Abstract
Objectives
Our aim was to provide further evidence for the efficacy/safety of radioembolization using yttrium-90-resin microspheres for unresectable chemorefractory liver metastases from colorectal cancer (mCRC).
Methods
We followed 104 consecutively treated patients until death. Overall survival (OS) was calculated from the day of the first radioembolization procedure. Response was defined by changes in tumour volume as defined by Response Evaluation Criteria in Solid Tumours (RECIST) v1.0 and/or a ≥30 % reduction in serum carcinoembryonic antigen (CEA) at 3 months.
Results
Survival varied between 23 months in patients who had a complete response to prior chemotherapy and 13 months in patients with a partial response or stable disease. Median OS also significantly improved (from 5.8 months to 17.1 months) if response durability to radioembolization extended beyond 6 months. Patients with a positive trend in CEA serum levels (≥30 % reduction) at 3 months post-radioembolization also had a survival advantage compared with those who did not: 15.0 vs 6.7 months. Radioembolization was well tolerated. Grade 3 increases in bilirubin were reported in 5.0 % of patients at 3 months postprocedure.
Conclusions
After multiple chemotherapies, many patients still have a good performance status and are eligible for radioembolization. This single procedure can achieve meaningful survivals and is generally well tolerated.
Key Points
• After multiple chemotherapies, many patients are still eligible for radioembolization (RE).
• RE can achieve meaningful survival in patients with chemorefractory liver-predominant metastatic colorectal cancer (mCRC).
• Tumour responsiveness to prior systemic treatments is a significant determinant of overall survival (OS) after RE.
• Radioembolization in patients with a good performance status is generally well tolerated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most prevalent cancer worldwide and is the cause of 11.6 % and 13.0 % of all cancer deaths in men and women, respectively [1]. For patients with unresectable metastatic disease (mCRC), palliation with fluoropyrimidine in various combinations and schedules with oxaliplatin and/or irinotecan and new biological agents have evolved to provide substantially improved median survivals [2] and a meaningful window for localized control of liver metastases [especially if extrahepatic disease (EHD) appears to have an indolent clinical course]. Metastases in the liver is a common presentation [3] and is prognostic for mortality in these patients [4].
Liver-directed approaches are used to treat either discrete visually targeted tumours (using resection, ablation, irreversible electroporation, stereotactic body radiation therapy) or more widespread multinodular disease in the liver using radioembolization (or selective internal radiation therapy) or transarterial chemoembolization (either conventional or with drug-eluting beads) [5–10]. There is encouraging evidence to suggest that there might be a potential synergy between systemic therapy and the use of locoregional approaches to improve outcomes in liver-predominant mCRC [11–13], and the value of a multidisciplinary approach employing the skills of the interventional radiologists and radiation oncologists in this setting is recognized by the most recent guidelines from the European Society for Medical Oncology [14] .
The aim of this paper is to provide further evidence for the efficacy and safety of radioembolization based on the long-term follow-up of >100 patients with unresectable chemorefractory liver metastases from CRC.
Materials and methods
Patients
Consecutive patients with unresectable chemotherapy-refractory liver metastases from CRC who received radioembolization were retrospectively analyzed. All patients had documented progression, mainly in the liver, following prior treatment with fluoropyrimidine-, oxaliplatin- and irinotecan-based regimens with or without antiepidermal growth factor receptor (EGFR) and antivascular endothelial growth factor therapies (VEGF).
Suitable candidates for radioembolization were selected by our interdisciplinary tumour review board, and written informed consent was provided for analyses of these data. Patients were eligible for radioembolization if they had an absence of significant progressive extrahepatic disease, a tumour burden in the liver of <50 % of total liver volume, and hepatic arterial anatomy that would enable safe delivery of radioembolization to the liver only. Patients with limited hepatic reserve, ascites, or other clinical signs of liver failure (total bilirubin level >2.0 mg/dl in the absence of a reversible cause; serum albumin <3.0 g/dl), compromised bone marrow or renal function, or other severe comorbidities (e.g., chronic obstructive or chronic restrictive pulmonary disease, including dyspnea at rest from any cause) were generally considered unsuitable for radioembolization.
Radioembolization
Yttrium-90 (90Y) is a pure beta emitter that decays to stable zirconium-90 with an average energy of 0.94 MeV (half-life 2.67 days), with a mean tissue penetration of 2.5 mm and a maximum range of 11 mm. The principle of radioembolization is based on the preferential vascular distribution of radioactive microspheres within the tumour vasculature, which allows delivery of high doses of 90Y with relative sparing of normal liver parenchyma.
