Abstract
Purpose of Review
Acute spontaneous subarachnoid haemorrhage (SAH) is a severe disease, frequently complicated by vasospasm and delayed cerebral ischaemia (DCI), which have a negative impact on prognosis. Imaging studies are essential in the diagnosis of SAH. In this article, we review the available imaging techniques for prediction, monitoring and diagnosis of these complications of SAH.
Recent Findings
Non-contrast computed tomography (CT) and transcranial Doppler (TCD) have been so far the mainly used techniques to evaluate SAH patients during the acute stage of disease and to screen for vasospasm and DCI. However, there have been new developments of brain imaging techniques, with the introduction of automated methods to quantify blood volume and cerebral flow velocities, and the use of perfusion studies that could contribute to predict or diagnose such complications. Magnetic resonance (MR) imaging studies are proving useful to evaluate early brain injury and to diagnose DCI. Newer angiography suites have sophisticated post-processing tools that quantify cerebral haemodynamics in SAH and may provide important clues for the diagnosis of vasospasm.
Summary
Imaging studies are part of the standard management of patients with acute SAH. Blood quantification on CT and the evaluation of cerebral flow velocities on TCD are known to predict and monitor the occurrence of vasospasm. DCI has increasingly been recognized as the most clinically relevant complication of SAH but also the most difficult to predict. MR imaging is the most sensitive tool to diagnose DCI. Future developments in imaging are needed to predict this important complication and help to improve the prognosis of patients with SAH.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spontaneous (non-traumatic) subarachnoid haemorrhage (SAH) is responsible for approximately 5% of strokes, with an incidence of 7.2–10.5 per 100,000 person-years [1, 2]. It is most frequently caused by a ruptured intracranial aneurysm and carries high morbidity and mortality [3••]. Aneurysmal SAH is associated with significant pre-hospital mortality (reaching 50% in some series) and overall mortality of 18–67% [4, 5]. Complications of aneurysmal SAH such as vasospasm and delayed cerebral ischaemia (DCI) contribute for this elevated mortality and poor clinical outcome.
Vasospasm is defined as a narrowing of cerebral vessels, caused by contraction and hyperplasia of the muscular layer, not attributable to atherosclerosis or vessel hypoplasia, and can be diagnosed in angiographic imaging studies, such as digital subtraction angiography (DSA) [6, 7]. Angiographic vasospasm develops in up to 70% of patients after SAH, occurring most frequently at 6 to 8 days after aneurysm rupture and extending up to 14–21 days [8, 9]. The reduction of arterial diameter is thought to reduce cerebral perfusion and cause ischaemia. Microvascular spasm has also been described following aneurysmal SAH, and is not easily identified with current imaging techniques [10••].
DCI is defined as the development of a neurological deficit and/or the presence of ischaemic lesions on imaging studies, not immediately present after SAH, not related to treatment of the aneurysm, and not attributable to other causes [6, 7]. DCI occurs in about 30% of patients and is associated with worse clinical and cognitive prognosis [6]. The pathophysiology of DCI is multifactorial, and arterial vasospasm is only one of the contributors [10]. Angiographic vasospasm is not invariably associated with ischaemia, and cerebral infarction may originate in territories unaffected by vasospasm [11]. Therefore, monitoring the appearance of vasospasm exclusively would address only part of the problem. Nonetheless, prediction of both vasospasm and DCI is challenging and has been the focus of several studies, in an effort for improving the outcome of SAH patients.
Thanks to the development of new techniques and improvement of current imaging modalities, imaging studies play a growing role in prediction and diagnosis of these complications and in the management of SAH patients. This review focused on different imaging modalities and their role in predicting and assessing vasospasm and DCI.
Early imaging predictors of vasospasm and DCI
Computed tomography
Computed tomography (CT) is the first imaging study used for the diagnosis of acute SAH. CT is a widely available technique, with short scanning times and possibility of sequential complementary angiographic evaluation with CT angiography (CTA), allowing for swift diagnosis and treatment decisions. In the first 6 h after SAH, the diagnostic sensitivity of non-contrast brain CT scan is approximately 100% [12]. CTA has shown a sensitivity of approximately 98% in identifying intracranial aneurysms, and when combined, CT and CTA can diagnose aneurysmal SAH with greater than 99% sensitivity [13]. In addition to diagnosing SAH and screening the presence of aneurysm, initial imaging can provide some clues to predict the development of vasospasm and DCI (Table 1).
Quantification of cisternal blood is an important prognostic tool, and several scales have been developed for this purpose (Table 2). The widely used Fisher scale [18] and modified Fisher scale [14], as well as the more complex Hijdra scale [48], correlate the amount of blood and presence of intraventricular haemorrhage (IVH) to the risk of vasospasm, DCI and clinical outcome (Fig. 1) [14, 15, 18, 22, 23•, 48]. Of these rater-dependent scales, the Hijdra scale has proven to have the best inter-observer agreement [49]. The presence of IVH appears to be particularly relevant in predicting clinical vasospasm/DCI and outcome. Studies have shown that the combination of IVH and SAH is associated with worst outcome compared to IVH or SAH alone [19, 24, 50]. Semi-quantitative scores for IVH measurement exist, such as the Graeb score [51] and the modified Graeb score [52]. The latter has been shown to hold similar discrimination for DCI when compared to the modified Fisher scale, and, interestingly, combining these two scales in a dichotomized scale seems to improve prediction of DCI [25]. The presence of ICH is also an important predictor of DCI and unfavourable outcome [26, 53]. Acute hydrocephalus diagnosed in acute imaging has also been shown to associate to angiographic vasospasm and to negatively influence outcome [30, 54••].
Admission non-contrast CT scan of acute spontaneous SAH in five different patients, illustrating different grades of the Fisher scale: a Grade 1 in a patient with a ruptured P1 segment PCA aneurysm. b Grade 2 in a patient with a perimesencephalic haemorrhage. c Grade 3 in a patient with a ruptured right MCA aneurysm. d Grade 4 in a patient with ruptured anterior communicating aneurysm, with small amount of intraventricular blood. e Grade 4 in a patient with a ruptured anterior communicating artery aneurysm showing frontal hematoma and blood casts in both atria (*). f Grade 4 with IVH and ICH in a patient with a ruptured terminal segment right ICA aneurysm, showing a large intraparenchymal hematoma.
The density of subarachnoid haemorrhage on initial imaging, as measured by the Hounsfield unit (HU) value of the haemorrhage, has been postulated to predict symptomatic vasospasm [27]. A recent study found that the HU value of blood in the inter-peduncular cistern in aneurysmal SAH patients significantly correlated with the incidence of symptomatic vasospasm [28]. New developments in quantification of cisternal blood include automatic volume quantification of total blood volume (TBV), calculated from admission CT. TBV automatic quantification has the advantage of being rater-independent and has been shown to predict DCI [16, 19].
