Abstract
Purpose
We compared the perioperative and postoperative characteristics of thulium vapoenucleation and holmium laser enucleation of the prostate for the treatment of large volume benign prostatic hyperplasia.
Materials and methods
A total of 94 patients with benign prostatic hyperplasia and a median prostate size of 80 (IQR 46.75–100) cc were either randomized to thulium vapoenucleation or holmium laser enucleation of the prostate. Patients were assessed preoperatively, 1 and 6 months postoperatively.
Results
The median operative time was 60 (IQR 41–79) min without significant differences between the groups. There were no significant differences between the groups regarding catheter time [2 (IQR 2–2) days] and postoperative stay [2 (IQR 2–3) days]. Clavien 1 (13.8%), 2 (3.2%), 3a (2.1%), and Clavien 3b (4.3%) complications occurred without significant differences between the groups. At 6-month follow-up, median maximum flow rate (10.7 vs. 25.9 ml/s), post-void residual urine (100 vs. 6.5 ml), I-PSS (20 vs. 5), quality of life (4 vs. 1), PSA (4.14 vs. 0.71 µg/l), and prostate volume (80 vs. 16 ml) had improved significantly (p < 0.001) compared to baseline without significant differences between the groups. Median PSA decrease was 79.7% (58.8–90.6%) and prostate volume reduction was 74.5% (68.57–87.63%) without differences between the groups. The reoperation rate was zero at 6-month follow-up.
Conclusions
Thulium vapoenucleation and holmium laser enucleation of the prostate are safe and effective procedures for the treatment of large volume benign prostatic hyperplasia. Both procedures give satisfactory micturition improvement with low morbidity and sufficient prostate volume reduction at 6-month follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although associated with considerable perioperative complications like severe bleeding, open prostatectomy (OP) has been the standard treatment of substantially enlarged prostates over decades [1]. Since the introduction of the holmium laser enucleation of the prostate (HoLEP) into the armamentarium of benign prostatic obstruction (BPO) treatment [2], HoLEP has been proven to be a minimally invasive, size-independent method in numerous randomized controlled trials (RCTs) with excellent long-term results [3]. Alternative procedures for endoscopic enucleation of the prostate (EEP) mimicking the HoLEP technique have been described during the past 10 years using different types of energy sources [4]. HoLEP has been recommended by the current guidelines of the European Association of Urology in men with substantially enlarged prostates (e.g. > 80 cc) as first choice [5]. However, only few RCTs for EEP procedures other than HoLEP [3] or bipolar enucleation of the prostate (BipolEP) [6,7,8,9,10] for the treatment of large volume prostates are available: greenlight laser enucleation of the prostate (GreenLEP) [11], diode laser enucleation of the prostate (DiLEP) [10] and thulium laser enucleation of the prostate (ThuLEP) [12], respectively. The latter is a transurethrally performed enucleation technique using the beak of the resectoscope for dissecting the adenoma from the pseudocapsule of the prostate with Tm:YAG laser support [12]. In contrast, the Tm:YAG laser is continuously applied to the layer of enucleation for dissecting the adenoma from the surgical pseudocapsule in thulium vapoenucleation of the prostate (ThuVEP) [13]. ThuVEP has been shown to be a size-independent procedure for the surgical treatment of BPO with low perioperative morbidity and good long-term results [13,14,15]. To our knowledge, we present the first RCT comparing the perioperative and postoperative characteristics of ThuVEP with HoLEP in patients with large volume prostates during a short-term 6-month follow-up.
Methods
Study design and enrollment
After receiving institutional review board approval, patients were recruited between January 2015 and February 2016. This RCT was registered in the German clinical trials register (DRKS-ID: DRKS00008206). Inclusion criteria were a maximum urinary flow rate (Qmax) ≤ 15 ml/s, International prostate symptom score (I-PSS) ≥ 12, patients ≥ 18 years, patients with failed medical therapy of BPO, recurrent urinary tract infections (UTI), and patients with acute or recurrent episodes of urinary retention or postrenal acute kidney injury. Exclusion criteria were previous urethral/prostatic surgery, active prostate cancer (PCa) or urethral strictures, and urodynamically diagnosed neurogenic bladder.
