Abstract
There are no non-invasive methods to assess the real tumor size in rectal cancer prior to surgery, especially following radio/chemotherapy. Magnetic resonance imaging is gaining increasing acceptance as the primary modality at many centers for evaluation of pelvic malignancies including rectal cancers. The aim of this study was to evaluate if the tumor size as assessed by stereological or metric means on MRI correlates to the corresponding pathologic findings. To our knowledge, no such previous work has been reported in the literature. From the Cancer Register Center, 18 patients in the age range of 39–90 years with rectal cancer who had complete preoperative MR with subsequent giant section pathological examinations of the resected bowel were included. The tumor size was measured on MR and histopathologic specimen using both a stereologic and a metric mode. The measured parameters included the maximum transverse area occupied by the tumor, thickness, width, and the length of tumor and the volume of the tumor measured in two different fashions by the product of area and length (al) or the product of thickness, width, and length (twl). The depth of tumor infiltration (T) and presence of local lymph node metastases (N) were also separately evaluated on the histopathologic specimen. There were 1, 4, 12, and 1 patients with tumor stages T1, T2, T3, and T4, respectively. The mean thickness, width, length, area, and volumes, al and twl, were 1.62, 2.8, and 4.78 cm, and 4.72 cm2, 26.29 cm3, and 20.07 cm3, respectively. Regression curves were drawn for above-mentioned parameters. They showed some correlation with square correlation coefficient measuring between 0.38 and 0.82. The best correlation was seen for area (0.75) and volume measured by the product of area and length of the tumor (0.82). With the formula proposed from this material, we assume that rectal tumors can be measured on MR images using a metric model, especially area and the volume (the product of area and length), and then extrapolated to what we would expect from pathology, hence providing us with a tool where we could measure tumor response after neoadjuvant therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Every year, approximately 1500 patients are diagnosed as having rectal cancer in Sweden (National Cancer Registry, Social Styrelsen, nationellt kvalitetsregister cancer rekti 1999). High-resolution MR imaging has become the modality of choice for in vivo evaluation of rectal tumors at many centers due to the high contrast resolution and the ability to visualize rectal tumors and their relation to the mesorectal fascia [1, 2, 3, 4]. The other non-invasive imaging methods used for evaluation of rectal cancer include transrectal ultrasonography (TRUS), CT, and MR imaging using endorectal coils. Both TRUS and MR imaging with endorectal coils, while being useful for evaluation in early stages of rectal cancer when compared with CT or MR using pelvic phased-array coils, have been shown to have limitations in more advanced cases [3, 5, 6, 7, 8, 9].
Most patients in Sweden who undergo surgery for rectal cancer receive preoperative radiotherapy. Pathology has been considered the gold standard for staging and measurement of rectal cancers, but it provides measurement criteria only after total tumor resection. This has acted as a hindrance for evaluation of tumor size and size changes in vivo. It is still unclear as to whether tumor size and its changes have any impact on morbidity and mortality of rectal cancer, but to our knowledge this question has never been fully addressed in the literature. In order to study different size parameters, one has to assess these parameters and compare them with histopathology. If it is shown that a good correlation between histopathology and non-invasive preoperative assessment of different size parameter exists, one can then correlate these findings with relapse of rectal cancer and survival following treatment with different forms of therapy, and determine if these size parameters have any clinical significance, especially on an individual basis.
Furthermore, by comparing findings on MR images before and after radiotherapy, and with that of histopathology, we might be able to understand the MR findings after radiotherapy better.
The aim of this retrospective study was to evaluate if the tumor size as assessed by stereologic or metric means on MRI correlates to the corresponding pathologic findings. To our knowledge, no such previous work has been reported in the literature.
Patients and methods
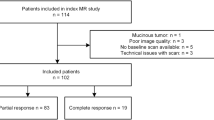
Consecutive patients without radiation therapy prior to surgery for removal of rectal cancer with the intention to cure during the years 1995–2001 at Karolinska Hospital with subsequent histopathological examination of giant sections from the resected specimen were chosen. The number of patients who had undergone surgery was 61. Exclusion criteria included insufficient material for study (no preoperative MRI or missing histopathology specimen in 34 cases), time lapse between surgery and MR examination more than 3 months (3 cases), prior radiation (1 case had received prior pelvic radiation due to gynecologic malignancy), and MRI studies of poor quality due mainly to bowel movement (5 cases). Those with complete pathology and MR examinations formed a final group with 18 patients. The age of the patients ranged between 39 and 90 years at the time of operation with 68 years as both median and mean of the age. The types of operation included anterior resection, Hartmann, and abdominoperineal resection in 8, 5, and 5 patients, respectively. Fifteen of these patients had undergone total mesorectal excision.