Cerebral perfusion studies
Cerebral perfusion is reduced in the acute stage of SAH, especially in patients with poor clinical grade at admission [55,56,57], and a few studies have addressed the ability of admission CT perfusion to predict complications. Studies on the value of early CT perfusion (within 72 h from SAH) to predict vasospasm or DCI have shown inconsistent results, including large variability in perfusion thresholds. Etminan et al. [34] showed that an early mean transit time (MTT) > 4,2 s combined with SAH clot volume > 50 mL increased the risk for cerebral infarctions and poor outcome, but showed no association with vasospasm. Sanelli et al. [35] found threshold values of MTT 5,5 s and CBF 24 mL/100 g/min to predict vasospasm. In a study where CT perfusion was performed at < 48 h after SAH, significantly higher mean MTT values and lower mean cerebral blood flow (CBF) values were found in patients that later developed vasospasm [20]. Some authors found a significant association between lower CBF values and longer MTT with DCI [32, 35,36,37]. Lagares and colleagues [36] found an MTT value > 5,9 s to have a positive predictive value (PPV) of 100% for DCI and to be associated to a 20-fold risk increase of poor outcome. Dong et al. in a large prospective study used whole-brain CT perfusion, and found early reduction of perfusion, in all parameters in patients that later developed DCI, specifically a time-to-maximum (Tmax) cut-off value of 2.24 s for early prediction of DCI at admission [33]. Recently, Malinova and colleagues [32] proposed CBF < 53,93 mL/100 g/min, CBV < 3,14 mL/100 mL, MTT > 4,25 s, time to peak (TTP) > 9,28 s and time to drain (TTD) > 4,93 s as threshold values for prediction of DCI. However, despite all available studies, data on the role of brain perfusion at early stage of SAH are conflicting [58,59,60,61,62], and the evaluation of perfusion is still not validated for the initial assessment of SAH patients, as a tool for prediction of vasospasm or DCI.
Digital subtraction angiography
DSA is routinely performed in acute SAH patients and is the gold standard technique for the detection of intracranial aneurysms. Since most patients perform DSA at admission, it would be tempting to identify predictors of vasospasm and DCI using this technique. A recently developed post-processing software, parametric colour coding, allows the evaluation of haemodynamic flow data from DSA acquisitions. Since then, some studies have analysed whether early haemodynamic changes detected on colour-coded DSA in the setting of aneurysmal SAH may be predictive of vasospasm or DCI. Burkhardt et al. found that patients developing vasospasm, either symptomatic or asymptomatic, had increased arterial flow velocities in the initial DSA [38••]. This increase in flow velocity may be due to vessel diameter reduction, increase in arterial blood pressure or both. Either way, these findings may represent early angiographic predictors of vasospasm and DCI and help identify patients at greater risk for these complications. An advantage of colour-coded DSA is the evaluation of microcirculatory changes, allowed by the higher temporal and spatial resolution of newer angiography suites. Gölitz et al. calculated cerebral circulation time, cortical relative time to peak and microvascular transit time (TT) in aneurysmal SAH patients [39]. The mean microvascular TT was significantly longer in patients that later had DCI, possibly indicating an early onset of microcirculatory injury in these patients. A threshold value of 2.69 s was suggested to predict development of DCI, with a sensitivity of 71%, but a specificity of only 54%. Angiographic vasospasm occurring within 48 h of aneurysmal rupture, known as ultra-early angiographic vasospasm, occurs in 4.6–13% of patients and is associated with increased risk of DCI and worse clinical outcome [40,41,42].
Early brain injury: a new marker?
Increasing attention has been drawn to early brain injury (EBI), defined as parenchymal insult occurring in the first 72 h after SAH [10••, 63, 64], thought to contribute to the later occurrence of DCI. Pathophysiological mechanisms of EBI are complex and still not fully understood. A recently developed score, the “Subarachnoid Haemorrhage Early Brain Edema Score” (SEBES) [31], includes early CT changes such as sulci effacement and disruption of the grey-white matter junction on admission CT, as markers of early brain injury, that predict DCI and unfavourable outcome and associate with the occurrence of vasospasm. In line with its superiority in evaluating brain lesions, MRI is the preferred imaging technique to detect early parenchymal changes. Early acute ischaemic lesions on diffusion-weighted imaging (DWI), changes in white matter integrity measured with diffusion tensor imaging, global cerebral edema or vasogenic edema in normal-appearing white matter [43••, 44, 46, 65, 66] can be associated with the development of DCI in the course of SAH [43••, 45,46,47, 66].
Combined predictors
Imaging parameters can be used as independent predictors of vasospasm and DCI, or they can be combined with clinical parameters to increase specificity and sensitivity. The VASOGRADE scale is a simple 3-category grading scale that can predict the risk of DCI, based on combining the modified Fisher scale and the World Federation of Neurosurgical Societies (WFNS) scale [67]. The HAIR score allows risk stratification for in-hospital mortality and is based on the four variables that name it: Hunt and Hess score, age, IVH and re-bleed [68]. One other recent study proposed an early score for DCI prediction that included 4 variables: WFNS scale, modified Fisher scale, SEBES and intraventricular haemorrhage [69]. Although VASOGRADE scale and HAIR score did not show to be superior to clinical evaluation in prediction of cerebral infarction and unfavourable outcome [70], they are superior to radiological scales alone [71].
In summary, the initial imaging evaluation of SAH patients provides potential predictors of vasospasm and DCI. The amount of subarachnoid blood on non-enhanced CT has the most robust evidence as a predictor of vasospasm and DCI. However, newer approaches, such as automatic measurement of subarachnoid blood volume, and colour-coding post-processing of DSA images might help identify patients that will develop vasospasm and DCI. Early perfusion imaging has shown to predict vasospasm and DCI, but is not reproducible across studies. MRI is still not routinely performed upon admission in SAH patients; however, it is the most sensitive imaging technique for diagnosis of early brain injury and could be an early tool for predicting DCI. Combined use of clinical and imaging parameters might increase sensitivity and specificity in the prediction of these complications.
Diagnosis and monitoring of vasospasm
Delayed vasospasm is a well-established complication of aneurysmal SAH occurring in about 70% of patients, most often 6 to 8 days after aneurysm rupture [8, 9]. About a third of patients will develop symptoms from vasospasm and eventually ischaemic lesions. Screening of vasospasm is a standard current practice in SAH, essential for correct management, especially in patients in poor neurological grade that cannot be evaluated clinically. Vasospasm is potentially reversible, both pharmacologically and by endovascular techniques. Several techniques for diagnosis and monitoring of vasospasm have been studied, and their main advantages and disadvantages are summarized in Table 3.
Digital subtraction angiography
At the present time, DSA still remains the gold standard for diagnosis of radiographic vasospasm, additionally allowing for endovascular treatment. Nonetheless, as an invasive technique which brings additional risks, requiring radiation exposure and contrast, DSA is not used as a monitoring technique but is rather performed following clinical or TCD suspicion of vasospasm [72]. Newer developments, such as colour-coded DSA, described in the previous section, allow the evaluation of microcirculatory changes secondary to vasospasm (Fig. 2).