Randomization and preoperative assessments
Patients were randomized to one of the two groups by a computer-based prospective random sequence generator in a 1:1 ratio. Preoperative assessment included a physical examination with digital rectal examination (DRE), transrectal ultrasound (TRUS) and biopsy whenever indicated, measurements of post-void residual urine (PVR) and Qmax, I-PSS, Quality of life (QoL), International Index of Erectile Function (IIEF-EF) questionnaire, serum prostate-specific antigen (PSA), urine analysis and urine culture.
Interventions
All procedures were performed by two surgeons (AJG, CN) with the experience from more than 500 ThuVEP and 200 HoLEP procedures each. A 26F continuous-flow laser resectoscope in combination with a mechanical tissue morcellator (R. Wolf, Piranha™, Knittlingen, Germany) was used for both procedures. ThuVEP was carried out using a continuous wave Tm:fiber laser (Vela® XL, Boston Scientific, Ratingen, Germany) at 90 W, while HoLEP was performed using a pulsed Ho:YAG laser (Auriga® XL, Boston Scientific, Ratingen, Germany) at 39.6 W (2.2 J, 18 Hz). A 550 µm bare-ended, re-usable laser fiber was used (LightTrail®, Boston Scientific, Ratingen, Germany).
The techniques of HoLEP and ThuVEP have been previously reported in detail [13, 16, 17]. All interventions were carried out using normal saline as irrigation fluid with the patient under spinal or general anesthesia. Depending on the lobe configuration and the size of the prostate, a 2- or 3-lobe technique was performed during all procedures without differences between HoLEP and ThuVEP. The 2-lobe technique was started with a 5- or 7-o’clock incision down to the surgical capsule. Then, the single lateral lobe was enucleated followed by enucleation of the other lobe together with the median lobe. The 3-lobe technique was usually performed in cases of large prostates with a large median lobe. After 5- and 7-o’clock incisions, the middle lobe was enucleated and afterwards the lateral lobes had to be dissected at the layer of the surgical pseudocapsule and pushed into the bladder. At the end of surgery, a 22F three-way foley catheter was inserted for continuous bladder irrigation (CBI) with normal saline, which was stopped the next morning based on our standard department protocol. Routinely, the catheter was removed at the second postoperative day. All patients received a perioperative antibiotic treatment with a second generation cephalosporine regularly or an antibiotic regimen according to an antibiogram until removal of the indwelling catheter. Patients were discharged after removal of the catheter and after being able to void adequately as measured by PVR and Qmax.
Data collection and follow-up
Blood loss was estimated by comparing the serum hemoglobin value before surgery with the corresponding value on the first postoperative day. Perioperative and postoperative complications were reported according to the modified Clavien–Dindo System [15, 18]. All patients were reassessed 1 and 6 months after surgery by IPSS, QoL, Qmax, PVR, and the occurrence of complications. In addition, PSA and prostate volume measurement by TRUS were carried out at 6-month follow-up.
Statistical analysis
Statistical analysis was performed using SPSS 22 (IBM Corp, Armonk, NY, USA). The two-tailed χ2-test (exact Fisher’s test) or the Mann–Whitney U test was applied in order to determine the statistical significance of differences between various parametric and non-parametric parameters of the study arms. Improvement in the assessed parameters in each treatment arm was calculated using the paired t test. Patient data were expressed as median (interquartile range (IQR)). A p value ≤ 0.05 was considered statistically significant.
The primary endpoints of the study were IPSS and Qmax (ml/s). The secondary endpoints were operation time, catheterization time, hospitalization time, the complication rate (CR), QoL, PSA, TRUS, and PVR assessments during follow-up. The sample size was calculated for the detection of statistically significant differences for the final analysis 2 years postoperatively. With α = 0.05 (type I error, 0.025 adjusted for the two primary outcomes) and a power of 90% (β = 0.10), a sample size of 32 patients per group was calculated. The calculation assumed that the relevant difference in IPSS was 3 (SD = 3) and in Qmax 3 (SD = 6) ml/s. Since an overall yearly dropout rate of about 15% was expected, 45 patients per group had to be recruited.
