Abstract
Objectives
To determine whether multiphasic dynamic CT can preoperatively predict lymphovascular invasion (LVI) in advanced gastric cancer (AGC).
Methods
278 patients with AGC who underwent preoperative multiphasic dynamic CT were retrospectively recruited. Tumour CT attenuation difference between non-contrast and arterial (ΔAP), portal (ΔPP) and delayed phase (ΔDP), tumour-spleen attenuation difference in the portal phase (ΔT-S), tumour contrast enhancement ratios (CERs), tumour-to-spleen ratio (TSR) and tumour volumes were obtained. All CT-derived parameters and clinicopathological variables associated with LVI were analysed by univariate analysis, followed by multivariate and receiver operator characteristics (ROC) analysis. Associations between CT predictors for LVI and histopathological characteristics were evaluated by the chi-square test.
Results
ΔPP (OR, 1.056; 95% CI: 1.032–1.080) and ΔT-S (OR, 1.043; 95% CI: 1.020–1.066) are independent predictors for LVI in AGC. ΔPP, ΔT-S and their combination correctly predicted LVI in 74.8% (AUC, 0.775; sensitivity, 88.6%; specificity, 54.1%), 68.7% (AUC, 0.747; sensitivity, 68.3%; specificity, 69.4%) and 71.7% (AUC, 0.800; sensitivity, 67.6%; specificity, 77.8%), respectively. There were significant associations between CT predictors for LVI with tumour histological differentiation and Lauren classification.
Conclusion
Multiphasic dynamic CT provides a non-invasive method to predict LVI in AGC through quantitative enhancement measurement.
Key points
• Lymphovascular invasion rarely can be evaluated preoperatively in advanced gastric cancer (AGC).
• Δ PP and Δ T-S were independent predictors for LVI in patients with AGC.
• Δ PP and Δ T-S showed acceptable predictive performance for LVI.
• Combination of Δ PP and Δ T-S improved predictive performance for LVI.
• Multiphasic dynamic CT may be a useful adjunct for detecting LVI preoperatively.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Curative surgery is the best treatment option for patients with resectable advanced gastric cancer (AGC) [1]. However, the long-term postoperative outcome is far from satisfactory because 40–50% of patients with AGC will develop local recurrence or distant metastasis [2]. Therefore, accurate preoperative risk estimates are required for treatment planning. Despite its use as a gold standard to predict outcome, the 7th edition of the American Joint Committee on Cancer (AJCC) failed to distinguish heterogeneous survival rates in patients with the same stage of AGC [3, 4]. Recently, lymphovascular invasion (LVI) has been shown to be associated with poor surgical outcomes in patients with gastric cancer [3–7]. LVI, which is referred to as lymphatic and/or blood vessel invasion, is an essential step to disseminating tumour cells [8, 9], and it holds a significant risk for regional lymph node metastasis [3]. However, it rarely can be evaluated preoperatively [10].
As a common preoperative examination, multiphasic dynamic CT has been shown to be an effective tool for assessing tumour angiogenesis by quantitative enhancement measurement [2, 11–13]. Several studies have shown that tumour neovascularization is related to LVI in patients with GC [2, 7]. However, there are limited data on the correlation between preoperative CT parameters and LVI. Although Yin et al. reported that contrast enhancement ratio (CER) of the arterial phase in GC was correlated with microvascular invasion, their study included only 64 patients and did not consider other potentially confounding factors such as clinicopathological characteristics [14]. Komori et al. showed that the tumour-to-normal wall enhancement ratio in the arterial phase was correlated with LVI, but their study did not obtain non-contrast CT scans for the evaluation of the relative tumour enhancement ratio, which might introduce bias in their results [2].
Therefore, the purpose of this study is to investigate the diagnostic value of multiphasic dynamic CT-derived parameters for prediction of LVI in AGC. Furthermore, the associations between the CT predictors and tumour histological differentiation and Lauren classification were evaluated.