Thirty-six-year-old patient with a ruptured anterior communicating artery aneurysm. Admission DSA showed normal diameter of the arteries (a, right internal carotid artery injection, AP view). Colour-coded DSA images (b) show no delay in transit time between ICA and A1 at post-embolization period, as demonstrated by the time-contrast concentration curves with similar times measured in the internal carotid artery (white arrow) and in the A2 segment of the anterior cerebral artery (open arrow). At 15 days, moderate vasospasm of the A1 and A2 segments of the anterior cerebral artery are noted on DSA (c), with corresponding delay of contrast arrival at the A2 segment on the colour coded DSA images (open arrow) (d). A CTA performed on the same day (e, coronal; f, axial MIP reconstructions) showed similar vasospasm in the A1 segments bilaterally. Note how the presence of metallic artefacts originated from the aneurysmal coils impairs correct assessment of adjacent arteries (f)
Transcranial Doppler
Transcranial Doppler (TCD) allows dynamic monitoring of CBF velocity and pulsatility indexes (Fig. 3). Current American Heart Association’s guidelines for the management aneurysmal SAH indicate TCD as a reasonable tool for vasospasm monitoring (class IIa, level B evidence) [3••]. In addition to mean flow velocity (mFV), the use of indices, such as Lindegaard ratio for MCA vasospasm and the Sviri ratio for basilar artery vasospasm, helps to distinguish increased velocities due to haemodynamic factors from vasospasm (velocity adjustment by calculating a ratio with the ipsilateral ICA and both the vertebral arteries, respectively) [74, 76]. A new intracranial arteriovenous index (AVI) between flow velocity in the MCA and the basal vein of Rosenthal has been proposed, with slightly higher reliability for differentiating vasospasm and hyperperfusion [75].
Thirty-nine-year-old male with a ruptured basilar tip aneurysm that later developed vasospasm and cerebral infarct. CT scan at admission showed a diffuse modified Fisher grade 3 SAH (a), and DSA performed at admission (b) showed normal diameter vessels and a basilar tip aneurysm. CT scan repeated at day 7 post-SAH (c) shows an acute ischaemic infarct on the right PCA vascular territory. Same day TCD study shows increased mFV of the right PCA P1 segment (d), 85 cm/s, left PCA P1 segment (e), 119 cm/s, left ACA A1 segment (f), 103 cm/s, and basilar artery (g), 127 cm/s, suggestive of moderate vasospasm of the PCA P1 segments and left ACA A1 segments, and moderate to severe vasospasm of the basilar artery
Over the years, several mFV threshold values for development of vasospasm have been proposed, either regarding a relative increase of mFV (increase of 20–50 cm/s) or absolute mFV values (> 120–200 cm/s) [99•, 100]. In 2001, a meta-analysis showed that TCD had higher specificity (99%) and sensitivity (67%) for MCA vasospasm, as compared to other arteries, with a positive predictive value (PPV) of 97% and a negative predictive value (NPV) of 78%, when compared to DSA [73]. In 2004, a consensus statement supported that, for MCA vasospasm, TCD is a reliable predictor for the absence of angiographic vasospasm at mFV < 120 cm/s and for the presence of angiographic vasospasm at mFV > 200 cm/s [101].
There have been recent advances in TCD: image-guided TCD and TCD automated analysis. Neulen et al. demonstrated the feasibility of image-guided TCD, in which the ideal ultrasonic bone window regions and ultrasonic trajectories were obtained from CTA images and uploaded on a hand-held image-guided device [77] Although time-consuming, image-guided TCD was feasible in aneurysmal SAH patients, with high spatial accuracy and inter-observer reproducibility. In order to facilitate continuous TCD-monitoring protocols, an automated algorithm for detection of vasospasm based on TCD audio signal analysis was developed, with promising results [78].
Non-invasive angiographic studies
CTA is a fast and widely available non-invasive angiographic imaging modality. It is considered fairly accurate for detection of radiographic proximal vasospasm, with a reported sensitivity of 80% and specificity of 93% [79]. Despite this, there is concern regarding its value to help guide clinical management, as it has only moderate inter-rater reproducibility [102]. Recent areas of research include volumetric analysis of the intracranial vessels, in which vessel volume of a given arterial segment could be used as an objective parameter for identification of vasospasm requiring endovascular treatment, as addressed in two pilot studies [80, 81].
Although MR is not a routine imaging study in acute SAH, the various modalities of magnetic resonance angiography (MRA) can diagnose proximal vasospasm, although less accurately than DSA [82,83,84]. Recently developed black-blood MR angiography (BBMRA) utilizes a non-T1-weighted contrast spin-echo sequence. A small retrospective study by Takano et al. showed superior accuracy of BBMRA when compared to TOF-MRA and high sensitivity and specificity in detection of vasospasm when compared to CTA or DSA [85]. Also recently described is the association between intracranial MR vessel wall enhancement and the development of angiographic vasospasm in ruptured aneurysm patients [86]. Although larger studies are necessary, newer vessel wall imaging sequences may be promising in the evaluation of vasospasm.
Perfusion studies
CT perfusion studies can assess perfusion deficits secondary to vasospasm, manifested by increased MTT and reduced CBF [55, 87,88,89,90,91,92,93]. A high degree of agreement between CT perfusion and DSA has been documented [94], and a meta-analysis showed a sensitivity of 74,1% and specificity of 93% of CT perfusion for the diagnosis of vasospasm [79]. Various studies found MTT to be the most sensitive parameter [88,89,90,91, 93]. MTT threshold values of 4,6–6,4 s [88, 93] and a CBF value of 44,3 mL/100 g/min [93] have been described. However, because of equipment and post-processing software differences between centres, validation of these values is challenging and should be interpreted with caution. Some authors have suggested a combined CTA and CT perfusion approach as the preferred method in the diagnosis of vasospasm [103, 104]. MR perfusion studies in SAH have mainly addressed prediction or early detection of DCI, with very few having focused on prediction or diagnosis of vasospasm. Combination of DWI and perfusion-weighted imaging (PWI) in patients with vasospasm enabled the detection of small regions of early ischaemic injury within larger regions of abnormal relative CBF and MTT, compatible with vascular supply regions of vessels with angiographically demonstrated vasospasm [97] (Fig. 4). Diffusion-perfusion mismatch, translated by elevated MTT and no signs of parenchymal ischaemia on DWI, has also been suggested for early identification of vasospasm and prediction of its evolution to ischaemia [96, 98].
Forty-one-year-old patient with a ruptured basilar tip aneurysm. a DSA at admission, after coiling of the aneurysm. Normal diameter of basilar artery and posterior cerebral arteries (PCA) (white arrows). b DSA at day 7 post-SAH, showing reduction of the diameter of the basilar artery and both PCAs (black arrows). MRI performed at day 4 post-SAH showed small acute ischaemic lesions on both PCA territories, on DWI (c), and an increase of TTP on the same territory (d), reflecting hypoperfusion, with a DWI/PWI mismatch. e CT scan at day 10 after SAH, showing an acute ischaemic lesion on the right PCA territory, and global cerebral edema, that progressed despite aggressive treatment of vasospasm.
In summary, TCD is still the preferred technique for screening the appearance of vasospasm. Although operator-dependent, it is a non-invasive, widely available bedside technique that can effectively detect and monitor cerebral artery vasospasm, with a high positive predictive value. Image-guided TCD and TCD automated analysis are being developed and seem promising for improving monitoring accuracy and facilitate its implementation on critical care units.