Results
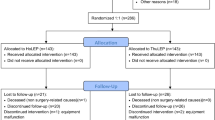
A total of 94 patients were finally enrolled in the study and randomized to ThuVEP (n = 48) or HoLEP (n = 46) (Fig. 1). Figure 1 further shows that in the ThuVEP group, five patients were excluded from assessment due to discovery of prostate cancer (four patients were excluded due to incidental PCa (two patients with pT1a, and two patients with pT1b) receiving curative therapy/active surveillance and one patient with Carcinoma in situ (Cis) of the prostate that required radical cystectomy), while in the HoLEP group, another four patients were excluded for the same reason (three patients were excluded because of incidental PCa (all pT1b) receiving curative therapy/active surveillance and one with locally advanced Prostate cancer). All patients that were diagnosed with either pT1a or pT1b PCa are currently under active surveillance. The patient with the locally advanced PCa was treated with a radical prostatectomy and was staged thereafter with a “pT3” PCa.
There were no statistically significant differences in any baseline characteristics between the groups (Table 1). 50 (53.2%) patients had a gland volume ≥ 80 cc, with 29 (30.9%) patients having a gland ≥ 100 ml, respectively. 18 patients (19.1%) were treated on ongoing anticoagulant therapy in the ThuVEP (n = 9) and HoLEP (n = 9) group (Table 1).
Table 2 lists perioperative data. The median (IQR) operative time was 60 (41–79) min without significant differences between the groups (p = 0.275), although the median (IQR) enucleation time was significantly shorter for ThuVEP [27.3 (21.53–37.65) min] as compared to HoLEP [40 (29.75–50.09) min, p ≤ 0.004]. Median (IQR) enucleation efficiency (resected weight/enucleation time) was significantly higher in ThuVEP [1.87 (1.18–2.59) g/min] compared to HoLEP [1.19 (0.85–1.86) g/min, p ≤ 0.005]. There were no differences between the groups regarding the median (IQR) catheter time [2 (2–2) days] and median (IQR) postoperative stay [2 (2–3) days].
Table 3 lists detailed information on all complications and treatment modalities which occurred during the first 30 postoperative days. Clavien 1 (13.8%), 2 (3.2%), 3a (2.1%), and 3b (4.3%) complications occurred without differences between the groups. The occurrence of postoperative AUR during the first 30 postoperative days was significantly higher after HoLEP compared to ThuVEP (15.2 vs. 2.1%, p ≤ 0.022). However, there were no significant differences in the occurrence of any other complications between the groups (Table 3).
One patient (2.1%) in the ThuVEP group and 4 (8.7%) in the HoLEP group showed transient urge incontinence (p = 0.149), while 9 (18.8%) in the ThuVEP group and 8 (17.4%) in the HoLEP group had transient stress incontinence (p = 0.491). At 6-month follow-up, one patient in the ThuVEP group (2.1%) and one (2.1%) patient in the HoLEP group had urge incontinence. However, none of the patients had stress incontinence at the 6-month follow-up mark. Between the 1- and 6-month follow-up mark, an episode of acute urinary retention (AUR) occurred in 1 patient (2.1%) in the ThuVEP group. Two patients (4.2%) in the ThuVEP group and 4 (8.7%) patients in the HoLEP group developed UTI without significant differences between the groups (p = 0.31).
In both groups, Qmax, PVR, I-PSS, and QoL had improved significantly compared to preoperative assessment at 4-weeks follow-up and continued to improve at 6-month follow-up (p ≤ 0.001) without significant differences between the groups (Table 4). At 6-month follow-up, the median (IQR) reduction of PSA was 80 (62–91.4) vs. 78.9 (53–89.7) (p = 0.814) and the median (IQR) reduction of TRUS estimated prostate size was 75 (68.57–88) vs. 73.91 (68.92–85.88) in the ThuVEP and HoLEP groups, respectively (p ≤ 0.777).
