Abstract
The purpose of the present study was to assess the size and configuration of the perirectal fatty tissues using magnetic resonance imaging, including the volume occupied by the rectum itself, and to establish a simple method by which such analysis could be derived. Included in the study were 25 consecutive patients without any large pelvic tumor (diameter of potential pelvic tumor less than 3 cm in any plane) referred for high-resolution pelvic MR imaging. The volume and cross-sectional parameters based on the amount of mesorectum to different sides of the rectum, and the total area occupied, including the rectum, were retrospectively measured using a transaxial three-dimensional T1-weighted gradient–echo sequence. The mesorectum, including the rectum within, occupied an axial area ranging from 320 to 5992 mm2, and a total volume of 54–323 ml. There was a good correlation between anteroposterior diameter of the perirectal fat at 4 cm below S1-2 and the left-to-right diameter 7 cm below S1-2, and the total volume. Furthermore, the form of mesorectal tissue differed significantly between male and female subjects. In male subjects, measurements in the anteroposterior dimension accurately reflected the volume of mesorectal tissue, while in women, assessment of both the anteroposterior and the size parameters of the mesorectum from the left to right were required for the best evaluation of the volume of mesorectal tissue. The amount of fat posterior to the rectum was significantly more in men than in women, with or without consideration of length of the pelvis. Finally, the contour of the mesorectal fascia was subject to impression by other nearby visceral organs. There is a great individual variation in the amount of mesorectal fat, and in morphometric parameters between the two sexes. The morphological variations of the mesorectum can be assessed by magnetic resonance imaging using a formula based on two simple measurements of the anteroposterior and left-to-right dimensions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rectal cancer is one of the most common form of large bowel cancer [1, 2]. The prognosis of the disease is related to the stage of the tumor at diagnosis [3]. The degree of mural tumor infiltration, and the presence of local lymph node metastases, vascular invasion, and the extent of extramural spread as well as distance to the mesorectal fascia all influence the prognosis [4, 5].
The mesorectal fat refers to the loose perirectal tissue, while the mesorectal fascia usually denotes the visceral perirectal fascia. The latter is the tissue that ought to be removed intact when a successful total mesorectal excision (TME) for treatment of rectal cancer is contemplated [6, 7]. The importance of these anatomical structures was first brought to attention by the work of Heald et al. in 1982 [8] and this led to a dramatic reduction in local recurrence rates [9].
Ever since the importance of this anatomical structure became known, attempts have been made by radiologists to convey to the surgeon in the most accurate manner the necessary information about the relation of the tumor to the fascia [10, 11]. Indeed, after knowledge of the extension of the tumor to nearby structures, endangered perirectal visceral fascia is the most valuable information that the radiologist can provide the surgeon and/or oncologist preoperatively, regarding the local staging of rectal adenocarcinoma [10, 11]. This information will have an impact on the decision as to how to perform the surgical procedure as well as whether neoadjuvant therapy should be administered [2].
Previous studies have explored the relationship of the mesorectal fascia and encroachment of the tumor on it by magnetic resonance imaging (MRI) [12–15], yet there has been no work done to describe the form, shape and configuration of the mesorectum. In the following work, the structure of mesorectal fatty tissue with regard to shape and configuration was studied by state-of-the-art high-resolution pelvic MRI. It was our hypothesis that the morphology of the mesorectum could be morphometrically approximated in a simple fashion.
Materials and methods
Included in the study were 25 consecutive adult patients without exclusion criteria studied with high-resolution pelvic MRI for various indications. Patients with previous abdominal or pelvic surgery, previous or ongoing local radiotherapy, large (>3 cm any diameter) pelvic tumors (because of the fear of disturbing the normal anatomy), and patients with congenital anomalies were excluded.
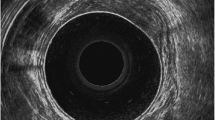
Pelvic MRI examinations were performed on a 1.5-T system (Philips Intera, Best, The Netherlands) using either a four-channel body phased-array coil or a five-channel cardiac phased-array surface coil. In addition to localizer images, sagittal and transaxial T2-weighted turbo spin-echo sequences were performed. A transaxial three-dimensional T1-weighted sequence gradient-echo with 2-mm slice thickness [TR/TE 9.3/4.6, matrix size 205/256, FOV 240, RFOV (rectangular field of view) 80%, NSA (number of signal averages) 2, flip 10°] was performed from the promontory to the lower level of the pubic symphysis.