The T- and N staging, according to histopathology, were defined according to the definitions made by the American Joint Committee on Cancer Guidelines. The number of lymph nodes with metastasis while reviewing the pathology slides was derived from the original pathological reports.
Preoperative MR imaging was performed on two different 1.5-T systems (General Electric Signa or Philips Intera) using dedicated pelvic or body phased-array surface coils. Sagittal and transaxial T2-weighted (TR 3000–4000 ms and TE 102–119 ms) fast- or turbo-spin-echo sequences were performed with a field of view of 16–24 cm, slice thickness of 5 mm, interslice gap of 0 mm, and a matrix size of 256×192–512×256. Transaxial T1-weighted spin-echo or spoiled gradient-echo images were also performed. In patients with high rectal tumors, oblique T2-weighted sequences perpendicular to the tumor were also performed.
The T2-weigthed images were used for the different measurement parameters. On histopathology, giant sections were processed according to routines described previously [1].
The tumor size was measured both on MRI and axial giant histopathological sections separately by one radiologist (M.T.) and one gastrointestinal pathologist (J.L.). The pathologist, furthermore, assessed the T and N stage on histopathology specimen.
Metric model
Length
Length is the distance between the extremes (the first and the last axial images that show tumor tissue) of the tumor on an axis parallel (oral–aboral) to the rectal lumen in centimeters on MR images. In those cases where such a plane had not been acquired (only 1 case) a reformatted image was post-processed on the workstation (Volume View, Easy Vision, Philips Medical Systems, Eindhoven, The Netherlands). For pathology, the length of the tumor was derived from the reports.
Width and thickness
The section of the study at MRI was defined as the plane that showed the largest burden of tumor mass as perpendicular to the bowel wall as possible. For pathology, the slide, which provided the most abundant tumor tissue, was used. The width was defined as the largest diameter in centimeters occupied on such a plane by the tumor (Fig. 1). In circumferential tumors (partial or total), the distance occupied by the lumen (tumor-free area) was excluded. The thickness was defined as the largest diameter of the tumor in centimeters on the axis perpendicular to the diameter used for measurement of the width.
Area
On the same plane as defined above, the area occupied by the tumor tissue was measured. For this purpose, the stereology method was used. Stereology or random marking technique when applied to measurements of area is based on the count of points of a lattice grid fallen within the boundaries of the area of interest [10, 11]. Presently, the software programs on many workstations permit measurement of area by a process of counting the total number of pixels, otherwise known as planimetry. Planimetry is usually more time-consuming and in certain areas, such as studying hard copies or pathology specimen, it might not be attainable [12]. The lattice grid used here was a checkered grid with two sets of parallel lines perpendicular to each other, also called square lattice grid (Fig. 2). The number of lines were 2 (grid I) or 4 (grid II) on any axis for every centimeter, thus creating 4 and 16 cross points per square centimeter, respectively. Grid I was used primarily except when the number of measured points were fewer than 25, in that case grid II was used. The unit used was square centimeters. The cutoff point of 25 points was based on the results of measurements on surfaces with known surface area and assessment of the least number of points with a safety margin that could provide a reliable and reproducible assessment of that area (not shown here).
From the metric and stereologic definitions given above, the following parameters were calculated:
-
Volume (al)=area×length (measured in cm3)
-
Volume (twl)=width×thickness×length (measured in cm3)
-
Thickness+width=width+thickness.
The term volume is somewhat of a misnomer. We did not try to measure the tumor volume but instead defined two calculated parameters that take several measurements on different axes into consideration, and for the sake of convenience the term volume was adopted. Every measurement was repeated twice. In cases where the difference between measurements exceeded 10%, another series of measurements were done and a consensus was reached. In cases where the difference was not larger than 10% the difference was considered negligible and an average was obtained.
For statistical purposes, the p value, the Pearson product-moment correlation coefficient (r), and the confidence interval (CI) were calculated for all measurements.
The local ethics committee approved the study.
Results
According to histopathology, there were 1, 4, 12, and 1 patients with T-stages T1, T2, T3, and T4, respectively. None of the T1 and T2 cases showed local metastatic lymphadenopathy. The patients in the T3 stage showed different N stages with 4, 4, 3, and 1 patients in the N0, N1, N2, and N3 stages, respectively. Half of our patients (nine) did not have regiolocal metastatic lymphadenopathy. The only patient in the T4 stage showed metastasis along the course of major vessels of the pelvis (N3).