Before the radioembolization was undertaken, meticulous coeliac and superior mesenteric angiography was conducted to map the hepatic arterial tree and to detect and occlude, using microcoil embolization, every collateral vessel that arose from the hepatic artery that could lead to extrahepatic deposition of microspheres.
At a second hepatic arterial catheterization conducted separately after the therapy-planning arteriography, 90Y resin-microspheres (SIR-Spheres; Sirtex Medical Ltd, Sydney, Australia) suspended in sterile water were injected under intermittent fluoroscopic visualization, alternating with contrast medium, to assess for preserved antegrade hepatic arterial flow. The prescribed activity, calculated using the body surface area method based on target volumes of tumour and liver for each patient [15], was administered as either whole liver, lobar, or sequential lobar treatment according to tumour burden [16]. Within 24 h of therapy, single photon emission computed tomography (SPECT) scans were performed to confirm microsphere target deposition.
Data collection and analysis
Results from hematologic, liver function, blood biochemistry tests, and physical examination were recorded prior to the first radioembolization procedure (baseline) and at all subsequent follow-up visits. Patients resumed a routine schedule of laboratory tests and clinical examination at day 1-3 after 1, 6, 12, and 24 weeks. The nature and severity of any changes in liver function recorded and any other clinically significant grade ≥3 adverse events using the National Cancer Institute Common Toxicity Criteria Adverse Events version 3.0 (CTC v3) [17]. Survival was calculated from the day of the first radioembolization procedure to the day of death or last follow-up. Patients were censored at the time of last follow-up if their status could not be established. Response was defined according to the RECIST criteria in 3-month intervals using computed tomography (CT) and magnetic resonance imaging (MRI) and additionally as a ≥30 % reduction in serum carcinoembryonic antigen (CEA) at 3 months compared with pretreatment values according to RECIST [18].
Statistical analyses were conducted using SAS version 9.2 XP Pro statistical analyses software (SAS Institute Inc., Cary, NC, USA). Variables of interest were calculated using descriptive statistics. Summary statistics for continuous variables included mean, median, standard deviation (SD), interquartile range (IQR), minimum and maximum, and 95 % confidence intervals (CI), as appropriate. Categorical data were summarized by frequency distributions with percentage-based on nonmissing data. Nonparametric estimates of median survival and 95 % CI were computed using Kaplan-Meier product-limit method. Univariate proportional hazards models were utilized to estimate the effects of covariates on time-to-event, as determined by the hazard ratio and 95 % CI.
Results
Patients and treatment
In this analysis, 104 consecutive chemorefractory patients with mCRC received radioembolization for progressive disease in the liver; 52.3 % of patients also had evidence of limited extrahepatic disease progression at the time of radioembolization (Table 1). All patients were followed up until death. Prior chemotherapy consisted mostly of fluoropyrimidine-based treatment combined with oxaliplatin or irinotecan. In addition, 46.2 % of patients had received prior treatment with bevacizumab and/or cetuximab.
A median of 94.6 % of the planned 90Y activity [1.6 GBq (IQR 0.5) of 1.8 GBq (IQR 0.4)] was delivered to patients, mostly as a whole-liver treatment. Mean ± SD lung shunting was 4.9 % ± 2.3 (range 1.0–12.0 %).
Overall survival
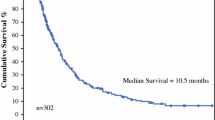
Median OS was 10.2 months (95 % CI 7.8–13.0), which did not differ significantly by gender or age. Median OS was similar regardless of duration (≥ or <24 months) between diagnosis of CRC (or liver metastases) and radioembolization (Table 2). However, the presence of extrahepatic disease or substantial tumour liver involvement (<25 % vs. ≥ 25 %) at the time of radioembolization were adverse prognostic factors, although there was only a trend toward reduced OS in patients with extrahepatic disease (p = 0.052).
Median OS post-radioembolization was significantly prolonged in patients who had a good response to prior chemotherapy, defined by either changes in tumour volume (according RECIST 1.0) or CEA (response or stable disease vs. no response) (Fig. 1). Moreover, if durability of response to radioembolization extended to ≥6 months (as in 45 of 104 patients; 43.3 %), median survival was 17.1 months (95 % CI 13.7–23.7) compared with 5.8 months (95 % CI 13.7–23.7) in patients who had disease progression within 6 months of treatment. Median OS also significantly improved (from 5.8 months to 17.1 months) if the durability of response to radioembolization extended >6 months.