Discussion
Over the last years, a paradigm shift from transurethral resection of the prostate (TURP) and OP for treatment of BPO to minimally invasive transurethral EEP has taken place due to less complications and a shorter hospitalization rate [4].
In this RCT, we could prove that both ThuVEP and HoLEP lead to satisfactory micturition improvement with low perioperative morbidity and significantly improved functional outcomes at 6-month follow-up for large volume prostates (median 80 cc).
Although various studies have shown a benefit using EEP, we still lack of RCTs comparing different EEPs. HoLEP has been proven to be a safe and efficacious procedure with long-lasting micturition improvement [3, 19]. Therefore, HoLEP has been justifiably adopted to the European guidelines as first-line therapy for enlarged prostates ≥ 80 cc [5]. With regard to HoLEP [3] and BipolEP [6,7,8,9,10, 20, 21], numerous trials have been conducted with the result of being equivalent techniques to TURP and OP. Considering more recent EEPs, only few RCTs have been conducted so far. GreenLEP [11], ThuLEP [12, 22], ELEP [23], and DiLEP [10] have all shown promising results regarding the functional outcome. An important advantage of enucleation prostatectomy as opposed to vaporization technique is the availability of prostate tissue for histopathology. In our series, nine patients had to be excluded after randomization to ThuVEP and HoLEP due to an incidental PCa or Cis in the prostate and were treated with a radical prostatectomy, radical cystectomy or are currently under active surveillance, respectively. These patients would have been lost for a curative approach in case of vaporization of the prostate.
Considering this incredible race in modern urology for minimally invasive laser techniques, the thulium laser has emerged to the most challenging enucleation technique next to HoLEP in terms of CR and long-term efficacy [13,14,15,16]. In the preliminary study results, we could already show that ThuVEP leads to an equivalent micturition improvement with a comparable CR at short-term follow-up of 4 weeks [24]. We here present the 6-month outcomes of our RCT comparing ThuVEP with HoLEP.
Despite the technical differences of both procedures (i.e., pulsed vs. continuous laser power), the surgical principals remain identical (i.e., complete removal of the adenoma) with no expected differences regarding functional outcome parameters. Both lasers have arguments for and against its use in clinical practice. The holmium:YAG laser can also be used for stone fragmentation or laser coagulation inside the ureter. Regarding infiltrative PCa, ThuVEP might be superior due to the versatile possibilities of vaporization, resection and enucleation with the thulium laser.
In this RCT, ThuVEP and HoLEP demonstrated equivalent micturition improvement in all functional parameters regarding Qmax, PVR, I-PSS and QoL at 1- and 6-month follow-up in large volume prostates comparable to previously reported RCTs for HoLEP [3, 11, 22], ThuLEP [12, 22], and BipolEP [6, 8, 21, 25, 26]. Most remarkably, the patients’ comfort in subjective micturition improved at the interval of 1- to 6-month follow-up in both groups. The improved functional parameters after 6 months compared to 1 month are a common finding after ThuVEP [27], HoLEP [28], OP [21], BipolEP [6, 10, 20, 21] and DiLEP [10] and most likely due to an incomplete wound healing after 4 weeks. This raises the question if the quality assessment of any BPO technique should be noted at short-term follow-up of 4 weeks.
The median postoperative stay in our series was 2 days with a catheter removal at the day of discharge which is less compared to OP [3, 7,8,9, 20, 21, 29] and TURP [1, 3, 6]. Regarding series including only patients with enlarged prostates (≥ 80 cc), shorter hospitalization rates were seen in series for HoLEP [3, 11], BipolEP [9, 10, 21], and GreenLEP [11], whereas longer hospitalization rates were also noted for BipolEP [7, 9, 10, 20] and DiLEP [10].
The accuracy of EEPs is usually measured by the volume reduction of the prostate and represents the completeness of a procedure during follow-up. Our data reveal a percentage loss of 75 and 73.9% of the gland for ThuVEP and HoLEP, respectively. These results are well comparable to other enucleation techniques [8, 10]. Wu et al. reported a 66% resection rate of the previously measured prostate volume for DiLEP and BipolEP [10]. Similar rates have been reported for HoLEP [25] and ThuVEP [16].