The mean (median and range) thickness, width, length, area, and volumes, al and twl, on histopathology were 1.62 cm (1.35, 0.3–3.8 cm), 2.8 cm (2.83, 1.5–5.2 cm), 4.78 cm (4.5, 2–8.5 cm), 4.72 cm (3.50, 0.81–11.5 cm2), 26.29 cm2 (17.54, 1.62–97.5 cm2), and 20.07 cm2 (17.5, 1.35–88.4 cm2), respectively. The results of measurements of different tumor size parameters are shown in Table 1.
For all measurements, least-squares regression curves were defined (scatter diagrams shown in Figs. 3, 4, 5, 6, 7, 8, 9). The regression lines are shown in Table 2.
The measured p values for all measurements were larger than 2.120 (the value of t for p<0.05 with 16 degrees of freedom), meaning that it is unlikely that this sample was drawn from a population without any existing relationship between the measured parameters. The Pearson product-moment correlation coefficient (r) and the confidence interval (CI) were calculated, the results of which are shown in Table 3. The best r2 was observed for area (0.75) and volume measured by the product of area and length of the tumor (0.82).
Discussion
During the past two decades we have witnessed great improvements in terms of treatment of rectal cancer due to several factors including better preoperative assessment, better surgical techniques, and more efficacious neoadjuvant therapy [13]; hence, the mortality and relapse rates (<5%) have decreased making studies based on follow-up of patients more difficult. In order to circumvent this problem, there has been a surge of multi-center studies that try to solve the problem by compiling the material obtained.
A direct approach comprising an assessment before and after neoadjuvant therapy, although not as perfect as studies based on rates of mortality and tumor relapse, do offer some advantages. They could be used on an individual basis informing us of the benefit(s) of treatment for any individual patient. In addition, when comparing different forms of neoadjuvant therapy they are able to isolate the effects of therapy and diminish the effects of confounding factors such as surgeon and/or surgical techniques. Finally, in clinical trials they could use the whole group of patients (increasing the number of patients being compared) and decrease the time required to execute a study, i.e., comparison of the status before initiation of therapy vs preoperative (imaging studies) or post-operative (pathology) studies instead of several years of follow-up. Pathology is able to study tumors in this regard only after tumor removal [14], limiting the benefits of this gold standard of tumor assessment.
In this study we tried to define different size parameters and measured them on both histopathology specimens as well MR images. Our results show that there exists a trend between the parameters area and volume (al) measured on MRI and pathology specimen [15].
One other potential benefit of such measurements could be to act as a complement to T staging of the rectal tumor. It has become increasingly more recognized by us that T3 stage is a heterogeneous group as it regards the prognosis and most probably even treatment [16, 17]. Merkel and colleagues [17] have addressed the issue of how much a tumor has breached the muscularis propria, whereas Beets Tan et al [18] have looked at the distance between the tumor and mesorectal fascia. The radial margin status seems to have a direct impact on the prognosis [19].
Another potential benefit of such metric measurements would be a more objective mathematical description of tumor shape. For instance, between two tumors showing almost identical values for thickness and width, the tumor showing the larger value for area is most probably more globular/nodular and the tumor with the smaller area is most likely a spiculated tumor. The pattern of growth of rectal cancer and, accordingly, its shape seem to bear some significance as it pertains to prognosis [20, 21, 22]. We have come to appreciate the difficulties associated with deciding whether this streaking is a desmoplastic reaction, fibrous tissue, or a harbinger of a more malignant nature [23]. On the other hand, a nodular rectal cancer is considered malignant in all of its nodular area. By virtue of size determinants, we would be able to objectively define if any tumor shows characteristics typical of each such group. Still, it might be difficult to differentiate vital tumor tissue from necrotic or fibrotic areas.
Perhaps the most important advantage of our study would mainly be a comparison of the images before neoadjuvant treatment and the amount of tumor tissue on pathology specimen removed by the surgeon. Such a comparison is possible by virtue of extrapolating the MRI findings into pathology findings. Conversely, by conducting an MRI study of patients after radiotherapy and directly before surgery and its comparison with the findings on pathology, we would be able to understand the changes induced by radiotherapy on MRI. A drawback to such assumptions is that we still do not know how much of a tumor is considered critical in order to modify or change the treatment.