Prediction and diagnosis of DCI
Delayed cerebral ischaemia is the end result of a complex cascade of events after SAH that include early brain injury (that results from microvascular changes, coagulation dysfunction, cortical spreading depression, activation of inflammatory mediators) and delayed vasospasm [10••]. Although DCI negatively influences patient prognosis, the best method to predict this complication remains uncertain.
Computed tomography and MR imaging
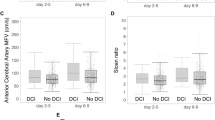
In patients that suffer neurological deterioration after SAH, non-contrast CT is a rapid and widely available technique, allowing the exclusion of hydrocephalus, rebleeding or cerebral edema that may occur in the subacute stages of SAH. CT can diagnose cerebral infarctions related to DCI in up to 35% of patients in the course of SAH (Fig. 3); however, if MR imaging is used, ischaemia can be detected in up to 81% of patients [105](Fig. 5). Besides clinical and imaging predictors present at admission, there are other possible imaging predictors of DCI during the early phase of SAH and in the period of vasospasm (Table 4).
Fifty-nine-year-old patient with a ruptured communicating artery aneurysm treated with coils. Follow-up CT scan at day 9 after SAH (a) shows a very subtle hypoattenuating lesion in the left insular and temporal lobes. Same day MRI, DWI (b) and ADC map (c), clearly depict the acute cerebral infarct, illustrating the lower sensitivity of CT in diagnosis of acute cerebral ischaemia. CT perfusion performed 2 days earlier showed a very slight decrease in CBF (d) in the infarct area and no asymmetry on the MTT map (e). DSA performed at day 10 (f) shows no signs of angiographic vasospasm.
Transcranial Doppler
TCD is the most used monitoring tool for vasospasm after SAH; however, evidence of the value of TCD in predicting DCI is still conflicting. Meta-analysis found that the diagnosis of moderate/severe vasospasm by TCD (defined by mFV > 120 cm/s) can accurately predict DCI, with high sensitivity and high negative predictive value [106]. However, centres that routinely screened for vasospasm using TCD did not have higher rates of DCI diagnosis compared to non-screening centres [120].
Perfusion studies
Although CT perfusion can detect areas of cerebral hypoperfusion that correlate with arterial vasospasm, there are conflicting results regarding its association with DCI, which again underlines the multifactorial origin of DCI. Several CT perfusion studies have shown significantly lower CBF and CBV values and higher MTT values in patients with DCI, during the vasospasm window period [88, 114, 115]. Two meta-analyses, one including 345 patients [116] and the other including 444 patients [62], confirmed these findings. In the first one, a 23-fold increased probability of DCI was found in patients with CT perfusion changes demonstrating perfusion deficits [116]. Different threshold values have been proposed for diagnosis of DCI at the time window for vasospasm, including MTT values of 5,0–5,85 s [88, 114, 115] and CBF values of 30,5–36,3 mL/100 mg/min [114, 115]. The ability of CT perfusion changes to predict DCI appears to be higher during the period of vasospasm, between 4 and 10 days after SAH. MR perfusion imaging is much less used in SAH patients, and therefore, less studies have focused on this technique. Positron emission tomography (PET) studies have also shown that hypoperfused and oligemic areas of the brain frequently occur in regions without vasospasm, and these physiologic parameters might better predict DCI [121].
Future research: autoregulation and permeability
Failure of autoregulatory mechanisms is one possible mechanism in the development of vasospasm and DCI. A few studies have suggested the utility of a transient hyperemic response test (THRT) in the early phase to predict cerebral autoregulation failure and development of clinical vasospasm [107, 108, 110]. This test is based on temporary compression of the common carotid artery while insonating the ipsilateral MCA. Upon decompression, an increase of more than 9% of the baseline systolic velocity is expected, when autoregulation is normal. A negative THRT was associated to development of symptomatic vasospasm and DCI [109]. A reduced cerebrovascular reactivity (CVR) assessed by carbon dioxide or acetazolamide TCD was also associated with DCI [111,112,113]. In a small pilot study, blood oxygenation level-dependent (BOLD) technique functional MRI measurements of CVR, by means of carbon dioxide challenge, seemed to have good spatial correlation with areas of future ischaemic events, in the context of DCI [117]. Assessment of cerebral autoregulation or CVR is still not used in clinical practice.
Finally, blood-brain barrier (BBB) dysfunction has been implicated as one of the many contributors to DCI. Its assessment by means of permeability imaging (through CT or MR perfusion techniques) might add as a tool for predicting DCI. Two recent studies have found an association between increased BBB permeability and DCI [118, 119]; however, permeability imaging is still not used in the clinical setting.
In summary, although DCI is one of the most important complications of SAH, it is very difficult to predict. TCD, although useful in the diagnosis of vasospasm, has questionable value in predicting DCI. CT perfusion performed during the period of vasospasm might help identify patients that will have DCI. Diagnosis of DCI relies on non-contrast imaging, and MRI is the best technique, with higher sensitivity than the most commonly performed CT studies. Research is ongoing on other techniques, such as the evaluation of autoregulatory mechanisms and BBB dysfunction, and might add as future tools for prediction of this important complication of SAH.
Conclusion
Imaging studies have been traditionally used to diagnose acute spontaneous SAH and to investigate the presence of a ruptured aneurysm. However, imaging studies performed early in the course of SAH also provide clues for prediction of its major complications: vasospasm and DCI. The volume of subarachnoid blood is a strong predictor of both these complications, but recent technical improvements such as automatized quantification of blood on CT, and colour-coding post-processing of DSA images, have added value in identifying patients that will develop vasospasm and DCI. MRI, still not routinely performed in SAH patients, has the potential to diagnose early brain injury and help predict DCI.
Monitoring of vasospasm is still important in SAH patients, and TCD is still the preferred technique for this purpose in most centres. Patients with suspected symptomatic vasospasm on TCD will undergo DSA, the gold standard technique to confirm vasospasm, offering the possibility of endovascular treatment.
The occurrence of DCI has significant impact on the outcome of patients with SAH; however, and despite extensive research, it is very difficult to predict. Of all imaging methods, CT perfusion performed during the period of vasospasm, at 7–10 days, might help identify patients that will have DCI. However, CT perfusion thresholds are still not validated across centres. Other techniques, such as the evaluation of autoregulatory mechanisms and BBB dysfunction, are under research and might be future tools to help predict of this important complication of SAH. Combining clinical and imaging parameters might increase sensitivity and specificity in the prediction of vasospasm and DCI after SAH.
Change history
05 January 2021
A correction to this paper has been published: https://doi.org/10.1007/s11940-020-00658-w
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Barry C, Turner RJ, Corrigan F, Vink R. New therapeutic approaches to subarachnoid hemorrhage. Expert Opin Investig Drugs. 2012;21:845–59.
Linn FHH, Rinkel GJE, Algra A, van Gijn J. Incidence of subarachnoid hemorrhage. Stroke. 1996;27:625–9.
•• Connolly ES, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2012;43:1711–37 Essential reading for those who manage SAH, these are the most recent guidelines.
Hop JW, Rinkel GJE, Algra A, et al. Case-fatality rates and functional outcome after subarachnoid hemorrhage: a systematic review. Stroke. 1997;28:660–4.
