Abstract
Objective
A new computer tool is proposed to distinguish between focal nodular hyperplasia (FNH) and an inflammatory hepatocellular adenoma (I-HCA) using contrast-enhanced ultrasound (CEUS). The new method was compared with the usual qualitative analysis.
Methods
The proposed tool embeds an “optical flow” algorithm, designed to mimic the human visual perception of object transport in image series, to quantitatively analyse apparent microbubble transport parameters visible on CEUS. Qualitative (visual) and quantitative (computer-assisted) CEUS data were compared in a cohort of adult patients with either FNH or I-HCA based on pathological and radiological results. For quantitative analysis, several computer-assisted classification models were tested and subjected to cross-validation. The accuracies, area under the receiver-operating characteristic curve (AUROC), sensitivity and specificity, positive predictive values (PPVs), negative predictive values (NPVs), false predictive rate (FPRs) and false negative rate (FNRs) were recorded.
Results
Forty-six patients with FNH (n = 29) or I-HCA (n = 17) with 47 tumours (one patient with 2 I-HCA) were analysed. The qualitative diagnostic parameters were accuracy = 93.6%, AUROC = 0.94, sensitivity = 94.4%, specificity = 93.1%, PPV = 89.5%, NPV = 96.4%, FPR = 6.9% and FNR = 5.6%. The quantitative diagnostic parameters were accuracy = 95.9%, AUROC = 0.97, sensitivity = 93.4%, specificity = 97.6%, PPV = 95.3%, NPV = 96.7%, FPR = 2.4% and FNR = 6.6%.
Conclusions
Microbubble transport patterns evident on CEUS are valuable diagnostic indicators. Machine-learning algorithms analysing such data facilitate the diagnosis of FNH and I-HCA tumours.
Key Points
• Distinguishing between focal nodular hyperplasia and an inflammatory hepatocellular adenoma using dynamic contrast-enhanced ultrasound is sometimes difficult.
• Microbubble transport patterns evident on contrast-enhanced sonography are valuable diagnostic indicators.
• Machine-learning algorithms analysing microbubble transport patterns facilitate the diagnosis of FNH and I-HCA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Benign hepatocellular tumours are rare, constituting 10% of all hepatic tumours [1]. Two large groups of benign hepatocellular tumours can be distinguished: reactive regenerative lesions (focal nodular hyperplasias [FNHs]) and tumoural lesions (hepatocellular adenomas [HCAs]). Both lesions are most common in young females [1]. Diagnostic imaging is essential to guide treatment decisions, which range from no treatment to surgical resection or confirmatory biopsy. Traditionally, multiphase computed tomography (CT) or magnetic resonance imaging (MRI) has been used for detailed evaluation of hepatic lesions. However, the high-level radiation associated with multiphase CT and the limited accessibility of MRI have rendered dynamic contrast agent-enhanced ultrasound (CEUS) an attractive, safe, non-invasive, accurate, and economic tool for evaluating hepatic lesions [2,3,4,5,6]. Although the appearance is not always typical in some cases, both FNH and HCA demonstrate typical, reproducible, arterial-phase enhancement patterns on CEUS in most cases. The diagnostic criteria for FNH are a hyper-enhancing lesion in the arterial phase with rapid centrifugal filling from a central vessel, and radial vascular branches (the “spoke and wheel” sign) [2, 5] and also sustained enhancement in portal and late phase [7]. HCAs constitute a heterogeneous group of tumours exhibiting multiple histological subtypes (inflammatory, with FNH1A or catenin gene mutations, or unclassified) [8]. On CEUS, HCAs are hyper-enhancing in the arterial phase; the enhancement pattern commences peripherally and exhibits rapid centripetal filling; this pattern is characteristic of 86–90% of all inflammatory HCAs (I-HCAs). Other HCA subtypes exhibit iso-vascularity or moderate hyper-vascularity, with mixed filling patterns in the arterial phase [2, 9]. In