Abstract
Objectives
To detect symptomatic hemispheres during the postoperative course of subarachnoid haemorrhage (SAH) using arterial spin labelling (ASL).
Methods
Eighteen patients with aneurysmal SAH were included; four exhibited symptomatic vasospasm postoperatively. All patients underwent ASL on days 9–10 (single time-point ASL). Nine patients underwent serial measurements of ASL (serial ASL) on days 1–2, 9–10 and 13–21, and seven patients also underwent imaging on days 4–7. CBF in the posterior part of the MCA territory was measured, and the ipsilateral/contralateral ratio of CBF was calculated. Differences between symptomatic hemispheres and others underwent ROC analysis.
Results
Single time-point ASL revealed that CBFday9-10 and CBFi/c_day9-10 were significantly lower in symptomatic hemispheres than in asymptomatic hemispheres (P < 0.001). Serial ASL was significantly decreased on CBFday4-7 compared with CBFday1-2 and on CBFday9-10 compared with CBFday4-7, and significantly increased on CBFday13-21 compared with CBFday9-10. ROC analysis of single time-point ASL revealed that AUC for CBFday9-10 was 0.95, significantly higher than CBFi/c_day9-10 (P < 0.001). ROC analysis of serial ASL showed that AUC for CBFday9-10 was 0.93 and significantly higher than CBFday9-10/day1-2 and CBFi/c_day9-10 (P < 0.001).
Conclusions
Single time-point ASL revealed significant CBF reduction in symptomatic hemispheres compared with asymptomatic hemispheres. Serial ASL showed time-dependent CBF changes after SAH.
Key Points
• MR arterial spin labelling (ASL) can non-invasively assess cerebral blood flow (CBF)
• ASL revealed significant CBF reduction in symptomatic hemispheres compared with asymptomatic hemispheres
• Serial ASL measurements enable observation of time-dependent CBF changes after SAH
• ASL is non- invasive and suitable for serial repeated examinations
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Angiographic vasospasm occurs in 30–70 % of patients with aneurysmal subarachnoid haemorrhage (SAH), with a typical onset of 3–5 days after haemorrhage, maximal narrowing at 5–14 days, and gradual resolution over 2–4 weeks [1]. However, the risk of symptomatic vasospasm remains between 20–40 %, and vasospasm has been thought to be associated with delayed ischaemic neurological deficits. Approximately 15–20 % of patients suffer stroke or die of vasospasm during the postoperative course [2].
Imaging studies including diffusion-weighted imaging (DWI) and perfusion-weighted imaging (PWI) or magnetic resonance (MR) imaging [3, 4], single photon emission computed tomography [5], positron emission tomography (PET) [6], and computed tomography (CT) have been reported to be advantageous in guiding the management of the vasospasm [1]. However, diagnostic accuracy varies with time, and serial measurements are necessary. Transcranial Doppler ultrasound (TCD) can be performed repeatedly, but covers only the middle cerebral artery (MCA), and a meta-analysis found no evidence for TCD as a valid method for diagnosing vasospasm [7]. Many centres continue to rely on cerebral angiography for the diagnosis of vasospasm [1].
Arterial spin labelling (ASL) has been introduced as a non-invasive method capable of assessing cerebral blood flow (CBF) [8]. ASL can be performed without administration of contrast media or exposure to radiation, allowing repeated measurements. The purpose of this study was thus to evaluate CBF in patients with aneurysmal SAH during the postoperative course using ASL and to examine the capabilities of ASL for diagnosing vasospasm.
Patients and methods
This study was approved by the local institutional review board, and written informed consent was obtained from all patients or their families. The group of participants comprised 18 patients with aneurysmal SAH treated in our hospital (4 men, 14 women; mean age, 62.2 ± 11.2 years). Patient characteristics are provided in Table 1. Fourteen patients underwent surgical clipping and four underwent endovascular coiling. Treatment was conducted within 24 h of onset for all patients. Metallic materials were not applied in cranioplasty for surgical clipping as far as possible in order to avoid metallic artefact over cortices on ASL.