Materials and methods
Patient population
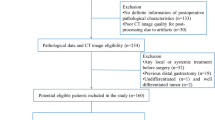
This retrospective study was approved by the institutional ethics committee of Guangdong General Hospital, and formal consent was not required for this study.
A total of 431 consecutive patients underwent gastrectomy with regional lymphadenectomy for AGC between January 2010 and December 2015 in our Hospital. Inclusion criteria for these patients were: (i) endoscopic biopsy-proven untreated GC; (ii) visible GC on preoperative contrast-enhanced CT; and (iii) histologically confirmed gastric adenocarcinoma. 153 patients were excluded for the following reasons: absence of preoperative gastroscopy or contrast-enhanced CT in this hospital (n = 63), poor visualisation of the tumour due to insufficient distension or peristaltic motion of the stomach (n = 44), limited area to draw regions of interest (ROIs) owing to too small tumour size (n = 24), and previous distal gastrectomy (n = 22). Finally, 278 patients were included into our study (190 men, 88 women; age range, 28–90 years; median age, 60 years, interquartile range, 51–67 years).
CT protocol
Among the 278 patients, CT was performed (i) with an 8-channel multi-detector CT scanner (Lightspeed; GE Healthcare, Hino, Japan) (n = 32) or (ii) with a 64-channel multi-detector CT scanner (Lightspeed VCT; GE Healthcare, Milwaukee, WI, USA) (n = 246). Before CT scanning, all patients fasted for more than 5 h and were administered an intramuscular injection of 20 mg of scopolamine (Buscopan, Boehringer Ingelheim) to minimise bowel peristalsis. All the patients were advised to drink 600–1,000 ml of water 30 min before examination. Scanning covered the entire stomach region during a single breath-hold with the patient supine. Imaging acquisition parameters were as follows: 120 kVp; 130 mAs; 0.5 s rotation time; detector collimation: 8 × 0.625 mm or 64 × 0.625 mm; field of view (FOV) 350 × 350 mm; matrix 512 × 512.
Following routine non-enhanced CT, multiphasic contrast-enhanced CT scans were obtained 25–30 s (arterial phase), 60 s (portal phase) and 180 s (delayed phase) after an infusion of 1.5 ml/kg of iodinated contrast material (Ultravist 370, Bayer Schering Pharma, Berlin, Germany) at a rate of 3.5 ml/s with an automatic power injector (Ulrich CT Plus 150, Ulrich Medical, Ulm, Germany). Images were displayed with a section thickness of 1.25 and 5.0 mm; the former was used for tumour volume measurement and the latter was used for measurement of CT values.
CT images analysis
The CT images were retrospectively analysed by a radiologist (C.L.) with 8 years of experience in gastrointestinal CT imaging interpretation. The observer was blinded to the clinicopathological data but was aware that the patients had AGC. The lesion was determined to be cancerous when the gastric wall showed focal thickening of ≥6 mm [15]. After localisation of the gastric lesion on the CT images using multi-planar reconstruction, the circular ROIs of approximately 8–25 mm2 were placed on the maximal section of the tumours in each phase. The ROIs were drawn to encompass the area of greatest enhancement among one of the three contrast-enhanced phases maximally, but limited to one-half the diameter of the thick gastric wall (Fig. 1) [2]. Vessel structures, ulceration and necrosis should not be involved in the ROIs. Next, the same size ROIs were placed in approximately the same site of the tumour on images of the other two contrast-enhanced phases and the non-enhanced image. Meanwhile, tumour mean attenuation values in Hounsfield units (HUs) of the ROIs were recorded.
