, Knoll T, Michel MS, Häcker A (2008) Systemic evaluation of a recently introduced 2-micron contiuous-wave laser for vaporesection of the prostate. J Endourol 22:1041–1045. doi:10.1089/end.2007.0421
Bach T, Igelmann HerrmannTRW, Ganzer R, Gross AJ (2008) Thulium:YAG vaporesection of the prostate: expert versus novice-functional outcome. Eur Urol Suppl 7:203. doi:10.1016/S1569-9056(08)60528-X Abstract 532
Vavassori I, Hurle R, Vismara A, Manzetti A, Valenti S (2004) Holmium laser enucleation of the prostate combined with mechanical morcellation: two years of experience with 196 patients. J Endourol 18:109–112. doi:10.1089/089277904322836767
Conflict of interest statement
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bach, T., Wendt-Nordahl, G., Michel, M.S. et al. Feasibility and efficacy of Thulium:YAG laser enucleation (VapoEnucleation) of the prostate. World J Urol 27, 541–545 (2009). https://doi.org/10.1007/s00345-008-0370-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-008-0370-0