Symptomatic vasospasm was defined as any new neurological deficit presenting after onset of SAH, confirmed and explained by angiographic findings, and not explained by other causes of neurological deterioration (rebleeding, hydrocephalus, electrolyte disturbances, hypoxia, or seizure). Four symptomatic patients were examined with conventional cerebral angiography when symptoms became apparent. Angiography confirmed vasospasm in all four symptomatic patients at least at the posterior trunk of the ipsilateral MCA. The other 14 asymptomatic patients were not examined using conventional angiography. The laterality was determined by the location of the ruptured aneurysm. When the aneurysm was located in the midline, the side with more subarachnoid haemorrhage was termed as ipsilateral.
Imaging protocol
Patients underwent MR imaging using a 3-T system (Magnetom Verio; Siemens, Erlangen, Germany) with a 32-channel phased array head coil. Day 0 was designated the day of SAH onset. All patients underwent ASL measurement on days 9–10 (single time-point ASL). Nine patients had three serial ASL measurements on days 1–2, 9–10 and 13–21 (serial ASL). Seven also had an ASL measurement on days 4–7. Several additional measurements of ASL were performed when necessary. ASL on days 1–2 was considered to represent baseline postoperative CBF. Restless and/or uncooperative patients were sedated as necessary.
Imaging parameters
Pulsed ASL was performed using the second version of the quantitative imaging of perfusion with thin-slice TI periodic saturation (Q2TIPS) [9]. Imaging parameters were as follows: repetition time, 3,000 ms; echo time, 14 ms; field of view, 256 × 256 mm; matrix, 64 × 64 pixels; slice thickness, 8 mm; interslice gap, 2 mm; 9 slices; partial Fourier acquisition rate, 7/8; TI1, 700 ms; TI1s, 1,600 ms; TI2, 1,800 ms; 45 pairs of labelled and unlabelled images. For quantitation, the following values were used: λ (brain/blood partition coefficient of water), 0.9 g/ml; α (inversion efficiency), 0.95; T1a (longitudinal relaxation time of arterial blood), 1,496.19 ms. Other routine imaging sequences including DWI, T2-weighted imaging, and MR angiography were performed as needed.
Image data analysis
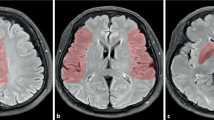
The CBF images were created on the MR operating system. DICOM data of ASL images were transferred to an off-line workstation. ASL images were anatomically normalised using iNeurostat software (Nihon Medi-Physics, Tokyo, Japan). Region of interest (ROI) analysis was automatically performed for normalised CBF images based on vascular territories, and ROIs were placed on each slice; average CBF values for each ROI were calculated (Fig. 1) [10]. ROIs of the posterior parts of MCA territories were adopted and the number of ROIs was 26 for each hemisphere.
Box-and-whisker plots of CBF for all ROIs involving the posterior parts of MCA territories on days 9–10 (CBFday9-10) were calculated for each subject to evaluate single time-point ASL measurements, and three percentiles (25th, 50th and 75th) were determined. For serial ASL, plots of CBF for all ROIs in the posterior parts of MCA territories in nine patients were also created for days 1–2 (CBFday1-2), days 4–7 (CBFday4-7), days 9–10 (CBFday9-10), and day 13–21 (CBFday13-21). In two patients, no ASL imaging was conducted on days 4–7 and the values of seven patients were thus used. When ASL was performed multiple times during days 13–21, ASL of the latest day was adopted.
For CBFday9-10, CBF ratios of ipsilateral to contralateral sides of ruptured aneurysms (CBFi/c_day9-10) were derived for both single and serial ASL. Ratios of CBF (days 9-10) against baseline ASL (days 1-2) were also calculated (CBF day9-10/day1-2) for serial ASL.