Image preparation
The three-dimensional T1-weighted sequence was chosen for the morphometric analysis. From the data set, axial reformatted images perpendicular to the long axis of the rectum with 10-mm interval were created which served as the basis for the quantitative measurements. In cases where the boundaries of the mesorectal fascia were not clear cut on the reformatted images, the original acquisitions were reviewed for guidance. The analysis was performed on a dedicated workstation (Easy Vision, Philips, Best, Netherlands).
Quantitative measurements
On each axial reformatted image the measurements shown in Fig. 1 were made. The measurements were defined as follows:
- AA:
-
The most anterior portion of the outer wall of rectum was identified, and then an anteroposterior, i.e. parasagittal, line was drawn until the line made contact with the anterior part of the mesorectal fascia (Fig. 1a). AA was defined as the distance between the most anterior point of the rectum and the intersection of the parasagittal line with the mesorectal fascia.
- PP, RR, and LL:
-
Correspondingly derived from the posterior, right and left outer wall of the rectum to the outer border of the mesorectal fascia, respectively (Fig. 1a).
- AP:
-
The distance between the most anterior part of the fascia and the most posterior part of the fascia interpolated on a parasagittal plane (Fig. 1b).
- RL:
-
Defined in a similar manner to AP, but in the right to left (coronal plane) direction (Fig. 1b).
- Area:
-
For each slice the area occupied by the whole fascia was measured by planimetry on the software provided by the manufacturer (Easy Vision) (Fig. 1c). This was done manually by one of the authors (M.R.T.).
The total mesorectal volume (which also included the volume occupied by rectum) was derived from the summation of the measured areas and multiplication by the thickness of the slices (10 mm).
Simply adding or multiplying the above-mentioned values leads to the combined variables, e.g. AP + RL is derived by adding AP and RL values.
Semiquantitative measurements
In the craniocaudal direction, the first slices that showed the following structures in relation to the anterior border of the S1-2 disc (disc between the first and the second sacral vertebrae) in the midsagittal plane were noted: a complete circular mesorectum, the upper part of the rectum, and the pelvic floor musculature as the muscles approached to make the puborectal ring. The last slice where the fatty tissue surrounding the rectum was no longer visible (defined as anorectal junction on axial images) was also noted. The upper part of rectum was defined as the junction between the sigmoid colon and the rectum. This junction was defined when the posterior part of rectum was no longer intraperitoneal.
Qualitative measurements
Special note was made regarding the interface between other visceral organs and mesorectal fascia. These structures included: the intestines, the female genitalia, the urinary bladder in the male, the seminal vesicles, the prostate and ascites (when present). The interface was noted as convex or concave if the indentations were convex or concave in relation to the mesorectal fascia.
Ethics
The study was approved by the local ethics committee.
Statistics
For statistical purposes, Microsoft Office 2000 Excel was used. In addition, linear stepwise regression was calculated for significant (P<0.05) independent single determinants of the mesorectal volume. Finally, a t-test and Mann-Whitney U-test were used for comparison between male and female patients depending on whether or not the distribution followed a normal pattern.
Results
Of the 25 patients, 12 were female and 13 male. Patients ranged in age from 30 to 88 years at the time of MRI examination, with a mean age of 63 years. Unintentionally, the men were found to be older than the women (P=0.003, Fig. 2a).
Quantitative measurements
Area
A total of 214 areas were measured. The axial area ranged from 320 to 5992 mm2, with a mean of 1798.36 mm2 and standard deviation of 1223.83 mm2 (Table 1 and Fig. 2). There was no significant difference between genders regarding the measured areas.
Volume
The volume ranged from 54,300 to 322,570 mm3 (92,070–322,570 for men and 54,300–188,470 for women), with a mean of 153,949.2 mm3 (181,667.7 for men and 123,900 for women), and standard deviation of 65,390.1 mm3 (70,110.7 for men and 45,538.4 for women). The difference in mesorectal volume between men and women (Fig. 2b) was significant (P=0.038).