Measurement of attenuation value of the tumour in a 61-year-old woman with gastric adenocarcinoma with lymphovascular invasion in the cardia. The circular regions of interest (ROIs) were positioned on the maximal section of the tumours in each phase. The tumour ROI was drawn to encompass the subsurface area of greatest enhancement among one of the three contrast-enhanced phases (the portal phase in this case), but limited to one-half the diameter of the thick gastric wall. Vessel structures, ulceration and necrosis should not be involved in the ROIs. Next, the same size ROI was copied onto the CT images of the same slice in the other two contrast-enhanced phases. (A) The mean attenuation value of the lesion is 36 HU in the non-contrast phase. (B) The mean attenuation value of the lesion is 103 HU in the arterial phase. (C) In the portal phase, the mean attenuation value of the lesion is 128 HU. (D) In the delayed phase, the mean attenuation value of the lesion is 104 HU
In addition, to eradicate patient-related confounding factors such as cardiac function and scanner factors such as fluctuations in kVp [16], we measured the attenuation value of the spleen as another reference standard to compare to the tumour CT attenuation value in the portal phase. Two ROIs of the same size were drawn in the homogeneous spleen parenchyma (visible vasculatures were excluded) on the maximal section of the spleen to generate an averaged spleen CT value.
To verify the intra-observer reproducibility of the CT value measurements, all the measurements were repeated 2 weeks later by the same observer in the same way in a random order for all the patients.
The CT attenuation values of the tumour in the non-enhanced (arterial, portal, delayed) phase were recorded as ValueNON (ValueAP, ValuePP, ValueDP), and of the spleen in the portal phase as Value spleen.
With the ValueNON and Valuespleen as the reference, post-contrast tumorous attenuation difference (ΔAP, ΔPP, ΔDP) and the difference between tumour and spleen (ΔT-S), CER and tumour-to-spleen ratio (TSR) were calculated according to the following formulae:
where T-S in ΔT-S and CERT-S indicates tumour-to-spleen.
In addition, the gross tumour volumes (GTVs) were measured on the basis of portal phase CT images to identify whether GTVs were associated with LVI. Another radiologist (X.H.), with 7 years of experience in gastrointestinal imaging, manually outlined the visible tumours on each slice on the open software 3D Slicer (version 4.3, http://www.slicer.org), and GTVs were automatically calculated.
Pathological evaluation
Pathological tumour differentiation as one of the preoperative indicators was evaluated by endoscopic biopsy according to the WHO Classification of Tumours of the Digestive System (2010 version). In addition, the Lauren classification [17], which includes diffuse type, intestinal type and mixed type, was also determined preoperatively in our hospital.
After surgery, all gastric specimens were processed according to standard pathological procedures. All slides were analysed for LVI by pathologists with expertise in gastric pathology and were blinded to imaging findings. LVI was defined as the presence of tumour emboli within either the lymphatic or vascular channels [6]. Vascular channels have not been differentiated from lymphatic vessels owing to the difficulty and unsatisfactory reproducibility in clinical practice [9].
Statistical analysis
In this study, the patients were divided into groups of ‘with LVI’ and ‘without LVI’. For categorical variables such as patient gender (female or male), age at the time of surgery (≤60 or >60 years) [4], tumour location (lower third, middle third, upper third or two-thirds or more) [18], tumour differentiation (well/moderate, poor/undifferentiated), Lauren classification (intestinal, diffuse or mixed), and preoperative carcinoembryonic antigen (CEA; normal or elevated (CEA value >5 ng/ml)) were analysed with the chi-square test between the two groups.
For continuous variables, data are expressed as the mean ± standard deviation (M ± SD). Normality was tested using the Kolmogorov-Smirnov method, and variance homogeneity was then tested with the Levene’s test.
A paired Student’s t test was performed to evaluate the systematic bias of repeated ROI measurements; if there was no significant difference between the two measurements, the mean values of the ROIs were calculated for further analysis. Moreover, the intraclass correlation coefficient (ICC) was used to assess the intra-observer reproducibility of CT value measurements. An ICC >0.75 was regarded as being in good agreement [19]. Tumour CT-derived parameters between the two groups were compared using the independent t test or Mann-Whitney U test, where appropriate.
The independent predictors for LVI were identified and their combination was built by multivariate logistic regression analysis, using the significant variables from the univariate analysis as inputs. In addition, receiver operating characteristic (ROC) curve analyses were performed to determine the area under the curve (AUC), accuracy, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV).
Furthermore, associations between CT predictors for LVI and tumour histological differentiation and Lauren classification were analysed using the chi-square test.