clinical practice, it is essential to distinguish FNH from adenoma to ensure appropriate management. Confirmed FNHs are managed conservatively (with regular follow-up); HCAs require cessation of oral contraceptive use, (commonly) biopsy, and either surgery or (at least) follow-up imaging. I-HCA show the most important hyper-vascularity, and 10–15% of I-HCA are also found to be β-catenin activated with a risk for malignant transformation. Distinguishing between FNH and I-HCA using CEUS is sometimes difficult because both lesions evidence hyper-enhancement during the arterial phase and it can be challenging to qualitatively differentiate centrifugal from centripetal tumour filling, particularly for larger nodules. Computer-assisted methods are thus required for quantitative spatiotemporal assessment of organ perfusion. Such techniques must be faster and more reproducible than visual analysis, and must lack learning curves. Efforts have been made to quantify enhancement parameters in vascular compartments as indicators of several pathological conditions [10,11,12,13,14]. In particular, transport equations have been recently derived to estimate microbubble velocity at the time of bolus contrast arrival [15]. In practice, an “optical flow” algorithm is employed to mimic the human visual perception of microbubble transport in CEUS [16,17,18]. Here, we use this approach to quantitatively distinguish between FNH and I-HCA. We quantify divergence (sources and sinks), curling (shearing), amplitudes, and convergence towards the centre of tumour (centrifugal/centripetal nature) in dense transport fields [16]; these are very simple indicators of displacement vector directions, orientations, and magnitudes. In turn, these serve as inputs to a binary FNH/I-HCA classifier.
The purpose was to compare, as a preliminary study, the original concept of computer-assisted method with the usual qualitative analysis for the diagnosis of two benign hepatocellular tumours (FNH and I-HCA) with hyper-vascularity during the arterial phase of the CEUS.
Materials and methods
Study design and population
In this retrospective single-centre study conducted from July 2005 to July 2018, we identified images from patients who underwent CEUS and were (otherwise) definitively diagnosed with FNH or I-HCA. We included I-HCA patients who had been histologically diagnosed [6] and FNH patients diagnosed based on commonly accepted MRI criteria [3], imaging follow-up, or histology. All MRIs were performed using a 1.5-T machine running a published imaging protocol [19, 20]. The study adhered to all local regulations and data protection agency recommendations (the National Commission on Informatics and Liberty (CNIL) dictates). Patients have been informed of the use of their data anonymously.
Demographic characteristics
We enrolled 46 patients (Table 1) with the inclusion criteria; 29 had FNH and 17 I-HCA (18 I-HCA tumours were analysed because one patient had two tumours). Of 29 FNH patients, 23 (79%) were female and the median age was 44 (21–61) years; of 17 I-HCA patients, 16 (94%) were female and the median age was 40.5 (21–66) years. The median diameters of FNH and I-HCA lesions were, respectively, 2.9 (3–10) and 6.9 (3.4–12) cm. Histological data of the 18 I-HCA tumours were available for 15 surgical specimens and 3 percutaneous biopsies Histological data on 7/29 FNH tumours (24%) were available (percutaneous biopsy, six samples; one surgical sample); imaging follow-up data were available for 15/22 patients without histological diagnosis (68%) with a median follow-up of 12 (4–84) months ; CEUS was performed using Sequoia (n = 37), S2000 (n = 4), and S3000 (n = 5) instruments.
Histological analysis
Histological samples were obtained by biopsy or during surgical resection; for ethical reasons, no samples were taken purely for the purpose of this study; clinical indications were required. All analyses were performed as previously described [8, 9, 19], in the same laboratory.