Kaplan-Meier analysis showed that median OS decreased significantly with increasing severity of pretreatment laboratory parameters (beyond CTC grade 0) for aspartate transaminase (AST), gamma-glutamyl transferase (GGT), and total bilirubin, although patients with total bilirubin (beyond pretreatment CTC grade 0) were in the minority (27.5 % of patients) compared with AST (49.5 %) or GGT (89.2 %).
Safety and tolerability
Radioembolization with 90Y resin microspheres was generally well tolerated. The most commonly reported observed adverse event the days after the procedure were fatigue (14.4 %) and abdominal pain (8.7 %). Gastric ulcer due to the suspected extrahepatic deposition of microspheres was reported in three patients (2.9 %) and cholecystitis in two (1.9 %); all occurred early following radioembolization and resolved with treatment. Regarding liver-related events, raised bilirubin (all grades) was recorded in 26.9 % of patients at baseline, increasing to 50.0 % of patients at month 3 post-radioembolization. Clinically significant radioembolization-induced liver disease (REILD) was not reported, and grade 3 increases in bilirubin were reported in a minority (5.0 %) of patients at month 3. Raised AST levels (all grades) were more common events at both baseline (43.9 %) and at month 3 (72.0 %) than changes in bilirubin; however, grade 3 increases in AST were reported in only 1.3 % of patients at month 3.
Discussion
This analysis provides further evidence for the safety and efficacy of radioembolization in liver-predominant mCRC. Our findings equate to the observations from centers in the USA [19, 20], Europe [21], and Australia [22], which reported median OS following radioembolization were consistently ≥10 months in patients who had exhausted most, if not all, conventional chemotherapy options.
Uniquely, our analysis also showed that tumour responsiveness to prior systemic treatment (and not duration since diagnosis of mCRC) was a significant determinant of median OS after radioembolization; OS varied between 23 months in patients who had a complete response to prior chemotherapy and 13 months in patients with a partial response or stable disease (according to RECIST). These data suggest that response to chemotherapy is a useful clinical marker of tumour biology [4]. Median OS also significantly improved (from 5.8 to 17.1 months) if the durability of response to radioembolization extended >6 months. Patients with a positive trend in CEA serum levels (≥30 % reduction) at 3 months post-radioembolization also had a survival advantage compared with those who did not. This fits with the fundamental premise of liver-directed therapies, in which the aim of treatment is to slow the course of disease in the liver, which may be predictive of prolonged survival [23]. Several previously published studies on radioembolization have demonstrated the value decreasing CEA as a marker of reduced tumour metabolic function, correlating with findings from positron emission tomography (PET)-CT, and decreased tumour load [24, 25].
Pretreatment markers of disease progression in the liver characterized by changes in liver-cell function (as measured by albumin and AST) and in the biliary tract (as measured by alkaline phosphatase (ALPase, GGT, and bilirubin) are not only prognostic for OS following radioembolization but predictive of treatment outcome with chemotherapy [26–28].
Of interest in the contemporary management of mCRC is the value of radioembolization as either an alternative, or as an add-on therapy, to either EGFR or VEGF receptor inhibitors. Our analyses showed a trend toward improved survival in patients who had not received prior bevacizumab or cetuximab (16 vs. 10 months). Data from the recent
Randomized phase III trial comparing first-line mFOLFOX6 ± bevacizumab (bev) versus mFOLFOX6 + selective internal radiation therapy (SIRT) ± bev in patients (pts) with metastatic colorectal cancer (mCRC) (SIRFLOX) study indicate that the combination of bevacizumab with chemotherapy and radiotherapy was an effective and well-tolerated strategy in prolonging the time to tumour progression in the liver compared with chemotherapy plus bevacizumab alone. Moreover, radioembolization may also be a potentially useful therapy as an alternative to EGFR receptor inhibitors (especially in patients with KRAS mutant genotype).
REILD to normal liver reserve is transient and not fatal; however, some deaths have been reported in patients with progressive liver failure attributed to REILD and not tumour progression. The likelihood of this potentially fatal event can be ameliorated by appropriate selection of patients and correct delivery and calculation of 90Y activity. In our analyses of 104 patients, clinically significant REILD was not reported, and grade 3 increases in bilirubin were evident from routine laboratory investigations only in a minority (5.0 %) of patients at 3 months posttreatment. This is consistent with recent findings from the Metastatic Colorectal Cancer Liver Metastases Outcomes after RadioEmbolization (MORE) case-control study at 11 US centers, where REILD was an uncommon event using today’s carefully defined treatment protocols (all grades, 1.7 %; grade ≥3, 0.5 %) [29].