Statistical analyses were performed with SPSS Statistics (version 22.0, IBM Corporation, Armonk, NY, USA). A p value < 0.05 was considered to be statistically significant.
Results
The histopathological results showed that 167 patients had LVI (60.07%) and 111 patients did not have LVI (39.93%).
Clinicopathological characteristics of the patients
The results of the univariate analysis for clinicopathological characteristics are presented in Table 1. The Lauren classification and histological grade showed a statistically significant association with LVI. Diffuse type and poorer histological grade showed a higher tendency for LVI in AGC.
With regard to gender, age, tumour location and CEA level, there were no statistically significant differences between the two groups (Table 1).
Intra-observer reproducibility of CT value measurements
No significant differences were observed between two repeated measurements of CT value measured by the same observer (P = 0.219–0.648). ICC (95% CI) for ValueNON, ValueAP, ValuePP, ValueDP and Valuespleen varied from 0.885 (0.856–0.907) to 0.974 (0.968–0.979). All of them were in good agreement. Therefore, we calculated the mean CT values in different phases for further analysis.
Comparison of CT-derived parameters between the two groups
The results of the univariate analysis for CT-derived parameters between the two groups are presented in Table 2. The mean tumour CT values in patients with LVI were significantly higher in both the portal and delayed phases (both P < 0.001).
When using tumour non-enhanced CT attenuation values as a reference standard, the CT attenuation difference (Δ) and the CERs were significantly higher in the group with LVI than in those in the group without LVI (all P < 0.001), except for ΔAP (P = 0.086).
With regard to the CT attenuation values of spleens in the portal phase (Valuespleen), there were no significant differences between the two groups (Table 2). Using the spleen as a reference standard, ΔT-S and TSR were significantly higher in the group with LVI (P < 0.001).
In addition, GTVs showed no significant difference between the two groups (Table 2).
Multivariate analysis of preoperative indicators for patients with and without LVI
In multivariate analysis, only ΔPP (odds ratio (OR), 1.056; 95% CI: 1.032–1.080) and ΔT-S (OR, 1.043; 95% CI: 1.020–1.066) were the independent predictors for LVI (both P < 0.001), which are presented in Table 3. Higher ΔPP and higher ΔT-S showed statistically significant associations with the presence of LVI (Table 3).
Diagnostic performance of CT predictors and their combination
The diagnostic performance of ΔPP, ΔT-S, and their combination are listed in Table 4. Although ΔPP showed relatively higher accuracy and sensitivity, the specificity of detection of LVI was relatively lower than that of ΔT-S and their combination. The combination of ΔPP and ΔT-S achieved a relatively higher AUC (0.800), specificity (77.8%) and PPV (82.1%) than those of ΔPP and ΔT-S.
ROC analysis of ΔPP, ΔT-S and their combination for the prediction of LVI in AGC is shown in Fig. 2.
Receiver operator characteristics (ROC) analysis in patients with and without LVI. (A) ROC curve demonstrates how use of a ΔPP cutoff of 59.5 HU helps differentiate positive LVI cases from negative LVI cases. (B) ROC curve demonstrates how use of a ΔT-S cutoff of −18.50 HU helps differentiate positive LVI cases from negative LVI cases. (C) ROC curve demonstrates how use of a combination cutoff of −0.142 helps differentiate positive LVI cases from negative LVI cases
Association of pathological characteristics with CT predictors for LVI
Although histological grade and Lauren classification were not the independent predictors for LVI, they showed a statistically significant association with LVI (Table 1). To further clarify the pathological characteristics of the CT predictors for LVI, associations between the CT predictors (ΔPP and ΔT-S) with tumour histological differentiation and Lauren classification are shown in Table 5. Poorer histological grade and diffuse type showed a statistically significant association with the group of higher ΔPP or ΔT-S (Table 5).
Discussion
This study demonstrated that tumour enhancement measured with preoperative multiphasic dynamic CT was a non-invasive, quantitative method that could predict LVI in patients with AGC, of which ΔPP and ΔT-S were independent predictors for LVI in AGC, with acceptable predictive performance, which could be improved by their combination.