CEUS protocol
CEUS was performed by abdominal radiologists who had 5–10 years of experience. Each patient received a bolus injection of ultrasound contrast agent (SonoVue, Bracco). Contrast-enhanced sequences were obtained using dedicated, low mechanical index (MI) contrast-imaging software (MI < 0.2) employing one of three US machines (Sequoia, S2000 and S3000; a Siemens Medical Solution instrument featuring Cadence Contrast Pulse Sequencing [CPS]; and a Convex Array 4C1-S probe). Standard pre-settings were used, but it was possible to adjust settings for individual patients. SonoVue was injected intravenously as a bolus of 2.4 mL via a 20-gauge cannula into the antecubital vein, followed by flushing with 5 mL normal saline. Digital cine clips showing dynamic contrast enhancement within the lesion and surrounding liver tissue were continuously recorded, commencing 5 s before SonoVue injection and covering the arterial (10–45 s post-injection), portal (60–90 s), and late (120–150 s) phases. Injection was repeated using the same dose (2.4 mL SonoVue) if the data were of poor quality. All sequences were digitally stored. Intra-tumoural vascular geometry and lesional enhancement patterns were evaluated.
CEUS analysis of lesional type
Qualitative visual analysis
Data were reviewed in consensus by two abdominal radiologists blinded to pathological and MRI diagnoses. Each lesion was classified using pre-defined criteria for FNH and I-HCA. For FNH, these were hyper-enhancement in the arterial phase, with rapid centrifugal filling; (usually) an obvious central vessel and radial vascular branches (especially in larger lesions; the “spoke and wheel” sign); and iso- or hyper-enhancement in the portal and venous phases, without washout. For I-HCA, the criteria were hyper-enhancement in the arterial phase, frequently accompanied by rapid centripetal filling; no radial vascular structure; and iso- or hyper-enhancement in the portal and venous phases, without washout [3, 9, 21].
Computer-assisted quantitative analysis using a transport equation model
Microbubble transport fields in lesions were estimated (using a transport equation) on a pixel-by-pixel basis employing the “optical flow” process [15]. The “optical flow” problem has long been studied by vision scientists in efforts to analyse general visual motion in images of a moving target [16, 17]. For each lesion, the absolute changes in four image-based displacement indicators were calculated: (i) the divergence δ (reflecting the presence of sources and sinks); (ii) the curl ρ (reflecting local vortices); (iii) the amplitude γ (reflecting the magnitude of apparent displacement); and (iv) the centripetal nature τ (reflecting the flow field convergence towards the centre of the tumour). The analysis was restricted to a region of interest, manually drawn on a high-contrast CEUS image, encompassing the tumour. The analytical window size was fixed at 2 s commencing at the bolus arrival time, and thus covered the filling phase. The reader is referred to the Appendix for additional information on numerical resolution and implementation. All computer-assisted analyses were blinded to pathological data.
Statistical analysis
The accuracies, area under the ROC curve (AUROC), sensitivity, specificity, positive predictive values (PPVs), negative predictive values (NPVs), false predictive rates (FPRs), and false negative rates (FNRs) of qualitative and quantitative analyses were recorded (we considered the diagnostic of an adenoma as a “positive case” in the scope of this study).
For quantitative analyses, using one of the four microbubble displacement indicators (δ, ρ, γ, or τ) as an input feature, we developed machine-learning models to differentiate between FNH and I-HCA. For this binary classification task, the following four machine-learning algorithms were applied using the commercial software Matlab (©1994–2019 The MathWorks, Inc.)/“Statistics and Machine Learning” toolbox: random forest (RF), k-nearest neighbour (KNN), support vector machine (SVM), and logistic regression (LR). Default hyperparameters in Matlab implementations were employed. We refer the interested reader to [22, 23] for additional information about above-mentioned computer-assisted classification algorithms. We evaluated the diagnostic performances through self-validation (the complete 47-tumour set was used for both train and test samples) and through 10-fold-stratified cross-validation (the 47-tumour set was randomly partitioned into complementary 90%-training and 10%-test subsets). The cross-validation steps were repeated 100 times with shuffling of the folds and test metric averages calculated. We also compared the medians and interquartile ranges of all four indicators using the unpaired Mann–Whitney U test. A p value < 0.025 was considered to reflect statistical significance.