Statistical analysis
CBFday9-10 for single time-point ASL was compared between symptomatic and asymptomatic hemispheres using one-way analysis of variance in all 18 patients, followed by Tukey’s post-hoc test. Distal MCA ROIs were selected, because vasospasm was confirmed at the posterior trunk of the ipsilateral MCA in all four symptomatic patients on conventional angiography. ROIs of both symptomatic as well as asymptomatic hemispheres were compared in the statistical analysis. ROIs at the ipsilateral hemisphere of symptomatic patients were assigned to symptomatic hemispheres. ROIs at the contralateral hemisphere of symptomatic patients and ROIs at both hemispheres of asymptomatic patients were assigned to asymptomatic hemispheres.
Concerning serial ASL, changes among CBFday1-2, CBFday4-7, CBFday9-10 and CBFday13-21 of both hemispheres were compared using the Games-Howell test for nine patients (7 patients for CBFday4-7).
Receiver-operating characteristic (ROC) curve analysis was conducted to detect CBF decreases in distal MCA areas for CBFday9-10 and CBFi/c_day9-10 with single time-point ASL, and for CBFday9-10, CBFi/c_day9-10 and CBFday9-10/day1-2 with serial ASL. Areas under the curve (AUCs) for CBFday9-10, CBFi/c_day9-10, and CBFday9-10/day1-2 were analysed using a non-parametric approach [11]. The positive predictive value (PPV) and negative predictive value (NPV) for symptomatic vasospasm were derived from ROC analysis. Values of P < 0.05 were considered indicative of a statistically significant difference. SPSS version 15 software (IBM Japan, Tokyo, Japan) was used for all statistical analyses.
Results
Box-and-whisker plots of CBFday9-10 and CBFi/c_day9-10 for single time-point ASL are shown in Fig. 2a and b. The three percentiles (25th, 50th and 75th) for CBFday9-10 were 19.34, 22.63, and 25.21 ml/100 g/min for symptomatic hemispheres and 30.13, 35.76, and 43.60 ml/100 g/min for asymptomatic hemispheres, respectively (P < 0.001) (Fig. 2a). The three percentiles (25th, 50th, and 75th) for CBFi/c_day9-10 were 0.55, 0.65, and 0.79 for symptomatic hemispheres and 0.87, 1.01, and 1.19 for asymptomatic hemispheres, respectively (P < 0.001) (Fig. 2b). Box-and-whisker plots of CBF for serial ASL are shown in Fig. 3. The three percentiles (25th, 50th, and 75th) were 41.99, 49.42, and 55.90 ml/100 g/min for CBFday1-2, 33.70, 41.13, and 48.75 ml/100 g/min for CBFday4-7, 29.67, 36.26 and 45.79 ml/100 g/min for CBFday9-10, and 37.87, 40.26, and 53.59 ml/100 g/min for CBFday13-21, respectively (Fig. 3). All P values were less than 0.05 except for CBFday4-7 compared with CBFday13-21 (P = 0.849) (Table 2).
Box-and-whisker plot for CBFday9-10 and CBFi/c_day9-10. The three percentiles (25th, 50th, 75th) for ROIs of CBFday9-10 are 19.34, 22.63, and 25.21 ml/100 g/min for symptomatic hemispheres and 30.13, 35.76, and 43.60 ml/100 g/min for asymptomatic hemispheres, respectively (P < 0.001) a The three percentiles (25th, 50th, and 75th) of CBFi/c_day9-10 are 0.55, 0.6, and 0.79 for symptomatic hemispheres and 0.87, 1.01, and 1.19 for asymptomatic hemispheres, respectively (P < 0.001) (b)
Box-and-whisker plot for CBF with serial ASL. The three percentiles (25th, 50th, 75th) for ROIs of CBF are 41.99, 49.42, and 55.90 ml/100 g/min for CBFday1-2, 33.70, 41.13, and 48.75 ml/100 g/min for CBFday4-7, 29.67, 36.26, and 45.79 ml/100 g/min for CBFday9-10, and 37.87, 40.26, and 53.59 ml/100 g/min for CBFday13-21. P values are less than 0.05 except between CBFday4-7 and CBFday13-21 (P = 0.849). A gradual CBF reduction is observed from CBFday1-2 to CBFday9-10, and recovery of CBF on CBFday13-21 to nearly equal to CBFday4-7 is observed
The ROC analysis for single time-point ASL revealed that AUCs for CBFday9-10 and CBFi/c_day9-10 were 0.95 and 0.89 (P < 0.001) (Fig. 4). The optimal cutoff for CBFday9-10 was 26.9 ml/100 g/min (sensitivity, 90.38 %; specificity, 93.89 %; PPV, 46.53 %; NPV, 99.40 %). ROC analysis of serial ASL measurements showed AUCs for CBFday9-10, CBFday9-10/day1-2, and CBFi/c_day9-10 of 0.93, 0.87, and 0.86, respectively (Fig. 5). The optimal cutoff for CBFday9-10 was 26.9 ml/100 g/min (sensitivity, 90.38 %; specificity, 92.31 %; PPV, 59.49 %; NPV, 98.71 %). P values from ROC analyses were as follows: CBFday9-10 vs. CBFi/c_day9-10, P < 0.001; CBFday9-10 vs. CBFday9-10/day1-2, P < 0.001; and CBFi/c_day9-10 vs. CBFday9-10/day1-2, P = 0.832.