Yin et al. showed that CERAP was associated with microvascular invasion (p = 0.01) in univariate analysis, which was consistent with our results. Previous studies indicated that the VEGF family induced both angiogenesis and lymphangiogenesis actively [20], and tumour neovascularization was closely related to LVI in patients with GC [21, 22]. Theoretically, the arterial phase, which reflected vasclularity and haemodynamic change [23], might reflect the presence of LVI. However, our study showed that CERAP was not an independent predictor for LVI, a point which was not fully understood and needs further study to address.
The mean CT attenuation value of AGC in the portal phase reported by Tsurumaru et al. was 117.1 HU, which was greater than that in our study (106.6 HU). The difference may be explained by the different CT acquisition time and smaller size in their study (n = 24) [13]. In our study, ΔPP and ΔT-S were significantly higher in the group with LVI. The results might be explained as follows: LVI occurs when tumour cells infiltrate and destroy the vascular and/or lymphatic structures and form vascular cancer emboli [9]. It is known that portal enhancement reflects the diffusion of contrast medium in the interstitial space [23]. Destruction of lymphovascular structures may increase the microvascular permeability, which can account for higher a CT value in the portal phase.
As the most common classification systems for gastric adenocarcinoma, histological differentiation and Lauren classification have been reported to be significantly correlated with the presence of LVI [4], which is in accordance with our results. Our study also showed that AGC of diffuse type and poorer histological grade had higher ΔPP or ΔT-S.
Although an attractive technique to assess permeability, perfusion CT is infrequently used in gastric cancer for the following reasons: first, the mean radiation dose of perfusion CT is higher than conventional CT; second, there is restricted anatomical coverage in the z-axis of older CT machines; third, artefacts due to respiration; and fourth, the anatomical structure and physiological characteristics of the stomach [24]. Although researchers have proposed using perfusion CT to assess angiogenesis and malignancy in GC, they reported varied results. For example, Asami Satoh et al. reported a decrease in tumour perfusion with increasing level of malignancy in terms of histological differentiation and Lauren classification [25]. However, some studies showed higher blood perfusion and permeability changes in poorly differentiated GC [26, 27]. In contrast to perfusion CT, dual energy CT, which enables quantification of tumour perfusion based on iodine-related attenuation, can be performed within a single breath-hold without increasing radiation dose compared with a single-energy CT protocol. One drawback of this technology is the increased cost of maintenance fees due to the larger x-ray tube [28]. Dynamic contrast-enhanced (DCE) MRI can also be used to evaluate haemodynamic features; however, a longer scanning time, higher cost and some contraindications result in limited use of this technique [28, 29]. To our knowledge, there are no studies that have addressed the relationship between perfusion/dual energy CT or DCE-MRI with LVI. Therefore, further studies are needed to compare multiphasic dynamic CT with emerging CT technologies or DCE-MRI to establish a priority method to predict LVI in patients with AGC.
In previous studies, tumours with larger diameters have been shown to be the preoperative predictor for LVI in hepatocellular carcinoma [4, 10]. However, unidirectional measurements carriy high variability. There were some studies reported that volume measurement could compensate for this shortcoming [10, 30]. Our study is the first to compare GTVs between the two groups with and without LVI in AGC. Unexpectedly, there was no significant correlation between GTVs and LVI status of AGC in the present study.
There are several limitations in our study. First, we could not completely avoid a site-by-site bias when placing ROIs on the CT images in all phases. However, as the gastric wall involved by cancer was stiff and peristalsis disappeared, the tumours were compared with themselves instead of the normal gastric wall in our study. In addition, by encouraging patients to maintain breath-hold during scanning, the mismatches of ROIs were maximally controlled. Second, we did not assess inter-observer agreement by multiple reviewers, although intra-observer agreement was shown to be good in our study. Third, there was an interval of only 2 weeks between the two repeated CT value measurements in this study, which might involve memory bias. An interval time of at least 3 months would be optimal. However, previous studies have reported variable interval times of 1 week or more. Finally, because this was a retrospective study with unintended selection bias, the cut-off of the CT predictors for LVI must be verified in a further prospective study.