Results
Qualitative CEUS analysis
FNH and I-HCA were correctly identified via qualitative CEUS in 27/29 and 17/18 tumours, respectively (accuracy = 93.6%, AUROC = 0.94, sensitivity = 94.4%, specificity = 93.1%, PPV = 89.5%, NPV = 96.4%, FPR = 6.9%, FNR = 5.6%; Table 2, first row).
Quantitative CEUS analysis
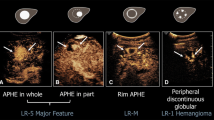
Figures 1 and 2 show typical microbubble transport fields as revealed by dynamic contrast imaging; one clip (Fig. 1) is from an FNH patient and the other (Fig. 2) from an I-HCA patient. Of the four tested transport indicators, divergence and centripetal indicators differed most significantly between the two populations (Mann–Whitney test, p value = 2 × 10−4 for divergence and 1 × 10−7 for the centripetal indicator) (Figs. 3 and 4). The centripetal indicator served as a valuable binary classifier in all tested machine-learning systems (Table 2). In particular, using the naïve Bayes classifier applied on the centripetal indicator, the diagnostic parameters were accuracy = 95.9%, AUROC = 0.97, sensitivity = 93.4%, specificity = 97.6%, PPV = 95.3%, NPV = 96.7%, FPR = 2.4%, and FNR = 6.6% (in average over the 100 cross-validation steps, FNH and I-HCA were thus correctly identified in 28.3/29 and 16.8/18 tumours, respectively).
Typical results obtained when evaluating an FNH lesion. Data obtained at different CEUS timepoints are shown: 0.5 s (left column), 1 s (middle column), and 1.5 s (right column) after bolus arrival. The manually drawn mask encompassing the lesion is shown in a. a–c Contrast images. d–f Estimated, apparent transport vector fields. The flow field exhibits fast centrifugal filling of the lesion from a central vessel and radial vascular branches. The pixelwise centripetal indicator is shown in the insets of the bottom row (note the large negative values, attributable to centrifugal filling of the lesion, and the small positive values attributable to the tumour feeding arterial)
Typical results from a patient with an I-HCA lesion. The manually drawn mask encompassing the lesion is shown in a. Data obtained at different times during CEUS are shown: 0.5 s (left column), 1 s (middle column), and 1.5 s (right column) after bolus arrival. a–c Contrast images. d–f Estimated, apparent vector transport fields. The flow field is hyper-enhanced in the arterial phase (enhancement commences peripherally) and exhibits rapid centripetal filling. The pixel-wise centripetal indicator is shown as insets in the bottom row (note the large positive values, attributable to centripetal filling of the lesion)
Boxplots of indicators of the four dense transport fields (divergence δ (a), curl ρ (b), amplitude γ (c), and centripetal indicator τ (d)) for both patient populations (FNH vs. I-HCA self-validations). The medians are shown by the central marks, the first and third quartiles are the edges of the boxes, the whiskers extend to the most extreme timepoints not considered to be outliers, and the outliers are individually marked in red
Discussion
We show that the dense transport fields provide valuable kinetic information in CEUS time series; the results are more accurate than those of qualitative visual analysis. Using the qualitative analysis, one false-negative case and two false-positive cases were to deplore. Concerning the false-negative case, the filling direction was difficult to determine visually. Concerning the two false-positive cases, one tumour (44 mm) presented two feeding pedicles, and one (22 mm) underwent a too-fast filling. For both FNH tumours, it was also difficult to appreciate visually the centrifugal filling. A quantitative approach delivers reproducible results and minimises operator dependency, as visual interpretation of CEUS images lacks a learning curve when the process is automated. Our method deals with the intrinsic variations in spatiotemporal greys that are inevitable during dynamic imaging. This allows numerical access to visual perceptions of microbubble trajectories. We used four simple indicators (δ, ρ, γ, and τ) of transport field direction/orientation and amplitude. The amplitude and curl indicators were not useful (Fig. 4b, c), whereas the divergence and centripetal indicators were (Fig. 4a, d). The best results were obtained using the indicator τ which best fits the initial centrifugal/centripetal tumour filling hypothesis (Fig. 4d). For its part, the divergence operator gave decent results. In theory, the divergence of any vector field is positive for sources (centrifugal trajectories) and negative for sinks (centripetal trajectories). The divergence operators were positive for both FNH and I-HCA data; bolus arrival manifested as one or several sources of microbubbles. However, for I-HCA lesions, the divergence operator was modulated by centripetal filling, whereas the divergence operator was enhanced by centrifugal filling in FNH patients.