ROC analysis for single time-point ASL revealed that AUCs of CBFday9-10 and CBFi/c_day9-10 are 0.95 and 0.89. This indicates that CBFday9-10 is a better parameter for predicting CBF reduction than CBFi/c_day9-10. The optimal cutoff for CBFday9-10 is 26.9 ml/100 g/min (sensitivity, 90.38 %; specificity, 93.89 %; PPV, 46.53 %; NPV, 99.40 %)
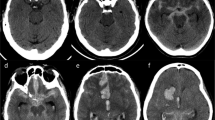
Representative cases of symptomatic patients (Figs. 6 and 7) and an asymptomatic patient (Fig. 8) are shown with serial CBF changes at multiple ROIs for the posterior parts of the MCA.
A 67-year-old woman with symptomatic vasospasm (case 15). Clipping for the right IC–PC aneurysm was performed on day 0. The patient had been conscious without motor weakness after surgery until day 6. Left-sided hemiplegia, sensory disturbance, and hemispatial neglect appeared on day 7. ASL immediately after the occurrence of these symptoms revealed decreased CBF in the right MCA territory, particularly in the distal slices (upper row) (a). Conventional angiography revealed vasospasm in the M1 segment of the right MCA. Repeated endovascular treatment was performed, and temporal improvement of MCA stenosis and paralysis was achieved, but left-sided hemiparalysis remained. Serial ASL measurements show gradual decreases in CBF even before the onset of symptoms and increasing hyperintensity on DWI (lower row) (a). A propensity towards a relative CBF decrease is seen in distal slices (b). Fluctuating CBF is shown on the left side, and a slight CBF decrease is shown in distal slices on day 8 (c). Note that DWI was not obtained for days 4 and 6. Proximal slices are displayed in black and distal slices in grey
A 77-year-old woman with symptomatic vasospasm (case 17). Clipping for right IC–PC aneurysm was performed on day 0. She had been well with no motor weakness except mild drowsiness until day 8. Left-sided hemiplegia and sensory disturbance occurred on day 9. ASL immediately after the occurrence of symptoms revealed decreased CBF in the right MCA territory, particularly in distal slices (upper row) (a). Conventional angiography revealed vasospasm in the M2 segment of the right MCA. Repeated endovascular treatment was performed, achieving a temporary improvement in paralysis. Unfortunately, left-sided hemiplegia deteriorated between days 10 and 13, and MR imaging was not performed during this interval. DWI (lower row) shows a hyperintense area in the posterior part of the right MCA territory on day 13 (a). Serial ASL measurements show gradual CBF decreases even before symptom onset and a propensity toward a relative CBF decrease in the distal slices (b). A slight CBF decrease is shown on the left side (c). Proximal slices are displayed in black and distal slices in grey
An asymptomatic 65-year-old woman (case 12). Emergency endovascular coiling for basilar aneurysm was performed on day 0. She had been under sedation with spinal drainage for SAH. After gradual recovery from drowsiness, no apparent neurological focal deficits were identified during the postoperative course. ASL shows no apparent decrease in CBF (upper row) and DWI (lower row) reveals no abnormalities (a). Serial ASL shows a mild CBF decrease around day 9, but to no less than 30 ml/100 g/min (b, c). Proximal slices are displayed in black and distal slices in grey
Discussion