The remaining results are shown in Table 1, which shows the correlation between each individual parameter as defined above and the area occupied by mesorectal tissue on the same plane. The highest correlation (non-adjusted r) was observed for AP alone, or when this parameter was added to or multiplied by RL (0.92–0.96). The lowest correlation was observed for AA, RR and LL (0.56–0.57). Table 2 shows the adjusted correlation coefficients and the results of the linear stepwise regression analysis for mesorectal volume for independent significant (P<0.05) determinants. Among the single parameters (AA, PP, RR, LL, AP and RL), only PP showed statistically significant differences (P<0.05) between men and women (P=0.003, Fig. 2c). Figure 3 shows the trend between the total volume and the AP diameter in different patients. AP measured 4 cm below the level of S1-2 disc showed the highest independent adjusted correlation coefficient among the single parameters. The next most significant independent determinant was RL measured at 7 cm below the level of S1-2.
As shown in Fig. 4, the largest axial area occupied by the mesorectal tissue was located at an axial level 7 cm caudal to the level of S1-2 in 16 of the patients who had the largest volume of mesorectal tissue. In these patients, the mesorectal area tapered cranially as well as caudally in a smooth and rather predictable fashion. In six patients, the mesorectal tissue was more flat in the middle part, with a shift of the point of maximum area to a lower level (8–10 cm from S1-2). Finally, in the group with the smallest mesorectal volume, the mesorectal area curve showed a rather flattened dumb-bell configuration. Thus it seems that larger mesorectal volumes are generally bulkier higher up (cranially) than smaller mesorectal volumes.
Semiqualitative measurements
The rectum was recognized as a discernible structure on the plane 1–4 cm caudally from the plane of S1-2, with a mean of 2.56 cm. A complete circular mesorectal fascia could be identified 1–4 cm from S1-2 with a mean distance of 2.26 cm vertically from S1-2. Fat surrounding the rectum, at least partially, could be followed at least 8–12 cm from S1-2 with a mean of 10.12 cm. The mean length of the rectum on a vertical axis was thus 7.76 cm with a range of 5–9 cm and a standard deviation of 1.13. There was no significant difference in the above-mentioned measurements between the two sexes.
Qualitative assessments
The intestines caused varying degrees of convex indentations toward the mesorectal fat in 22 patients (10 men and 11 women; Fig. 5). The female genitalia caused mesorectal indentations in 10 patients, while the prostate and seminal vesicles were responsible for similar changes in 11 patients. Most prominent was the effect of ascites in two women, which made a convex interface with mesorectal fat (Fig. 6).
Discussion
It should be noted that the volume of mesorectal tissue mentioned below includes the rectum itself. The reason that we did not deduct the size of the rectum from some of the above-mentioned parameters was that during rectal cancer surgery both the rectum and the surrounding mesorectum are removed. Nevertheless, for the sake of simplicity, the term mesorectal volume has been adopted in this article.
AA and PP
AA was the shortest parameter studied, although in some patients PP was smaller than AA. The youngest patient (30 years of age) showed 0 AA (no discernible fat present anterior to the most ventral part of the rectum) throughout the whole mesorectum, and interestingly also showed the smallest mesorectal volume (54,300 mm3). On the other hand, the patient with the largest sum of AAs (a male patient) had the next largest volume of mesorectal tissue (316,810 mm3). The correlation between the summed PP and the area occupied by the mesorectal tissue was interesting. While female patients showed virtually no correlation (r=−0.11), the male patients showed a rather strong correlation (r=0.86). Since the degree of correlation between the sum of APs and volume was also great among men, we assumed that the sums of PPs and APs are correlated (r=0.85). Yet, while the sums of AAs showed a correlation with the sums of APs (r=0.85), the correlation between AAs and volume was not as impressive (r=0.70). Another interesting and unexpected finding was the difference in the amount of fat between the two sexes. Male subjects showed not only more fat tissue dorsum to the rectum in total, but also per axial plane. The clinical relevance of this observation, if any, is impossible to ascertain with this study. This is more interesting in light of the fact that no other parameters showed such a significant difference (except for total volume).
RR and LL
The amount of mesorectal fat to each side of the rectum was apparently more than the amount of fat present either anteriorly or posteriorly, and this applied to both men and women. It appeared that the amount of fat was more to the left of the rectum than the right, but this was not statistically significant.