Rinkel GJE, Algra A. Long-term outcomes of patients with aneurysmal subarachnoid haemorrhage. Lancet Neurol. 2011;10:349–56.
Vergouwen MDI, Vermeulen M, Muizelaar JP, et al. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies proposal of a multidisciplinary research group. Stroke. 2010;41:2391–5.
Frontera JA, Fernandez A, Schmidt JM, Claassen J, Wartenberg KE, Badjatia N, et al. Defining vasospasm after subarachnoid hemorrhage: what is the most clinically relevant definition? Stroke. 2009;40:1963–8.
Crowley RW, Medel R, Dumont AS, Ilodigwe D, Kassell NF, Mayer SA, et al. Angiographic vasospasm is strongly correlated with cerebral infarction after subarachnoid hemorrhage. Stroke. 2011;42:919–23.
Kassell N, Sasaki T, Colohan A, et al. Cerebral vasospasm following aneurysmal subarachnoid hemorrhage. Stroke. 1985;16:562–73.
•• Geraghty JR, Testai FD. Delayed cerebral ischemia after subarachnoid hemorrhage: beyond vasospasm and towards a multifactorial pathophysiology. Curr Atheroscler Rep. 2017;19(12):50. https://doi.org/10.1007/s11883-017-0690-x. Important to understand the complex pathophysiology of SAH and its complications.
Rabinstein AA, Friedman JA, Weigand SD, McClelland RL, Fulgham JR, Manno EM, et al. Predictors of cerebral infarction in aneurysmal subarachnoid hemorrhage. Stroke. 2004;35:1862–6.
Dubosh NM, Bellolio MF, Rabinstein AA, Edlow JA. Sensitivity of early brain computed tomography to exclude aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. Stroke. 2016;47:750–5.
McCormack RF, Hutson A. Can computed tomography angiography of the brain replace lumbar puncture in the evaluation of acute-onset headache after a negative noncontrast cranial computed tomography scan? Acad Emerg Med. 2010;17:444–51.
Frontera JA, Claassen J, Schmidt JM, Wartenberg KE, Temes R, Connolly ES, et al. Prediction of symptomatic vasospasm after subarachnoid hemorrhage: the modified fisher scale. Neurosurgery. 2006;59:21–7.
Hijdra A, Van Gijn J, Nagelkerke N, et al. Prediction of delayed cerebral ischemia, rebleeding, and outcome after aneurysmal subarachnoid hemorrhage. Stroke. 1988;19:1250–6.
van der Steen WE, Marquering HA, Boers AMM, Ramos LA, van den Berg R, Vergouwen MDI, et al. Predicting delayed cerebral ischemia with quantified aneurysmal subarachnoid blood volume. World Neurosurg. 2019;130:e613–9.
Neidert MC, Maldaner N, Stienen MN, Roethlisberger M, Zumofen DW, D’Alonzo D, et al. The barrow neurological institute grading scale as a predictor for delayed cerebral ischemia and outcome after aneurysmal subarachnoid hemorrhage: data from a nationwide patient registry (Swiss SOS). Clin Neurosurg. 2018;83:1286–93.
Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery. 1980;6:1–9.
Zijlstra IA, Gathier CS, Boers AM, Marquering HA, Slooter AJ, Velthuis BK, et al. Association of automatically quantified total blood volume after aneurysmal subarachnoid hemorrhage with delayed cerebral ischemia. Am J Neuroradiol. 2016;37:1588–93.
Starnoni D, Maduri R, Hajdu SD, Pierzchala K, Giammattei L, Rocca A, et al. Early perfusion computed tomography scan for prediction of vasospasm and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2019;130:e743–52.
Dengler NF, Diesing D, Sarrafzadeh A, Wolf S, Vajkoczy P. The Barrow Neurological Institute scale revisited: predictive capabilities for cerebral infarction and clinical outcome in patients with aneurysmal subarachnoid hemorrhage. Neurosurgery. 2017;81:341–9.
Inagawa T. Risk factors for cerebral vasospasm following aneurysmal subarachnoid hemorrhage: a review of the literature. World Neurosurg. 2016;85:56–76.
• van der Steen WE, Leemans EL, van den Berg R, et al. Radiological scales predicting delayed cerebral ischemia in subarachnoid hemorrhage: systematic review and meta-analysis. Neuroradiology. 2019;61:247–56 Good review of available imaging scales for prediction of DCI.
Rosen DS, Macdonald RL, Huo D, Goldenberg FD, Novakovic RL, Frank JI, et al. Intraventricular hemorrhage from ruptured aneurysm: clinical characteristics, complications, and outcomes in a large, prospective, multicenter study population. J Neurosurg. 2007;107:261–5.
Eagles ME, Jaja BNR, Macdonald RL. Incorporating a modified graeb score to the modified fisher scale for improved risk prediction of delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. Clin Neurosurg. 2018;82:299–305.
Platz J, Güresir E, Wagner M, Seifert V, Konczalla J. Increased risk of delayed cerebral ischemia in subarachnoid hemorrhage patients with additional intracerebral hematoma. J Neurosurg. 2017;126:504–10.
Reilly C, Amidei C, Tolentino J, Jahromi BS, Macdonald RL. Clot volume and clearance rate as independent predictors of vasospasm after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2004;101:255–61.
Ishihara H, Oka F, Kawano R, Shinoyama M, Nishimoto T, Kudomi S, et al. Hounsfield unit value of interpeduncular cistern hematomas can predict symptomatic vasospasm. Stroke. 2020;51:143–8.
Scherer M, Jung JO, Cordes J, et al. Association of cerebrospinal fluid volume with cerebral vasospasm after aneurysmal subarachnoid hemorrhage: a retrospective volumetric analysis. Neurocrit Care. 2020;33(1):152–64. https://doi.org/10.1007/s12028-019-00878-2.
Black MCLP. Hydrocephalus and vasospasm after subarachnoid hemorrhage from ruptured intracranial aneurysms. Neurosurgery. 1986;18:12–6.
Ahn SH, Savarraj JP, Pervez M, et al. The subarachnoid hemorrhage early brain edema score predicts delayed cerebral ischemia and clinical outcomes. Clin Neurosurg. 2018;83:137–45.
Malinova V, Tsogkas I, Behme D, Rohde V, Psychogios MN, Mielke D. Defining cutoff values for early prediction of delayed cerebral ischemia after subarachnoid hemorrhage by CT perfusion. Neurosurg Rev. 2020;43:581–7.
Dong L, Zhou Y, Wang M, Yang C, Yuan Q, Fang X. Whole-brain CT perfusion on admission predicts delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. Eur J Radiol. 2019;116:165–73.
Etminan N, Beseoglu K, Heiroth HJ, Turowski B, Steiger HJ, Hänggi D. Early perfusion computerized tomography imaging as a radiographic surrogate for delayed cerebral ischemia and functional outcome after subarachnoid hemorrhage. Stroke. 2013;44:1260–6.
Sanelli PC, Jou A, Gold R, Reichman M, Greenberg E, John M, et al. Using CT perfusion during the early baseline period in aneurysmal subarachnoid hemorrhage to assess for development of vasospasm. Neuroradiology. 2011;53:425–34.