Single time-point ASL revealed a significant CBF reduction in the posterior parts of the MCA territory in symptomatic hemispheres compared with asymptomatic hemispheres on days 9–10. Decreased CBF associated with vasospasm will lead to cerebral infarction and delayed ischaemic neurological deficits (DIND). As the upper part of the pyramidal tract is fed by the long insular artery from the insular segment of the MCA and/or medullary arteries from the opercular and cortical segments of the MCA [12], a CBF decrease in the MCA territory due to vasospasm might cause motor weakness. As observed in the cases presented in Figs. 6 and 7, areas of decreased CBF were larger than the high-intensity areas on DWI for symptomatic patients, suggesting that ASL reveals an ischaemic penumbra. However, additional study is necessary to confirm this possibility, given the relatively small number of symptomatic patients in this study.
Our results showed that CBFday9-10 can predict CBF reduction in the posterior part of the MCA territory better than CBFi/c_day9-10. This suggests that CBF reduction on the contralateral side increased CBFi/c_day9-10, which may indicate that weak vasospasm also occurred contralaterally [13].
Serial ASL revealed the value of CBF to be decreased to the order of CBFday1-2, CBFday4-7, and CBFday9-10, and increased for CBFday13-21, confirming that serial ASL imaging is useful for monitoring vasospasm, although CBFday9-10/day1-2 was less predictable than CBFday9-10. Vasospasm represents the most important cause of DIND, because early aneurysm surgery has been reported to decrease the risk of rebleeding [14]. Intensive prophylactic therapy for vasospasm such as hypervolaemia, hypertension, and haemodilution (triple-H) is preferable for impaired CBF [15]. A PET study showed a wide variation in CBF patterns for patients with vasospasm, ranging from reduced to normal to hyperaemic [6], because PET studies are usually performed only once during the postoperative course. Serial ASL imaging in the present study showed a gradual decrease in CBF before clinical symptoms or DWI abnormalities became evident, consistent with previous reports of DWI-PWI mismatch in vasospasm [4, 16]. Serial ASL may help us to understand temporal changes in vasospasm for each patient and to select the timing for the treatment of vasospasm, such as endovascular treatment and CSF drainage [17, 18]. ASL is less invasive than MR/CT perfusion and suitable for repeated examinations, because ASL can measure CBF without any administration of contrast media or exposure to radiation.
Serial ASL also showed recovery from impaired CBF. Triple-H therapy has been widely performed, but the hypertension and hypervolaemia with such therapy may increase the risks of cardiac failure, electrolyte abnormality and cerebral oedema [1]. Hypertension and hypervolaemia therapy can be less intensive, if serial ASL shows improvement of CBF, although additional investigation is necessary to evaluate the therapeutic effects of serial ASL.
We focussed on ROIs for the posterior part of the MCA territory in this study. This was because metallic artefacts derived from aneurysm clips severely affected CBF values for ROIs placed at the anterior part of the MCA territory. The purpose of this study was to diagnose vasospasm after SAH, so this selection was considered inevitable, and we chose a feasible imaging protocol and processing method. However, several limitations to this study must be considered when interpreting the results. Serpiginous high signal was sometimes observed when labelled blood did not reach the capillary bed and remained in the artery, representing delayed artery transit artefacts [19]. Vasospasm occurs not only in the proximal artery segment, but also in the distal artery or even in intraparenchymal arterioles [20]. This increases the cerebral circulation time [21] and causes artery transit artefacts in ASL. In this context, CBF measured by ASL may not represent the true CBF, but serial ASL is still a useful tool for detecting vasospasm, because delayed artery transit indicates delayed artery circulation.