There remains limited published evidence on the efficacy and safety of transarterial chemoembolization [both conventional and irinotecan-loaded drug-eluting beads (DEBIRI)] in mCRC, making comparison with radioembolization in this setting difficult. To date, a two-armed prospective clinical trial has been published by Fiorentini and colleagues involving 74 patients randomly assigned to receive either DEBIRI (n = 36) or conventional 5-fluorouracil, leucovorin, and irinotecan (FOLFIRI) therapy (n = 38) [9, 30] and a single-arm study [31] of DEBIRI (n = 50). Data from these studies are encouraging, but variability of enrolment criteria (first line, second line, salvage) and significant differences in technique and dose intensity of IRI (high variation of the dose of irinotecan loaded on particles) impede interpretation of these data [8]. Our own limited experience of DEBIRI, a finding also reflected in the literature [32], is that this technique is not as well tolerated by patients as radioembolization and so is viewed less favorably in the palliative setting.
Although our analysis provides robust evidence for patient OS following radioembolization, the analysis has a number of limitations due to its retrospective nature. Notably, however, all data were collated prospectively in consecutive patients receiving radioembolization and so are representative of the usual candidates for this procedure in clinical practice. However, our analysis does not detail all prior chemotherapy regimens and also lacks the rigor of a clinical trial in terms of reporting adverse events.
In conclusion, there remains a high medical need for effective treatments in the chemorefractory setting. Even after multiple lines of chemotherapy, many patients still have a good performance status and are fit and eligible for radioembolization. In our view, this single treatment procedure affords substantial benefits and is generally well tolerated.
References
IARC IAfRoC (2014) GLOBOCAN: estimated incidence, mortality and prevalence worldwide in 2012 (population fact sheet in more developed countries). Copyright: IARC, Lyon, France. http://globocan.iarc.fr/Pages/fact_sheets_population.aspx. Last accessed January 2014
Cartwright TH (2012) Treatment decisions after diagnosis of metastatic colorectal cancer. Clin Colorectal Cancer 11:155–166
Elferink MA, de Jong KP, Klaase JM, Siemerink EJ, de Wilt JH (2015) Metachronous metastases from colorectal cancer: a population-based study in North-East Netherlands. Int J Color Dis 30:205–212
Ribero D, Vigano L, Amisano M, Capussotti L (2013) Prognostic factors after resection of colorectal liver metastases: from morphology to biology. Future Oncol 9:45–57
Clark ME, Smith RR (2014) Liver-directed therapies in metastatic colorectal cancer. J Gastrointest Oncol 5:374–387
Mi K, Kalady MF, Quintini C, Khorana AA (2015) Integrating systemic and surgical approaches to treating metastatic colorectal cancer. Surg Oncol Clin N Am 24:199–214
Fiorentini G, Aliberti C, Mulazzani L et al (2014) Chemoembolization in colorectal liver metastases: the rebirth. Anticancer Res 34:575–584
Liu DM, Thakor A, Baerlocher M et al (2015) A review of conventional and drug-eluting chemoembolization in the treatment of colorectal liver metastases: principles and proof. Future Oncology (London, England). doi:10.2217/fon.15.3:1-8
Fiorentini G, Aliberti C, Tilli M et al (2012) Intra-arterial infusion of irinotecan-loaded drug-eluting beads (DEBIRI) versus intravenous therapy (FOLFIRI) for hepatic metastases from colorectal cancer: final results of a phase III study. Anticancer Res 32:1387–1395
de Baere T, Tselikas L, Pearson E et al (2015) Interventional oncology for liver and lung metastases from colorectal cancer: the current state of the art. Diagn Interv Imaging. doi:10.1016/j.diii.2015.04.004
Hendlisz A, Van den Eynde M, Peeters M et al (2010) Phase III trial comparing protracted intravenous fluorouracil infusion alone or with yttrium-90 resin microspheres radioembolization for liver-limited metastatic colorectal cancer refractory to standard chemotherapy. J Clin Oncol 28:3687–3694
Van Hazel G, Blackwell A, Anderson J et al (2004) Randomised phase 2 trial of SIR-Spheres plus fluorouracil/leucovorin chemotherapy versus fluorouracil/leucovorin chemotherapy alone in advanced colorectal cancer. J Surg Oncol 88:78–85
Kennedy AS (2014) Radiation oncology approaches in liver malignancies. Am Soc Clin Oncol Educ Book e150–e155. doi:10.14694/EdBook_AM.2014.34.e150
Van Cutsem E, Cervantes A, Nordlinger B, Arnold D (2014) Metastatic colorectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 25:iii1–iii9