AP and RL
Individual slice AP, AP + RL, and AP × RL all showed a high correlation (r≥0.92) for individual same-slice areas for all patients. For men, there was a good correlation between the sum of (AP + RL), the sum of (AP × RL) and mesorectal volume. In women the sum of RLs showed almost the same correlation with volume (r=0.84) as the sum of APs (r=0.83), in contrast to men who show a stronger correlation for the sum of APs (r=0.94) compared to the sum of RLs (r=0.75). There were no significant differences in AP, RL, sum of APs and sum of RLs between the two sexes.
Qualitative assessment
Exactly how important the impressions into the fat and fascia surrounding the rectum mentioned above are cannot be determined with this study. We have to remember that our patients were all studied in the supine position, which is the normal position for most MRI studies. The extent to which our observations depended on the body position is difficult to estimate, but it would be reasonable to assume that at least some organs would have less influence on posterior structures in the prone position. Nevertheless, we spend a great deal of our daily time in the upright position, further complicating these observations. From these results one may question whether what is reported as the distance of a rectal tumor from the mesorectal fascia is in fact something permanent, and if it is dependent on other factors and then to what extent. The rectum itself is a dynamic organ, which not only moves but also shows various degrees of dilatation.
Anatomically, the rectum does not begin at the level of the sacral promontory in the supine position. In all our patients the mesorectum and rectum began at least one slice (10-mm thick slices) below S1-2. The indication for preoperative radiotherapy in rectal adenocarcinoma is to reduce local recurrence by killing tumor cells inside the mesorectal fat. As shown in another study by our group (submitted for publication), an important factor contributing to local relapse of rectal cancer is incomplete surgical removal of mesorectal fatty tissue. This shows once again how important is the role of mesorectum, and how essential it is to target the right field in the course of preoperative radiotherapy. An implication of our observations would be that the policy of having the radiation field begin above the level of the sacral promontory could, at least theoretically, lead to over-treatment. Despite this, the empirical radiotherapy fields have been tested, though with some variation, in large studies [16]. Furthermore, the number of our patients was small, and the main purpose of our study was not evaluation of the radiation field. Prudently, any suggestion that the field could be reduced at least cranially must be evaluated in large studies.
When performing local staging of rectal carcinoma, the degree of extramural extension has been shown to correlate with prognosis [3, 10]. MRI can assess this extension [2]. Furthermore, the distance between the encroaching tumor and the mesorectal fascia has proven to be significant factor. AA, PP, RR and LL, could influence the mesorectal size when performing local staging of rectal adenocarcinoma. For instance, a very short AA could mean that an anteriorly situated tumor could easily compromise the anterior part of mesorectal fascia despite a minor extramural tumor extension. The results here show that there is some degree of correlation between some of these parameters and the area of mesorectum at the same level (r=0.56–0.62). Does this mean that the total amount of perirectal space and fat have at best only a moderate effect on surgical outcome?
Summary
The space referred to as the mesorectum is occupied by vascular structures, lymphatic and blood vessels, neurons, the rectum itself and usually small lymph nodes embedded in the fatty tissue. This study showed that the space occupied by these structures not only shows a high degree of variability, but also gives way to pressure in the form of indentations caused by normal as well as pathological space-occupying processes. Our findings indicate that an approximation of the total amount of mesorectal tissue can be made by a simple formula measuring the anteroposterior diameter of mesorectal fat 4 cm below S1-2 and the right-to-left diameter 7 cm below the S1-2 disc. The amount of fat behind the rectum as well as the anteroposterior diameter of the mesorectal fascia provide a rather good approximation of the total amount of mesorectal volume or area in men while the correlation is non-existent (dorsal fat) or weaker (anteroposterior diameter) in females. Among the parameters calculated for a single axial section of the pelvis, the highest correlation was seen for the anteroposterior diameter at the level 4 cm below S1-2.