Regarding the short-term complications after 4 weeks using the modified Clavien classification system (CCS), we already discussed the results in a previous publication [24]. The main difference after 4 weeks was a higher recatheterization rate postoperatively after HoLEP compared to ThuVEP (15.2 vs. 2.1%, p ≤ 0.022). The higher recatheterization rate after HoLEP compared to ThuVEP was a surprising result of our study and cannot be totally explained. However, recatheterization rates up to 25% after HoLEP have been described before [3, 26]. Four patients developed AUR within a 4-week interval after surgery. Two patients showed up in our emergency department with coagula inside the bladder that could be easily evacuated. With regard to the other two patients, no cause could be determined for the development of AUR. In all four cases, the patients were able to void adequately after removal of the catheter.
We have noted no differences regarding Clavien 2, 3a and 3b complications. Our results after 4 weeks are comparable with large series regarding TURP [3] and OP series [3, 8, 9, 20], as well as HoLEP [3, 11] BipolEP [6,7,8,9,10,11, 20, 21], GreenLEP [11], ThuLEP [12,13,14,15,16, 22], ELEP [23], and DiLEP [10].
During 6-month follow-up, UTI was noted in two patients (2.1%) in the ThuVEP group and in four patients (4.2%) in the HoLEP group. These data are comparable to other series with a 6-month follow-up [21, 27, 28]. One patient in the ThuVEP group required a recatheterization due to an event of AUR. However, no obstructive cause could be found and the patient could void adequately after removal of the catheter. With regard to incontinence, one patient in each group showed up with urge incontinence which has been tolerated without reintervention. However, none of the patients had stress incontinence at the 6-month follow-up mark.
To evaluate a treatment modality for BPO, the aspect of durability is of major interest. In our RCT, we could show that ThuVEP and HoLEP are comparable procedures after 1 and 6 months of follow-up. To date, none of the patients developed urethral strictures, bladder neck contractures or were treated for regrowth of prostatic adenoma.
Although our study represents the largest series to date comparing ThuVEP with HoLEP in an RCT, several limitations have to be disclosed: (a) One might argue that this RCT was not powered to investigate a non-inferiority of either procedure. To achieve this objective, a study with a larger number of patients in a multicentric study design needs to be investigated. (b) The different power settings of the laser system for HoLEP (39.6 W) and ThuVEP (90 W) might be a limitation of this actual study, although it can be seen as a biased selection of energy setting against the holmium laser. So far, the optimum energy setting for each laser would be 70–120 W for Thulium, and 80–120 W for Holmium. However, shortly a published report showed that low-power HoLEP leads to a comparable functional outcome compared to the data of high-power HoLEP in the literature [30]. In our study, we could notice a difference in operation time which favors the ThuVEP technique; however, this difference turned out not be statistically significant. This stresses our assumption that enucleation technique with complete removal of the adenoma is more important than laser itself. However, as stated before, the difference in the energy setting might be a reasonable explanation for the difference in the enucleation rate next to the type of laser utilized.
Despite these limitations, this study definitely helps us to further understand that enucleation of the prostate is superior to TURP regardless of the energy source or technique. Nevertheless, there needs to be a continuous strive for more RCTs in order to further validate the long-term efficacy of ThuVEP compared to HoLEP.
Conclusions
This RCT confirms that both ThuVEP and HoLEP are comparable treatment modalities in terms of perioperative complications and functional outcome parameters. Conclusively, none of either procedure seems to be superior for the treatment of BPO at 6-month follow-up. Though, in order to draw final conclusions, a longer follow-up is needed to prove the long-term durability.