In conclusion, quantitative enhancement measurement during multiphasic dynamic CT, such as ΔPP, ΔT-S and their combination, may serve as surrogate markers for detecting LVI preoperatively. Patients with suspected positive LVI might need an aggressive treatment plan such as adjuvant chemotherapy or a greater extent of surgery [23, 31].
Abbreviations
- AGC:
-
Advanced gastric cancer
- AUC:
-
Area under the curve
- CEA:
-
Carcinoembryonic antigen
- CER:
-
Contrast enhancement ratio
- GTV:
-
Gross tumour volume
- HU:
-
Hounsfield unit
- ICC:
-
Intraclass correlation coefficient
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- ROC:
-
Receiver operator characteristics
- ROI:
-
Region of interest
- TSR:
-
Tumour-to-spleen ratio
References
Songun I, Putter H, Kranenbarg EM, Sasako M, van de Velde CJ (2010) Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol 11:439–449
Komori M, Asayama Y, Fujita N et al (2013) Extent of arterial tumor enhancement measured with preoperative MDCT gastrography is a prognostic factor in advanced gastric cancer after curative resection. AJR Am J Roentgenol 201:W253–W261
Ahmad R, Setia N, Schmidt BH et al (2016) Predictors of Lymph Node Metastasis in Western Early Gastric Cancer. J Gastrointest Surg 20:531–538
Li P, He HQ, Zhu CM et al (2015) The prognostic significance of lymphovascular invasion in patients with resectable gastric cancer: a large retrospective study from Southern China. BMC Cancer 15:370
Talamonti MS, Kim SP, Yao KA et al (2003) Surgical outcomes of patients with gastric carcinoma: the importance of primary tumor location and microvessel invasion. Surgery 134:720–727
Dicken BJ, Graham K, Hamilton SM et al (2006) Lymphovascular Invasion Is Associated With Poor Survival in Gastric Cancer. Ann Surg 243:64–73
Maehara Y, Kabashima A, Koga T et al (2000) Vascular invasion and potential for tumor angiogenesis and metastasis in gastric carcinoma. Surgery 128:408–416
Padera TP, Kadambi A, di Tomaso E et al (2002) Lymphatic metastasis in the absence of functional intratumor lymphatics. Science 296:1883–1886
Kikuchi E, Margulis V, Karakiewicz PI et al (2009) Lymphovascular invasion predicts clinical outcomes in patients with node-negative upper tract urothelial carcinoma. J Clin Oncol 27:612–618
Chou CT, Chen RC, Lee CW, Ko CJ, Wu HK, Chen YL (2012) Prediction of microvascular invasion of hepatocellular carcinoma by pre-operative CT imaging. Br J Radiol 85:778–783
Kim SH, Kim CS, Kim MJ, Cho JY, Cho SH (2016) Differentiation of clear cell renal cell carcinoma from other subtypes and fat-poor angiomyolipoma by use of quantitative enhancement measurement during three-phase MDCT. Am J Roentgenol 206:W21–W28
Lee-Felker SA, Felker ER, Tan N et al (2014) Qualitative and Quantitative MDCT Features for Differentiating Clear Cell Renal Cell Carcinoma From Other Solid Renal Cortical Masses. Am J Roentgenol 203:W516–W524
Tsurumaru D, Miyasaka M, Nishimuta Y et al (2015) Differentiation of early gastric cancer with ulceration and resectable advanced gastric cancer using multiphasic dynamic multidetector CT. Eur Radiol 26:1330–1337
Yin XD, Huang WB, Lu CY, Zhang L, Wang LW, Xie GH (2011) A preliminary study on correlations of triple-phase multi-slice CT scan with histological differentiation and intratumoral microvascular/lymphatic invasion in gastric cancer. Chin Med J (Engl) 124:347–351
Kim HJ, Kim AY, Oh ST et al (2005) Gastric cancer staging at multi-detector row CT gastrography: comparison of transverse and volumetric CT scanning. Radiology 236:879–885