Using our quantitative method, diagnosis is near instantaneous once the region of interest (encompassing the tumour) is delineated. Although the duration of the temporal window for the analysis must be sufficient to cover the filling phase, 2 s was adequate; this is a great advantage, eliminating all long-term bias imparted by probe motion, and respiratory and other motion artefacts [24, 25].
Several limitations of our work must be mentioned, particularly the small sample size. This was a single-centre retrospective study lacking an external validation cohort. Considering that only two categories of focal liver lesions were examined (FNH and I-HCA), an inherent overestimation of both qualitative and quantitative analyses has to be taken into account. Also, the mean tumour diameter was significantly smaller in the FNH group, associated with recruitment bias: only patients with histological diagnoses obtained after surgical resection or via percutaneous biopsy were included in the I-HCA group. However, in our centre, when an I-HCA tumour is identified using MRI [26] or CEUS, a pathological analysis is performed only when the tumour diameter is > 3 cm. Thus, the I-HCA group featured only tumours that met this criterion, unlike the FNH group, for which tumours of all diameters (including small tumours) were evaluated. Also, the fact that any US artefacts can intrinsically be interpreted as “false” motions by the transport equation constitutes a major source of uncertainty. This may bias the microbubble estimations in transport fields, in turn affecting all four image-based indicators. This is also of concern when brief US “shadow” artefacts develop in obese patients (one of our cohort was obese and was constantly misclassified by our quantitative approach due to poor image quality). Similarly, in-plane and/or out-of-plane organ motion within the image field of view must be no more than moderate. Please note that when organ motions are large or complex, it is possible to “pop” microbubbles on-line to virtually repeat the imaging session. Alternatively, image post-processing strategies may be valuable [24, 27,28,29] (Appendix). Finally, manually drawn masks encompassing lesions must exclude adjacent feeding arterials; otherwise, the estimated displacement is likely to be calculated from the border to the centre of the tumour, compromising FNH diagnosis.
In conclusion, this proof-of-concept study indicates that microbubble displacements evident on CEUS can be used to efficiently diagnose FNH/I-HCA lesions. Machine learning allows for computer-assisted diagnoses. In the future, we will optimise the model [27], enrol larger patient cohorts, include other lesional features, and study other pathologies.