References
Gratzke C, Schlenker B, Seitz M et al (2007) Complications and early postoperative outcome after open prostatectomy in patients with benign prostatic enlargement: results of a prospective multicenter study. J Urol 177:1419–1422. https://doi.org/10.1016/j.juro.2006.11.062
Fraundorfer MR, Gilling PJ (1998) Holmium:YAG laser enucleation of the prostate combined with mechanical morcellation: preliminary results. Eur Urol 33:69–72
Cornu J-N, Ahyai S, Bachmann A et al (2015) A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol 67:1066–1096. https://doi.org/10.1016/j.eururo.2014.06.017
Gilling PJ (2013) Laser enucleation is increasingly becoming the standard of care for treatment of benign prostatic hyperplasia of all sizes. Eur Urol 63(5):868–871. https://doi.org/10.1016/j.eururo.2013.01.001
Gravas S, Bach T, Bachmann A et al (2016) Guidelines on the management of non-neurogenic male lower urinary tract symptoms (LUTS), incl. benign prostatic obstruction (BPO) EAU. http://uroweb.org/guideline/treatment-of-non-neurogenicmaleluts/. Accessed Feb 2018
Zhu L, Chen S, Yang S et al (2013) Electrosurgical enucleation vs bipolar transurethral resection for prostates larger than 70 ml: a prospective, randomized trial with 5-year followup. J Urol 189:1427–1431. https://doi.org/10.1016/j.juro.2012.10.117
Rao J-M, Yang J-R, Ren Y-X et al (2013) Plasmakinetic enucleation of the prostate versus transvesical open prostatectomy for benign prostatic hyperplasia > 80 mL: 12-month follow-up results of a randomized clinical trial. Urology 82:176–181. https://doi.org/10.1016/j.urology.2013.02.032
Geavlete B, Stanescu F, Iacoboaie C, Geavlete P (2013) Bipolar plasma enucleation of the prostate vs open prostatectomy in large benign prostatic hyperplasia cases—a medium term, prospective, randomized comparison. BJU Int 111:793–803. https://doi.org/10.1111/j.1464-410X.2012.11730.x
Ou R, Deng X, Yang W et al (2013) Transurethral enucleation and resection of the prostate vs transvesical prostatectomy for prostate volumes > 80 mL: a prospective randomized study. BJU Int 112:239–245. https://doi.org/10.1111/bju.12181
Wu G, Hong Z, Li C et al (2016) A comparative study of diode laser and plasmakinetic in transurethral enucleation of the prostate for treating large volume benign prostatic hyperplasia: a randomized clinical trial with 12-month follow-up. Lasers Med Sci 31:599–604. https://doi.org/10.1007/s10103-016-1883-1
Elshal AM, Elkoushy MA, El-Nahas AR et al (2015) GreenLight™ laser (XPS) photoselective vapoenucleation versus holmium laser enucleation of the prostate for the treatment of symptomatic benign prostatic hyperplasia: a randomized controlled study. J Urol 193:927–934. https://doi.org/10.1016/j.juro.2014.09.097
Yang Z, Wang X, Liu T (2013) Thulium laser enucleation versus plasmakinetic resection of the prostate: a randomized prospective trial with 18-month follow-up. Urology 81:396–400. https://doi.org/10.1016/j.urology.2012.08.069
Bach T, Wendt-Nordahl G, Michel MS et al (2009) Feasibility and efficacy of thulium:YAG laser enucleation (vapoenucleation) of the prostate. World J Urol 27:541–545. https://doi.org/10.1007/s00345-008-0370-0
Netsch C, Engbert A, Bach T, Gross AJ (2014) Long-term outcome following thulium vapoenucleation of the prostate. World J Urol 32:1551–1558. https://doi.org/10.1007/s00345-014-1260-2
Gross AJ, Netsch C, Knipper S et al (2013) Complications and early postoperative outcome in 1080 patients after thulium vapoenucleation of the prostate: results at a single institution. Eur Urol 63:859–867. https://doi.org/10.1016/j.eururo.2012.11.048
Bach T, Netsch C, Pohlmann L et al (2011) Thulium:YAG vapoenucleation in large volume prostates. J Urol 186:2323–2327. https://doi.org/10.1016/j.juro.2011.07.073
Gilling P (2008) Holmium laser enucleation of the prostate (HoLEP). BJU Int 101:131–142. https://doi.org/10.1111/j.1464-410X.2007.07341.x