Lagares A, Cicuendez M, Ramos A, et al. Acute perfusion changes after spontaneous SAH: a perfusion CT study. Acta Neurochir. 2012;154:402–5.
Duan Y, Xu H, Li R, Zheng K, Hu Z, Wu N, et al. Computed tomography perfusion deficits during the baseline period in aneurysmal subarachnoid hemorrhage are predictive of delayed cerebral ischemia. J Stroke Cerebrovasc Dis. 2017;26:162–8.
•• Burkhardt JK, Chen X, Winkler EA, et al. Early hemodynamic changes based on initial color-coding angiography as a predictor for developing subsequent symptomatic vasospasm after aneurysmal subarachnoid hemorrhage. file///Users/isabelfragata/Downloads/burkhardt2017.pdfWorld. Neurosurg. 2018;109:e363–73 Interesting paper on newer developments in color-coded DSA.
Gölitz P, Hoelter P, Rösch J, Roessler K, Knossalla F, Doerfler A. Ultra-early detection of microcirculatory injury as predictor of developing delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Clin Neuroradiol. 2018;28:501–7.
Qureshi AI, Sung GY, Suri MAK, Straw RN, Guterman LR, Hopkins LN. Prognostic value and determinants of ultraearly angiographic vasospasm after aneurysmal subarachnoid hemorrhage [1] (multiple letters). Neurosurgery. 1999;44:967–74.
Baldwin ME, Macdonald RL, Huo D, et al. Early vasospasm on admission angiography in patients with aneurysmal subarachnoid hemorrhage is a predictor for in-hospital complications and poor outcome. Stroke. 2004;35:2506 LP – 2511.
Al-Mufti F, Roh D, Lahiri S, et al. Ultra-early angiographic vasospasm associated with delayed cerebral ischemia and infarction following aneurysmal subarachnoid hemorrhage. J Neurosurg. 2017;126:1545–51.
•• Frontera JA, Ahmed W, Zach V, et al. Acute ischaemia after subarachnoid haemorrhage, relationship with early brain injury and impact on outcome: a prospective quantitative MRI study. J Neurol Neurosurg Psychiatry. 2015;86:71–8 Important paper on imaging of early brain injury, and its relevance to outcome.
Liu Y, Soppi V, Mustonen T, Könönen M, Koivisto T, Koskela A, et al. Subarachnoid hemorrhage in the subacute stage: elevated apparent diffusion coefficient in normal-appearing brain tissue after treatment. Radiology. 2007;242:518–25.
Fragata I, Alves M, Papoila AL, Nunes AP, Ferreira P, Canto-Moreira N, et al. Early prediction of delayed ischemia and functional outcome in acute subarachnoid hemorrhage: role of diffusion tensor imaging. Stroke. 2017;48:2091–7.
De Marchis GM, Filippi CG, Guo X, et al. Brain injury visible on early MRI after subarachnoid hemorrhage might predict neurological impairment and functional outcome. Neurocrit Care. 2015;22:74–81.
Weimer JM, Jones SE, Frontera JA. Acute cytotoxic and vasogenic edema after subarachnoid hemorrhage: a quantitative MRI study. Am J Neuroradiol. 2017;38:928–34.
Hijdra A, Brouwers PJ, Vermeulen M, van Gijn J. Grading the amount of blood on computed tomograms after subarachnoid hemorrhage. Stroke. 1990;21:1156–61.
Woo PYM, Tse TPK, Chan RSK, Leung LNY, Liu SKK, Leung AYT, et al. Computed tomography interobserver agreement in the assessment of aneurysmal subarachnoid hemorrhage and predictors for clinical outcome. J Neurointerv Surg. 2017;9:1118–24.
Zanaty M, Nakagawa D, Starke RM, Leira EC, Samaniego EA, Guerrero WR, et al. Intraventricular extension of an aneurysmal subarachnoid hemorrhage is an independent predictor of a worse functional outcome. Clin Neurol Neurosurg. 2018;170:67–72.
Graeb DA, Robertson WD, Lapointe JS, Nugent RA, Harrison PB. Computed tomographic diagnosis of intraventricular hemorrhage. Etiology and prognosis. Radiology. 1982;143:91–6.
Morgan TC, Dawson J, Spengler D, Lees KR, Aldrich C, Mishra NK, et al. The modified graeb score: an enhanced tool for intraventricular hemorrhage measurement and prediction of functional outcome. Stroke. 2013;44:635–41.
Schuss P, Hadjiathanasiou A, Borger V, Wispel C, Vatter H, Güresir E. Poor-grade aneurysmal subarachnoid hemorrhage: factors influencing functional outcome—a single-center series. World Neurosurg. 2016;85:125–9.
•• Macdonald RL, Schweizer TA. Spontaneous subarachnoid haemorrhage. Lancet. 2016;389(10069):655–66. https://doi.org/10.1016/S0140-6736(16)30668-7. Very well written paper on spontaneous SAH, for a global clinical and imaging perspective.
Nabavi DG, LeBlanc LM, Baxter B, et al. Monitoring cerebral perfusion after subarachnoid hemorrhage using CT. Neuroradiology. 2001;43:7–16.
Tateyama K, Kobayashi S, Murai Y, Teramoto A. Assessment of cerebral circulation in the acute phase of subarachnoid hemorrhage using perfusion computed tomography. J Nippon Med Sch. 2013;80:110–8.
Fragata I, Alves M, Papoila AL, Diogo M, Canhão P, Canto-Moreira N. Temporal evolution of cerebral computed tomography perfusion after acute subarachnoid hemorrhage: a prospective cohort study. Acta Radiol. 2020;61:376–85.
Van Der Schaaf I, Wermer MJ, Van Der Graaf Y, et al. CT after subarachnoid hemorrhage: relation of cerebral perfusion to delayed cerebral ischemia. Neurology. 2006;66:1533–8.
Rodriguez-Régent C, Hafsa M, Turc G, Ben Hassen W, Edjlali M, Sermet A, et al. Early quantitative CT perfusion parameters variation for prediction of delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. Eur Radiol. 2016;26:2956–63.
Takahashi Y, Sasahara A, Yamazaki K, Inazuka M, Kasuya H. Disturbance of CT perfusion within 24 h after onset is associated with WFNS grade but not development of DCI in patients with aneurysmal SAH. Acta Neurochir. 2017;159:2319–24.
Fragata I, Alves M, Papoila AL, Nunes AP, Ferreira P, Diogo M, et al. Computed tomography perfusion as a predictor of delayed cerebral ischemia and functional outcome in spontaneous subarachnoid hemorrhage: a single center experience. Neuroradiol J. 2019;32:179–88.
Cremers CHP, van der Schaaf IC, Wensink E, Greving JP, Rinkel GJE, Velthuis BK, et al. CT perfusion and delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J Cereb Blood Flow Metab. 2014;34:200–7.
Kusaka G, Ishikawa M, Nanda A, Granger DN, Zhang JH. Signaling pathways for early brain injury after subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2004;24:916–25.
Sehba FA, Pluta RM, Zhang JH. Metamorphosis of subarachnoid hemorrhage research: from delayed vasospasm to early brain injury. Mol Neurobiol. 2011;43:27–40.