Another limitation is that symptoms might have developed around days 9-10. There has been no prospective study featuring vasospasm on ASL in the literature according to our knowledge. Therefore, we firstly focussed on the visualisation of cerebral ischaemia caused by vasospasm on ASL. It might have been helpful to have set the day for ASL imaging before day 9-10. However, the purpose of this study was to investigate visualisation of vasospasm, and early detection and prediction of vasospasm would be another study. Additional studies with more patients will be necessary to determine the lowest CBF and calculate the diagnostic performance of serial ASL for vasospasm.
Another limitation is that ASL images were not coregistered to three-dimensional (3D) anatomical images. Coregistration to 3D anatomical images is widely applied in image analysis [22], but 3D anatomical images were not obtainable because of the increased imaging time required conflicting with the need to minimise the time spent by ill patients in the MR unit. As we used ROI analysis, a small degree of misregistration may not have had a great effect on the results.
To increase the precision of perfusion quantification, the signal evolution after arterial labeling needs to be sampled at more than two points in time [23]. Multi-inversion time (TI) imaging could have been helpful for quantifying CBF; however, TI imaging requires longer imaging times for equivalent SNR [24]. Several reports demonstrated that single TI is sensitive to identification of abnormalities because of its high sensitivity to delay [25, 26]. Delayed arterial arrival time will lead to a decrease of CBF on ASL, which will add some advantage for the detection of vasospasm after aneurysmal SAH.
The last limitation is that the posterior part of MCA territory provides a very small window for evaluation of perfusion differences. Because conventional angiography confirmed vasospasm of at the posterior trunk of the MCA in all four symptomatic patients, we targeted posterior part of the MCA. Additional comparison studies are necessary to evaluate the entire brain perfusion after aneurysmal SAH.
In conclusion, single ASL revealed significant decreases in CBF for the posterior parts of the MCA territory in hemispheres with symptomatic vasospasm compared with asymptomatic hemispheres on days 9–10. Serial ASL detected a tendency towards CBF reduction related to vasospasm during the postoperative course of aneurysmal SAH.
References
Bederson JB, Connolly ES Jr, Batjer HH et al (2009) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the stroke council, American Heart Association. Stroke 40:994–1025
Weidauer S, Lanfermann H, Raabe A, Zanella F, Seifert V, Beck J (2007) Impairment of cerebral perfusion and infarct patterns attributable to vasospasm after aneurysmal subarachnoid hemorrhage: a prospective MRI and DSA study. Stroke 38:1831–1836
Condette-Auliac S, Bracard S, Anxionnat R et al (2001) Vasospasm after subarachnoid hemorrhage: interest in diffusion-weighted MR imaging. Stroke 32:1818–1824
Ohtonari T, Kakinuma K, Kito T, Ezuka I, Kanazawa T (2008) Diffusion-perfusion mismatch in symptomatic vasospasm after subarachnoid hemorrhage. Neurol Med Chir (Tokyo) 48:331–336, discussion 336
Egge A, Sjoholm H, Waterloo K, Solberg T, Ingebrigtsen T, Romner B (2005) Serial single-photon emission computed tomographic and transcranial doppler measurements for evaluation of vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurgery 57:237–242, discussion 237-242
Minhas PS, Menon DK, Smielewski P et al (2003) Positron emission tomographic cerebral perfusion disturbances and transcranial Doppler findings among patients with neurological deterioration after subarachnoid hemorrhage. Neurosurgery 52:1017–1022, discussion 1022-1014