Mamoulakis C, Efthimiou I, Kazoulis S et al (2011) The modified Clavien classification system: a standardized platform for reporting complications in transurethral resection of the prostate. World J Urol 29:205–210. https://doi.org/10.1007/s00345-010-0566-y
Ahyai SA, Gilling P, Kaplan SA et al (2010) Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol 58:384–397. https://doi.org/10.1016/j.eururo.2010.06.005
Chen S, Zhu L, Cai J et al (2014) Plasmakinetic enucleation of the prostate compared with open prostatectomy for prostates larger than 100 g: a randomized noninferiority controlled trial with long-term results at 6 years. Eur Urol 66:284–291. https://doi.org/10.1016/j.eururo.2014.01.010
Geavlete B, Bulai C, Ene C et al (2015) Bipolar vaporization, resection, and enucleation versus open prostatectomy: optimal treatment alternatives in large prostate cases? J Endourol 29:323–331. https://doi.org/10.1089/end.2014.0493
Zhang F, Shao Q, Herrmann TRW et al (2012) Thulium laser versus holmium laser transurethral enucleation of the prostate: 18-month follow-up data of a single center. Urology 79:869–874. https://doi.org/10.1016/j.urology.2011.12.018
Lusuardi L, Myatt A, Sieberer M et al (2011) Safety and efficacy of eraser laser enucleation of the prostate: preliminary report. J Urol 186:1967–1971. https://doi.org/10.1016/j.juro.2011.07.026
Netsch C, Becker B, Tiburtius C et al (2017) A prospective, randomized trial comparing thulium vapoenucleation with holmium laser enucleation of the prostate for the treatment of symptomatic benign prostatic obstruction: perioperative safety and efficacy. World J Urol 35:1913–1921. https://doi.org/10.1007/s00345-017-2071-z
Chen Y-B, Chen Q, Wang Z et al (2013) A prospective, randomized clinical trial comparing plasmakinetic resection of the prostate with holmium laser enucleation of the prostate based on a 2-year followup. J Urol 189:217–222. https://doi.org/10.1016/j.juro.2012.08.087
Neill MG, Gilling PJ, Kennett KM et al (2006) Randomized trial comparing holmium laser enucleation of prostate with plasmakinetic enucleation of prostate for treatment of benign prostatic hyperplasia. Urology 68:1020–1024. https://doi.org/10.1016/j.urology.2006.06.021
Gross AJ, Orywal AK, Becker B, Netsch C (2017) Five-year outcomes of thulium vapoenucleation of the prostate for symptomatic benign prostatic obstruction. World J Urol. https://doi.org/10.1007/s00345-017-2034-4
El Tayeb MM, Jacob JM, Bhojani N et al (2016) Holmium laser enucleation of the prostate in patients requiring anticoagulation. J Endourol 30:805–809. https://doi.org/10.1089/end.2016.0070
Reich O, Gratzke C, Bachmann A et al (2008) Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol 180:246–249. https://doi.org/10.1016/j.juro.2008.03.058
Minagawa S, Okada S, Morikawa H (2017) Safety and effectiveness of holmium laser enucleation of the prostate using a low-power laser. Urology 110:51–55. https://doi.org/10.1016/j.urology.2017.08.034
Funding
Funding was obtained from Boston Scientific (grant number:#ISRURO400001)
Author information
Authors and Affiliations
Contributions
All authors whose names appear on the submission have contributed sufficiently to the scientific work and, therefore, share collective responsibility and accountability for the results. B: Protocol/project development, data collection, data analysis, manuscript writing/editing, H: Protocol/project development, manuscript writing/editing, G: Protocol/project development, data collection, manuscript writing/editing, N: Protocol/project development, Data collection, data analysis, manuscript writing/editing
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Becker, B., Herrmann, T.R.W., Gross, A.J. et al. Thulium vapoenucleation of the prostate versus holmium laser enucleation of the prostate for the treatment of large volume prostates: preliminary 6-month safety and efficacy results of a prospective randomized trial. World J Urol 36, 1663–1671 (2018). https://doi.org/10.1007/s00345-018-2321-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2321-8