Sato K, Shimizu H, Fujimura M, Inoue T, Matsumoto Y, Tominaga T. Acute-stage diffusion-weighted magnetic resonance imaging for predicting outcome of poor-grade aneurysmal subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2010;30:1110–20.
Wartenberg KE, Sheth SJ, Michael Schmidt J, Frontera JA, Rincon F, Ostapkovich N, et al. Acute ischemic injury on diffusion-weighted magnetic resonance imaging after poor grade subarachnoid hemorrhage. Neurocrit Care. 2011;14:407–15.
De Oliveira Manoel AL, Jaja BN, Germans MR, et al. The VASOGRADE: a simple grading scale for prediction of delayed cerebral ischemia after subarachnoid hemorrhage. Stroke. 2015;46:1826–31.
Lee VH, Ouyang B, John S, Conners JJ, Garg R, Bleck TP, et al. Risk stratification for the in-hospital mortality in subarachnoid hemorrhage: the HAIR score. Neurocrit Care. 2014;21:14–9.
Fang YJ, Mei SH, Lu JN, Chen YK, Chai ZH, Dong X, et al. New risk score of the early period after spontaneous subarachnoid hemorrhage: for the prediction of delayed cerebral ischemia. CNS Neurosci Ther. 2019;25:1173–81.
Dengler NF, Sommerfeld J, Diesing D, Vajkoczy P, Wolf S. Prediction of cerebral infarction and patient outcome in aneurysmal subarachnoid hemorrhage: comparison of new and established radiographic, clinical and combined scores. Eur J Neurol. 2018;25:111–9.
Fang Y, Lu J, Zheng J, et al. Comparison of aneurysmal subarachnoid hemorrhage grading scores in patients with aneurysm clipping and coiling. Sci Rep. 2020;10:1–9.
Arias EJ, Vajapey S, Reynolds MR, Chicoine MR, Rich KM, Dacey RG Jr, et al. Utility of screening for cerebral vasospasm using digital subtraction angiography. Stroke. 2015;46:3137–41.
Lysakowski C, Walder B, Costanza MC, Tramèr MR. Transcranial Doppler versus angiography in patients with vasospasm due to a ruptured cerebral aneurysm: a systematic review. Stroke. 2001;32:2292–8.
Lindegaard KF, Nornes H, Bakke SJ, et al. Cerebral vasospasm diagnosis by means of angiography and blood velocity measurements. Acta Neurochir. 1989;100:12–24.
Connolly F, Schreiber SJ, Leithner C, Bohner G, Vajkoczy P, Valdueza JM. Assessment of intracranial venous blood flow after subarachnoid hemorrhage: a new approach to diagnose vasospasm with transcranial color-coded duplex sonography. J Neurosurg. 2018;129:1136–42.
Sviri GE, Ghodke B, Britz GW, Douville CM, Haynor DR, Mesiwala AH, et al. Transcranial doppler grading criteria for basilar artery vasospasm. Neurosurgery. 2006;59:360–5.
Neulen A, Stein M, Pantel T, Berres M, Brockmann C, Giese A, et al. Image-guided transcranial Doppler ultrasound for monitoring posthemorrhagic vasospasms of Infratentorial arteries: a feasibility study. World Neurosurg. 2020;134:284–91.
Elzaafarany K, Aly MH, Kumar G, Nakhmani A. Cerebral artery vasospasm detection using transcranial Doppler signal analysis. J Ultrasound Med. 2019;38:2191–202.
Greenberg ED, Gold R, Reichman M, John M, Ivanidze J, Edwards AM, et al. Diagnostic accuracy of CT angiography and CT perfusion for cerebral vasospasm: a meta-analysis. Am J Neuroradiol. 2010;31:1853–60.
Neulen A, Pantel T, Dieter A, Kosterhon M, Berres M, Thal SC, et al. Volumetric analysis of intracranial vessels: a novel tool for evaluation of cerebral vasospasm. Int J Comput Assist Radiol Surg. 2019;14:157–67.
Neulen A, Kunzelmann S, Kosterhon M, et al. Automated grading of cerebral vasospasm to standardize computed tomography angiography examinations after subarachnoid hemorrhage. Front Neurol. 2020;11:1–10.
Grandin CB, Cosnard G, Hammer F, Duprez TP, Stroobandt G, Mathurin P. Vasospasm after subarachnoid hemorrhage: diagnosis with MR angiography. Am J Neuroradiol. 2000;21:1611–7.
Hamaguchi A, Fujima N, Yoshida D, Hamaguchi N, Kodera S. Improvement of the diagnostic accuracy of MRA with subtraction technique in cerebral vasospasm. J Neuroimaging. 2014;24:548–53.
Hattingen E, Blasel S, Dumesnil R, et al. MR angiography in patients with subarachnoid hemorrhage: adequate to evaluate vasospasm-induced vascular narrowing? Neurosurg Rev. 2010;33:431–9.
Takano K, Hida K, Iwaasa M, Inoue T, Yoshimitsu K. Three-dimensional spin-echo-based black-blood MRA in the detection of vasospasm following subarachnoid hemorrhage. J Magn Reson Imaging. 2019;49:800–7.
Mossa-Basha M, Huynh TJ, Hippe DS, et al. Vessel wall MRI characteristics of endovascularly treated aneurysms: association with angiographic vasospasm. J Neurosurg. 2019;131:859–67.
Dankbaar JW, Rijsdijk M, van der Schaaf IC, Velthuis BK, Wermer MJH, Rinkel GJE. Relationship between vasospasm, cerebral perfusion, and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Neuroradiology. 2009;51:813–9.
Kanazawa R, Kato M, Ishikawa K, Eguchi T, Teramoto A. Convenience of the computed tomography perfusion method for cerebral vasospasm detection after subarachnoid hemorrhage. Surg Neurol. 2007;67:604–11.
Binaghi S, Colleoni ML, Maeder P, et al. CT angiography and perfusion CT in cerebral vasospasm after subarachnoid hemorrhage. AJNR Am J Neuroradiol. 2007;28:750–8.
Wintermark M, Dillon WP, Smith WS, Lau BC, Chaudhary S, Liu S, et al. Visual grading system for vasospasm based on perfusion CT imaging: comparisons with conventional angiography and quantitative perfusion CT. Cerebrovasc Dis. 2008;26:163–70.
Lefournier V, Krainik A, Gory B, Derderian F, Bessou P, Fauvage B, et al. Quantification du vasospasme cérébral après hémorragie sous-arachnoïdienne par scanner de perfusion. J Neuroradiol. 2010;37:284–91.
Dolatowski K, Malinova V, Frölich AMJ, et al. Volume perfusion CT (VPCT) for the differential diagnosis of patients with suspected cerebral vasospasm: qualitative and quantitative analysis of 3D parameter maps. Eur J Radiol. 2014;83:1881–9.
Wintermark M, Ko NUU, Smith WSS, Liu S, Higashida RT, Dillon WP. Vasospasm after subarachnoid hemorrhage: utility of perfusion CT and CT angiography on diagnosis and management. AJNR Am J Neuroradiol. 2006;27:26–34.
Moftakhar R, Rowley HA, Turk A, et al. Utility of computed tomography perfusion in detection of cerebral vasospasm in patients with subarachnoid hemorrhage. Neurosurg Focus. 2006;21:E6.