Abbreviations
- AUC:
-
Area under the curve
- CEUS:
-
Contrast-enhanced ultrasound
- CNIL:
-
National Commission on Informatics and Liberty
- CT:
-
Computed tomography
- FNH:
-
Focal nodular hyperplasias
- GB:
-
Gigabit
- HCA:
-
Hepatocellular adenomas
- I-HCA:
-
Inflammatory hepatocellular adenoma
- KNN:
-
k-nearest neighbour
- LR:
-
Logistic regression
- MRI:
-
Magnetic resonance imaging
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- RAM:
-
Random access memory
- RF:
-
Random forest
- ROC:
-
Receiver-operating characteristic
- SVM:
-
Support vector machine
- T:
-
Tesla
- US:
-
Ultrasound
References
Cherqui D, Rahmouni A, Charlotte F et al (1995) Management of focal nodular hyperplasia and hepatocellular adenoma in young women: a series of 41 patients with clinical, radiological, and pathological correlations. Hepatology 22(6):1674–1681
Burrowes DP, Medellin A, Harris AC, Milot L, Wilson SR (2017) Contrast-enhanced US approach to the diagnosis of focal liver masses. Radiographics 37(5):1388–1400
Dioguardi Burgio M, Ronot M, Salvaggio G, Vilgrain V, Brancatelli G (2016) Imaging of hepatic focal nodular hyperplasia: pictorial review and diagnostic strategy. Semin Ultrasound CT MR 37(6):511–524
Trillaud H, Bruel JM, Valette PJ et al (2009) Characterization of focal liver lesions with SonoVue-enhanced sonography: international multicenter-study in comparison to CT and MRI. World J Gastroenterol 15(30):3748–3756
Baranes L, Chiaradia M, Pigneur F et al (2013) Imaging benign hepatocellular tumors: atypical forms and diagnostic traps. Diagn Interv Imaging 94(7–8):677–695
Onofrio M, Crosara S, De Robertis R, Canestrini S, Mucelli RP (2015) Contrast enhanced ultrasound of focal liver lesions. AJR Am J Roentgenol 205:W56–66
Bartolotta TV, Taibbi A, Matranga D, Malizia G, Lagalla R, Midiri M (2010) Hepatic focal nodular hyperplasia:contrast-enhanced ultrasound findings with emphasis on lesion size, depth and liver echogenicity. Eur Radiol 20:2248–2256
Bioulac-Sage P, Rebouissou S, Thomas C et al (2007) Hepatocellular adenoma subtype classification using molecular markers and immunohistochemistry. Hepatology 46(3):740–748
Laumonier H, Cailliez H, Balabaud C et al (2012) Role of contrast-enhanced sonography in differentiation of subtypes of hepatocellular adenoma: correlation with MRI findings. AJR Am J Roentgenol 199(2):341–348
Tranquart F, Mercier L, Frinking P, Gaud E, Arditi M (2012) Perfusion quantification in contrast-enhanced ultrasound (CEUS)–ready for research projects and routine clinical use. Ultraschall Med 33(1):S31–S38
Rognin NG, Arditi M, Mercier L et al (2009) Parametric imaging of dynamic vascular patterns of focal liver lesions in contrast-enhanced ultra-sound. IEEE Ultrasonics Symp Proc 1282-1285
Dietrich CF, Averkiou MA, Correas JM, Lasau N, Leen E, Piscaglia F (2012) An EFSUMB introduction into dynamic contrast-enhanced ultrasound (DCE-US) for quantification of tumour perfusion. Ultraschall Med 33:344–351
Strouthos C, Lampaksis M, Sboros V, McNeilly A, Averkiou M (2010) Indicator dilution models for the quantification of microvascular blood flow with bolus administration of ultrasound contrast agents. IEEE Trans Ultrason Ferroelectr Freq Control 57(6):1296–1310
Mischi M, Kuenen MPJ, Wijkstra H (2012) Angiogenesis imaging by spatiotemporal analysis of ultrasound contrast agent dispersion kinetics. IEEE Trans Ultrason Ferroelectr Freq Control 59(4):621–629
Denis de Senneville B, Novell A, Arthuis C et al (2018) Development of a fluid dynamic model for quantitative contrast-enhanced ultrasound imaging. IEEE Trans Med Imaging 37(2):372–383
Corpetti E, Mémin E, Pérez P (2002) Dense estimation of fluid flows. IEEE Trans Pattern Anal Mach Intell 24(3):365–380
Horn B, Schunk B (1981) Determining optical flow. Artif Intell 17:185–203
Zachiu C, Papadakis N, Ries M, Moonen CTW, Denis de Senneville B (2015) An improved optical flow tracking technique for real-time MR-guided beam therapies in moving organs. Phys Med Biol 60(23):9003