Lysakowski C, Walder B, Costanza MC, Tramer MR (2001) Transcranial doppler versus angiography in patients with vasospasm due to a ruptured cerebral aneurysm: a systematic review. Stroke 32:2292–2298
Deibler AR, Pollock JM, Kraft RA, Tan H, Burdette JH, Maldjian JA (2008) Arterial spin-labeling in routine clinical practice, part 1: technique and artifacts. AJNR Am J Neuroradiol 29:1228–1234
Luh WM, Wong EC, Bandettini PA, Hyde JS (1999) QUIPSS II with thin-slice TI1 periodic saturation: a method for improving accuracy of quantitative perfusion imaging using pulsed arterial spin labeling. Magn Reson Med 41:1246–1254
Ogura T, Hida K, Masuzuka T, Saito H, Minoshima S, Nishikawa K (2009) An automated ROI setting method using NEUROSTAT on cerebral blood flow SPECT images. Ann Nucl Med 23:33–41
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Kumabe T, Higano S, Takahashi S, Tominaga T (2007) Ischemic complications associated with resection of opercular glioma. J Neurosurg 106:263–269
Rabinstein AA, Weigand S, Atkinson JL, Wijdicks EF (2005) Patterns of cerebral infarction in aneurysmal subarachnoid hemorrhage. Stroke 36:992–997
Ross N, Hutchinson PJ, Seeley H, Kirkpatrick PJ (2002) Timing of surgery for supratentorial aneurysmal subarachnoid haemorrhage: report of a prospective study. J Neurol Neurosurg Psychiatry 72:480–484
Sen J, Belli A, Albon H, Morgan L, Petzold A, Kitchen N (2003) Triple-H therapy in the management of aneurysmal subarachnoid haemorrhage. Lancet Neurol 2:614–621
Rordorf G, Koroshetz WJ, Copen WA et al (1999) Diffusion- and perfusion-weighted imaging in vasospasm after subarachnoid hemorrhage. Stroke 30:599–605
Alaraj A, Charbel FT, Amin-Hanjani S (2009) Peri-operative measures for treatment and prevention of cerebral vasospasm following subarachnoid hemorrhage. Neurol Res 31:651–659
Tanaka K, Minami H, Kota M, Kuwamura K, Kohmura E (2005) Treatment of cerebral vasospasm with intra-arterial fasudil hydrochloride. Neurosurgery 56:214–223, discussion 214-223
Chalela JA, Alsop DC, Gonzalez-Atavales JB, Maldjian JA, Kasner SE, Detre JA (2000) Magnetic resonance perfusion imaging in acute ischemic stroke using continuous arterial spin labeling. Stroke 31:680–687
Uhl E, Lehmberg J, Steiger HJ, Messmer K (2003) Intraoperative detection of early microvasospasm in patients with subarachnoid hemorrhage by using orthogonal polarization spectral imaging. Neurosurgery 52:1307–1315, discussion 1315-1307
Beck J, Raabe A, Lanfermann H et al (2006) Effects of balloon angioplasty on perfusion- and diffusion-weighted magnetic resonance imaging results and outcome in patients with cerebral vasospasm. J Neurosurg 105:220–227
Kiebel SJ, Ashburner J, Poline JB, Friston KJ (1997) MRI and PET coregistration–a cross validation of statistical parametric mapping and automated image registration. Neuroimage 5:271–279
Gunther M, Bock M, Schad LR (2001) Arterial spin labeling in combination with a look-locker sampling strategy: inflow turbo-sampling EPI-FAIR (ITS-FAIR). Magn Reson Med 46:974–984
Zaharchuk G, Do HM, Marks MP, Rosenberg J, Moseley ME, Steinberg GK (2011) Arterial spin-labeling MRI can identify the presence and intensity of collateral perfusion in patients with moyamoya disease. Stroke 42:2485–2491
Xie J, Gallichan D, Gunn RN, Jezzard P (2008) Optimal design of pulsed arterial spin labeling MRI experiments. Magn Reson Med 59:826–834
Zaharchuk G, Bammer R, Straka M et al (2009) Arterial spin-label imaging in patients with normal bolus perfusion-weighted MR imaging findings: pilot identification of the borderzone sign. Radiology 252:797–807
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aoyama, K., Fushimi, Y., Okada, T. et al. Detection of symptomatic vasospasm after subarachnoid haemorrhage: initial findings from single time-point and serial measurements with arterial spin labelling. Eur Radiol 22, 2382–2391 (2012). https://doi.org/10.1007/s00330-012-2511-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-012-2511-5