Afat S, Brockmann C, Nikoubashman O, Müller M, Thierfelder KM, Brockmann MA, et al. Diagnostic accuracy of simulated low-dose perfusion CT to detect cerebral perfusion impairment after aneurysmal subarachnoid hemorrhage: a retrospective analysis. Radiology. 2018;287:643–50.
Ohtonari T, Kakinuma K, Kito T, et al. Diffusion-perfusion mismatch in symptomatic vasospasm after subarachnoid hemorrhage. Neurol Med Chir (Tokyo). 2008;48:331–6 discussion 336.
Rordorf G, Koroshetz WJ, Copen WA, Gonzalez G, Yamada K, Schaefer PW, et al. Diffusion- and perfusion-weighted imaging in vasospasm after subarachnoid hemorrhage. Stroke. 1999;30:599–605.
Vatter H, Güresir E, Berkefeld J, et al. Perfusion-diffusion mismatch in MRI to indicate endovascular treatment of cerebral vasospasm after subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2011;82:876–83.
• Sharma S, Lubrica RJ, Song M, et al. The role of transcranial doppler in cerebral vasospasm: a literature review. Acta Neurochir Suppl. 2020;127:201–5 Good review on the role of TCD for diagnosis of vasospasm.
Mills JN, Mehta V, Russin J, Amar AP, Rajamohan A, Mack WJ. Advanced imaging modalities in the detection of cerebral vasospasm. Neurol Res Int. 2013;2013:1–15.
Sloan MA, Alexandrov AV, Tegeler CH, et al. Assessment: transcranial doppler ultrasonography. Report of the therapeutics and technology assessment Subcommittee of the American Academy of neurology. Neurology. 2004;62:1468–81.
Letourneau-Guillon L, Farzin B, Darsaut TE, Kotowski M, Guilbert F, Chagnon M, et al. Reliability of CT angiography in cerebral vasospasm: a systematic review of the literature and an inter- and intraobserver study. AJNR Am J Neuroradiol. 2020;41:612–8.
Sanelli PC, Pandya A, Segal AZ, Gupta A, Hurtado-Rua S, Ivanidze J, et al. Cost-effectiveness of CT angiography and perfusion imaging for delayed cerebral ischemia and vasospasm in aneurysmal subarachnoid hemorrhage. AJNR Am J Neuroradiol. 2014;35:1714–20.
Stecco A, Fabbiano F, Amatuzzo P, Quagliozzi M, Soligo E, Divenuto I, et al. Computed tomography perfusion and computed tomography angiography in vasospasm after subarachnoid hemorrhage. J Neurosurg Sci. 2018;62:397–405.
Rabinstein AA, Weigand S, Atkinson JLD, Wijdicks EFM. Patterns of cerebral infarction in aneurysmal subarachnoid hemorrhage. Stroke. 2005;36:992–7.
Kumar G, Shahripour RB, Harrigan MR. Vasospasm on transcranial Doppler is predictive of delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J Neurosurg. 2016;124:1257–64.
Lam JMK, Smielewski P, Czosnyka M, Pickard JD, Kirkpatrick PJ. Predicting delayed ischemic deficits after aneurysmal subarachnoid hemorrhage using a transient hyperemic response test of cerebral autoregulation. Neurosurgery. 2000;47:819–26.
Budohoski KP, Czosnyka M, Smielewski P, Varsos GV, Kasprowicz M, Brady KM, et al. Cerebral autoregulation after subarachnoid hemorrhage: comparison of three methods. J Cereb Blood Flow Metab. 2013;33:449–56.
Rynkowski CB, de Oliveira Manoel AL, dos Reis MM, Puppo C, Worm PV, Zambonin D, et al. Early transcranial Doppler evaluation of cerebral autoregulation independently predicts functional outcome after aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2019;31:253–62.
Al-Jehani H, Angle M, Marcoux J, et al. Early abnormal transient hyperemic response test can predict delayed ischemic neurologic deficit in subarachnoid hemorrhage. Crit Ultrasound J. 2018;10:1–6.
Bøthun ML, Haaland ØA, Moen G, Logallo N, Svendsen F, Thomassen L, et al. Impaired cerebrovascular reactivity may predict delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. J Neurol Sci. 2019;407:116539.
Carrera E, Kurtz P, Badjatia N, Fernandez L, Claassen J, Lee K, et al. Cerebrovascular carbon dioxide reactivity and delayed cerebral ischemia after subarachnoid hemorrhage. Arch Neurol. 2010;67:434–9.
Frontera JA, Rundek T, Schmidt JM, Claassen J, Parra A, Wartenberg KE, et al. Cerebrovascular reactivity and vasospasm after subarachnoid hemorrhage: a pilot study. Neurology. 2006;66:727–9.
Dankbaar JW, de Rooij NK, Rijsdijk M, Velthuis BK, Frijns CJM, Rinkel GJE, et al. Diagnostic threshold values of cerebral perfusion measured with computed tomography for delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Stroke. 2010;41:1927–32.
Sanelli PC, Anumula N, Johnson CE, Comunale JP, Tsiouris AJ, Riina H, et al. Evaluating CT perfusion using outcome measures of delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage. AJNR Am J Neuroradiol. 2013;34:292–8.
Mir DI, Gupta A, Dunning A, et al. CT perfusion for detection of delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2014;35:866–71.
da Costa L, Fisher J, Mikulis DJ, et al. Early identification of brain tissue at risk for delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. In: Fandino J, Marbacher S, Fathi A-R, et al., editors. Neurovascular Events After Subarachnoid Hemorrhage, vol. 120. Acta Neurochirurgica Supplement. Cham: Springer International Publishing; 2015. p. 105–9.
Russin JJ, Montagne A, D’Amore F, He S, Shiroishi MS, Rennert RC, et al. Permeability imaging as a predictor of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2018;38:973–9.
Malinova V, Iliev B, Tsogkas I, et al. Assessment of tissue permeability by early CT perfusion as a surrogate parameter for early brain injury after subarachnoid hemorrhage. J Neurosurg. 2020;23:1–6. https://doi.org/10.3171/2019.5.jns19765.
Hollingworth M, Jamjoom AAB, Bulters D, Patel HC. How is vasospasm screening using transcranial Doppler associated with delayed cerebral ischemia and outcomes in aneurysmal subarachnoid hemorrhage? Acta Neurochir. 2019;161:385–92.
Dhar R, Scalfani MT, Blackburn S, Zazulia AR, Videen T, Diringer M. Relationship between angiographic vasospasm and regional hypoperfusion in aneurysmal subarachnoid hemorrhage. Stroke. 2012;43:1788–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to the incorrect formating of the name of the last author. It should read from 'PatrU´cia CanhÐo’ to ‘Patrícia Canhão’.
This article is part of the Topical Collection on Critical Care Neurology
Rights and permissions
About this article
Cite this article
Fragata, I., Cunha, B. & Canhão, P. Imaging Predictors of Vasospasm and Delayed Cerebral Ischaemia After Subarachnoid Haemorrhage. Curr Treat Options Neurol 22, 47 (2020). https://doi.org/10.1007/s11940-020-00653-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s11940-020-00653-1