Laumonier H, Bioulac-Sage P, Laurent C, Zucman-Rossi J, Balabaud C, Trillaud H (2008) Hepatocellular adenomas: magnetic resonance imaging features as a function of molecular pathological classification. Hepatology 48(3):808–818
van Aalten SM, Thomeer MGJ, Terkivatan T et al (2011) Hepatocellular adenomas: correlation of MR imaging findings with pathologic subtype classification. Radiology 261(1):172–181
Quaia E, Calliada F, Bertolotto M et al (2004) Characterization of focal liver lesions with contrast-specific US modes and a sulfur hexafluoride-filled microbubble contrast agent: diagnostic performance and confidence. Radiology 232(2):420–430
Kohavi R (1995) A study of cross-validation and bootstrap for accuracy estimation and model selection. International Joint Conference on Artificial Intelligence (IJCAI) pp 1137–1143
Cantor SB, Kattan MW (2000) Determining the area under the ROC curve for a binary diagnostic test. Med Decis Making 20(4):468–470
De Luca V, Székely G, Tanner C (2015) Estimation of large-scale organ motion in B-mode ultrasound image sequences: a survey. Ultrasound Med Biol 41(12):3044–3062
Pratikakis I, Barillot C, Hellier P, Memin E (2003) Robust multiscale deformable registration of 3d ultrasound images. Int J Image Graph 3(4):547–565
Bise S, Frulio N, Hocquelet A et al (2018) New MRI features improve subtype classification of hepatocellular adenoma. Eur Radiol. https://doi.org/10.1007/s00330-018-5784-5
Ackermann D, Schmitz G (2016) Detection and tracking of multiple microbubbles in ultrasound b-mode images. IEEE Trans Ultrason Ferroelectr Freq Control 63(1):72–82
Cifor A, Risser L, Chung D, Anderson EM, Schnabel JA (2013) Hybrid feature-based diffeomorphic registration for tumor tracking in 2-D liver ultrasound images. IEEE Trans Med Imaging 32(9):1647–1656
Shapiro LG, Stockman GC (2001) Computer vision. Pearson, pp 137–150
Acknowledgements
Experiments presented in this paper were carried out using the PlaFRIM experimental testbed, supported by Inria, CNRS (LABRI and IMB), Université de Bordeaux, Bordeaux INP, and Conseil Régional d’Aquitaine (see www.plafrim.fr/). The authors thank the Laboratory of Excellence TRAIL ANR-10-LABX-57 for funding. This study has been carried out with the financial support of the French National Research Agency (ANR) in the frame of the “Investments for the future” Programme IdEx Bordeaux-CPU (ANR-10-IDEX-03-02).
Funding
The authors thank the Laboratory of Excellence TRAIL ANR-10-LABX-57 for funding. This study has been carried out with the financial support of the French National Research Agency (ANR) in the frame of the “Investments for the future” Programme IdEx Bordeaux-CPU (ANR-10-IDEX-03-02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Hervé Trillaud.
Conflict of interest
Hervé Trillaud: sponsored a lecture for Bracco and congress support. The other authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Patients have been informed of the use of their data anonymously.
Ethical approval
Institutional review board approval was obtained.
Study subjects or cohorts overlap
Some study subjects (10 cases) have been previously reported in Hepatology 2008 by Laumonier et al—“Hepatocellular adenomas: magnetic resonance imaging features as a function of molecular pathological classification”; AJR Am J Roentgenol 2012 by Laumonier et al—“Role of contrast-enhanced sonography in differentiation of subtypes of hepatocellular adenoma: correlation with MRI findings”; and European Radiology 2018 by Bise et al—“New MRI features improve subtype classification of hepatocellular adenoma”.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Denis de Senneville, B., Frulio, N., Laumonier, H. et al. Liver contrast-enhanced sonography: computer-assisted differentiation between focal nodular hyperplasia and inflammatory hepatocellular adenoma by reference to microbubble transport patterns. Eur Radiol 30, 2995–3003 (2020). https://doi.org/10.1007/s00330-019-06566-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06566-1