Rockall AG, Sohaib SA, Evans D et al (2003) Hepatic steatosis in Cushing's syndrome: a radiological assessment using computed tomography. Eur J Endocrinol 149:543–548
Lauren P (1965) The two histological main types of gastric carcinoma: Diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand 64:31–49
Liang YX, Deng JY, Guo HH et al (2013) Characteristics and prognosis of gastric cancer in patients aged >/= 70 years. World J Gastroenterol 19:6568–6578
Busing KA, Kilian AK, Schaible T, Debus A, Weiss C, Neff KW (2008) Reliability and validity of MR image lung volume measurement in fetuses with congenital diaphragmatic hernia and in vitro lung models. Radiology 246:553–561
Holopainen T, Bry M, Alitalo K, Saaristo A (2011) Perspectives on lymphangiogenesis and angiogenesis in cancer. J Surg Oncol 103:484–488
Tomoda M, Maehara Y, Kakeji Y, Ohno S, Ichiyoshi Y, Sugimachi K (1999) Intratumoral neovascularization and growth pattern in early gastric carcinoma. Cancer 85:2340–2346
Maehara Y, Kakeji Y, Oda S, Baba H, Sugimachi K (2001) Tumor growth patterns and biological characteristics of early gastric carcinoma. Oncology 61:102–112
Kim H, Park MS, Choi JY et al (2009) Can microvessel invasion of hepatocellular carcinoma be predicted by pre-operative MRI? Eur Radiol 19:1744–1751
Yao J, Yang ZG, Chen TW, Li Y, Yang L (2010) Perfusion changes in gastric adenocarcinoma: evaluation with 64-section MDCT. Abdom Imaging 35:195–202
Satoh A, Shuto K, Okazumi S et al (2010) Role of perfusion CT in assessing tumor blood flow and malignancy level of gastric cancer. Dig Surg 27:253–260
Sun ZQ, Cheng XF, Ge YX et al (2015) Role of CT perfusion imaging in patients with variously differentiated gastric adenocarcinoma. J Xray Sci Technol 23:737–744
Zongqiong S, Xiaohong L, Wei C et al (2016) CT perfusion imaging of the stomach: a quantitative analysis according to different degrees of adenocarcinoma cell differentiation. Clin Imaging 40:558–562
Sieren JC, Ohno Y, Koyama H, Sugimura K, McLennan G (2010) Recent technological and application developments in computed tomography and magnetic resonance imaging for improved pulmonary nodule detection and lung cancer staging. J Magn Reson Imaging 32:1353–1369
Dong Y, Lei GW, Wang SW, Zheng SW, Ge Y, Wei FC (2014) Diagnostic value of CT perfusion imaging for parotid neoplasms. Dentomaxillofac Radiol 43:20130237
Lee SM, Kim SH, Lee JM et al (2009) Usefulness of CT volumetry for primary gastric lesions in predicting pathologic response to neoadjuvant chemotherapy in advanced gastric cancer. Abdom Imaging 34:430–440
Mori N, Mugikura S, Takasawa C et al (2016) Peritumoral apparent diffusion coefficients for prediction of lymphovascular invasion in clinically node-negative invasive breast cancer. Eur Radiol 26:331–339
Acknowledgements
The scientific guarantor of this publication is Zaiyi Liu. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
This study received funding from the National Natural Scientific Foundation of China (No. 81271569, No. 81601469 and NO.U1301258).
No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Study subjects or cohorts have not been previously reported. Methodology: retrospective diagnostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Additional information
Zelan Ma and Changhong Liang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Ma, Z., Liang, C., Huang, Y. et al. Can lymphovascular invasion be predicted by preoperative multiphasic dynamic CT in patients with advanced gastric cancer?. Eur Radiol 27, 3383–3391 (2017). https://doi.org/10.1007/s00330-016-4695-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4695-6