Ahmadzadehfar H, Biersack HJ, Ezziddin S (2010) Radioembolization of liver tumors with yttrium-90 microspheres. Semin Nucl Med 40:105–121
Jakobs TF, Hoffmann RT, Tatsch K, Trumm C, Reiser MF, Helmberger TK (2007) Developments and perspectives in radioablative techniques. Radiologe 47:1083–1088
Institute NC (2006) Common terminology criteria for adverse events v3.0. http://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm
Chalian H, Tore HG, Horowitz JM, Salem R, Miller FH, Yaghmai V (2011) Radiologic assessment of response to therapy: comparison of RECIST Versions 1.1 and 1.0. Radiographics 31:2093–2105
Kennedy AS, Coldwell D, Nutting C et al (2006) Resin 90Y-microsphere brachytherapy for unresectable colorectal liver metastases: modern USA experience. Int J Radiat Oncol Biol Phys 65:412–425
Kennedy A, Ball D, Cohen Sea (2013) Safety and efficacy of resin 90Y-microspheres in 548 patients with colorectal liver metastases progressing on systemic chemotherapy. ASCO Gastrointestinal Cancers Symposium:Abs. 264
Cosimelli M, Golfieri R, Pennington B, Sennfält K (2013) Selective internal radiotherapy (SIRT) using resin yttrium-90 resin microspheres for chemotherapy-refractory metastatic colorectal cancer: an Italian cost-effectiveness analysis. Value Health 16:A409
Saxena A, Meteling B, Kapoor J, Golani S, Morris DL, Bester L (2015) Is yttrium-90 radioembolization a viable treatment option for unresectable, chemorefractory colorectal cancer liver metastases? A large single-center experience of 302 patients. Ann Surg Oncol 22:794–802
Chapiro J, Duran R, Lin M et al (2015) Early survival prediction after intra-arterial therapies: a 3D quantitative MRI assessment of tumor response after TACE or radioembolization of colorectal cancer metastases to the liver. Eur Radiol 25:1993–2003
Hipps D, Ausania F, Manas DM, Rose JD, French JJ (2013) Selective Interarterial Radiation Therapy (SIRT) in colorectal liver metastases: how do we monitor response? HPB Surg 2013:570808
Fendler WP, Ilhan H, Paprottka PM et al (2015) Nomogram including pretherapeutic parameters for prediction of survival after SIRT of hepatic metastases from colorectal cancer. Eur Radiol 25:2693–2700
Dixon MR, Haukoos JS, Udani SM et al (2003) Carcinoembryonic antigen and albumin predict survival in patients with advanced colon and rectal cancer. Arch Surg 138:962–966
Graf W, Bergstrom R, Pahlman L, Glimelius B (1994) Appraisal of a model for prediction of prognosis in advanced colorectal cancer. Eur J Cancer 30a:453–457
Maisano R, Azzarello D, Del Medico P et al (2011) Alkaline phosphatase levels as a prognostic factor in metastatic colorectal cancer treated with the FOLFOX 4 regimen: a monoinstitutional retrospective study. Tumori 97:39–42
Kennedy AS, Ball D, Cohen SJ et al (2015) Multicenter evaluation of the safety and efficacy of radioembolization in patients with unresectable colorectal liver metastases selected as candidates for (90)Y resin microspheres. J Gastrointest Oncol 6:134–142
Aliberti C, Fiorentini G, Muzzio PC et al (2011) Trans-arterial chemoembolization of metastatic colorectal carcinoma to the liver adopting DC Bead(R), drug-eluting bead loaded with irinotecan: results of a phase II clinical study. Anticancer Res 31:4581–4587
Martin RC, Joshi J, Robbins K et al (2011) Hepatic intra-arterial injection of drug-eluting bead, irinotecan (DEBIRI) in unresectable colorectal liver metastases refractory to systemic chemotherapy: results of multi-institutional study. Ann Surg Oncol 18:192–198
Stutz M, Mamo A, Valenti D et al (2015) Real-life report on chemoembolization using DEBIRI for liver metastases from colorectal cancer. Gastroenterol Res Pract 2015:715102
Acknowledgments
The scientific guarantor of this publication is PD Dr. med. Tobias Jakobs. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding.
Prof. Wieland Sommer (MPH) kindly provided statistical advice for this manuscript. Institutional Review Board approval was obtained. Written informed consent was obtained from all patients. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Additional information
T. F. Jakobs and K. J. Paprottka contributed equally to this work.
Rights and permissions
About this article
Cite this article
Jakobs, T.F., Paprottka, K.J., Raeßler, F. et al. Robust evidence for long-term survival with 90Y radioembolization in chemorefractory liver-predominant metastatic colorectal cancer. Eur Radiol 27, 113–119 (2017). https://doi.org/10.1007/s00330-016-4345-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4345-z