Our findings also indicate that among those with a larger mesorectal volume the largest area is about 7 cm from the level of S1-2 with smooth tapering above and below, while in those with the smallest mesorectal volumes the configuration is more like a flattened dumb-bell. For those in between, the configuration is still that of a hump with the maximum area located at a lower level in the pelvis (mostly 8–9 cm from S1-2). Finally our data show that mesorectal fat and tissue are probably subject to mechanical pressure from the surrounding structures and processes. While we have not studied the consequences and ramifications of such pliability of the mesorectum, we can assume that there should be variability over time in each individual patient. If this is true, then the distance measured from the tumor to the mesorectal fascia could also be subject to variation. Whether these variations could explain the discrepancies between MRI results and those of histopathology has to be further investigated.
References
Faivre J, Bouvier AM, Bonithon-Kopp C (2002) Epidemiology and screening of colorectal cancer. Best Pract Res Clin Gastroenterol 16(2):187–199
Elmas N, Killi RM, Sever A (2002) Colorectal carcinoma: radiological diagnosis and staging. Eur J Radiol 42(3):206–223
Bernick PE, Wong WD (2000) Staging: what makes sense? Can the pathologist help? Surg Oncol Clin N Am 9(4):703–720
Hermanek P, Wiebelt H, Staimmer D, Riedl S (1995) Prognostic factors of rectum carcinoma—experience of the German multicentre study SGCRC. German Study Group Colo-rectal Carcinoma. Tumori 81(3 Suppl):60–64
Quirke P, Dixon MF (1988) The prediction of local recurrence in rectal adenocarcinoma by histopathological examination. Int J Colorectal Dis 3(2):127–131
Rullier E, Laurent C (2003) Advances in surgical treatment of rectal cancer. Minerva Chir 58(4):459–457
Kapiteijn E, van de Velde CJ (2002) The role of total mesorectal excision in the management of rectal cancer. Surg Clin North Am 82(5):995–1007
Heald RJ, Husband EM, Ryall DH (1982) The mesorectum in rectal cancer surgery—the clue to pelvic recurrence. Br J Surg 69(10):613–616
Martling AL, Holm T, Rutqvist LE, Moran BJ, Heald RJ, Cedemark B (2000) Effect of a surgical training programme on outcome of rectal cancer in the County of Stockholm. Stockholm Colorectal Cancer Study Group, Basingstoke Bowel Cancer Research Project. Lancet 356 (9224):93–96
Wiggers T, van de Velde CJ (2002) The circumferential margin in rectal cancer. Recommendations based on the Dutch Total Mesorectal Excision Study. Eur J Cancer 38(7):973–976
Brown G, Radcliffe AG, Newcombe RG, Dallimore NS, Bourne MW, Williams GT (2003) Preoperative assessment of prognostic factors in rectal cancer using high-resolution magnetic resonance imaging. Br J Surg 90(3):355–364
Brown G, Richards CJ, Newcombe RG, Dallimore NS, Radcliffe AG, Carey DP, Bourne MW, Williams GT (1999) Rectal carcinoma: thin-section MR imaging for staging in 28 patients. Radiology 211(1):215–222
Beets-Tan RG, Beets GL, Vliegen RF, Kessels AG, Van Boven H, De Bruine A, von Meyenfeldt MF, Baeten CG, van Engelshoven JM (2001) Accuracy of magnetic resonance imaging in prediction of tumour-free resection margin in rectal cancer surgery. Lancet 357(9255):497–504
Torkzad M, Lindholm J, Martling A, Blomqvist L (2003) Retrospective measurement of different size parameters of non-radiated rectal cancer on MR images and pathology slides and their comparison. Eur Radiol 13(10):2271–2277
Blomqvist L, Rubio C, Holm T, Machado M, Hindmarsh T (1999) Rectal adenocarcinoma: assessment of tumour involvement of the lateral resection margin by MRI of resected specimen. Br J Radiol 72(853):18–23
Glimelius B, Gronberg H, Jarhult J, Wallgren A, Cavallin-Stahl E (2003) A systematic overview of radiation therapy in rectal cancer. Acta Oncol 42(5–6):476–492
Acknowledgements
The authors would like to express their utmost gratitude for the statistical assistance of Johan Almbrandht and Henrik Hellborg, both from the Oncologic Center, Karolinska University Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Torkzad, M.R., Blomqvist, L. The mesorectum: morphometric assessment with magnetic resonance imaging. Eur Radiol 15, 1184–1191 (2005). https://doi.org/10.1007/s00330-005-2657-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-005-2657-5