There were some drawbacks to this study. Our patients were selected on the basis that they did not receive preoperative radiotherapy. While important, this probably had no impact on the nature of this study concerning itself with size and different measurement parameters primarily. At the same time, radiotherapy introduces a new confounding factor regarding anatomy. Accordingly, these patients were those among whom a decision for surgical treatment with the intention to cure had been made implying that preoperative staging had been favorable.
Another drawback was that this study did not deal with controlled subjects. Especially with regard to pathology specimen we did not define exact matches for our MRI sections. It is possible that some slides that showed the most abundant tumor mass were in fact missing or never prepared, e.g., the pathologist had chosen the part that showed most tumor invasion (not necessarily the same as the most abundant tumor tissue). Some parameters (i.e., length of the specimen according to pathology and it derivatives) were extracted from the original report and are amenable to scrutiny afterwards. Despite these circumstances, we were able to show a good correlation between area and volume (al) of the tumors measured on MRI and histopathology, which shows that even in uncontrolled specimen an extrapolation of MR findings into pathologic findings, and vice versa, is possible. We believe that these parameters showed the best correlation because they take into account several dimensions, thus offsetting some of the problems caused by different tissue sampling and imaging planes. Moreover, we understand which parameters showed the least correlation, and among those that showed better correlation how strong this correlation is. Despite this, the individual differences were appreciable, something that any investigator should bear in mind, especially in everyday clinical decision making.
Conclusion
In conclusion, the results from this study show that rectal tumors can be measured on MR images with results that correlate with histopathology when the tumor is metrically measured as the product of maximum transverse area and length of the tumor.
References
Blomqvist L, Holm T, Rubio C, Hindmarsh T (1997) Rectal tumors: MR imaging with endorectal and/or phased-array coils, and histopathological staging on giant sections. A comparative study. Acta Radiol 38:437–444
Gagliardi G, Bayar S, Smith R, Salem RR (2002) Preoperative staging of rectal cancer using magnetic resonance imaging with external phase-arrayed coils. Arch Surg 137:447–451
Thoeni RF (1997) Colorectal cancer. Radiologic staging. Radiol Clin North Am 35:457–485
Kim NK, Kim MJ, Park JK, Park SI, Min JS (2000) Preoperative staging of rectal cancer with MRI accuracy and usefulness. Ann Surg Oncol 7:732–737
Blomqvist L, Machado M, Rubio C, Gabrielsson N, Granqvist S, Goldman S, Holm T (2000) Rectal tumour staging: MR imaging using pelvic phased-array and endorectal coils vs endoscopic ultrasonography. Eur Radiol 10:653–660
Akasu T, Sugihara K, Moriya Y, Fujita S (1997) Limitations and pitfalls of transrectal ultrasonography for staging of rectal cancer. Dis Colon Rectum 40:S10–S15
Ramana KN, Murthy PV, Rao KP, Bhagawanulu, Mandapal T, Pratap B (1997) Transrectal ultrasonography versus computed tomography in staging rectal carcinoma. Indian J Gastroenterol 16:142–143
Blomqvist L, Holm T, Nyren S, Svanstrom R, Ulvskog Y, Iselius L (2002) MR imaging and computed tomography in patients with rectal tumours clinically judged as locally advanced. Clin Radiol 57:211–218
Osti MF, Padovan FS, Pirolli C, Sbarbati S, Tombolini V, Meli C, Enrici RM (1997) Comparison between transrectal ultrasonography and computed tomography with rectal inflation of gas in preoperative staging of lower rectal cancer. Eur Radiol 7:26–30
Ladekarl M, Jensen V, Nielsen B (1996) Stereologic estimation of breast tumor size. Anal Quant Cytol Histol 18:151–157
Mazonakis M, Damilakis J, Maris T, Prassaopoulos P, Gourtsoyiannis N (2000) Estimation of spleen volume using MR imaging and a random marking technique. Eur Radiol 10:1899–1903
Savnik A, Bliddal H, Nyengaard JR, Thomsen KS (2000) MRI of the arthritic finger joints: synovial membrane volume determination, a manual vs a stereologic method. Eur Radiol 12:94–98
Blumberg D, Ramanthan RK (2002) Treatment of colon and rectal cancer. J Clin Gastroenterol 34:15–26
Graf W, Dahlberg M, Mazloum OM, Holmberg L, Påhlman L, Glimelius B (1997) Short-term preoperative radiotherapy results in down-staging of rectal cancer: a study of 1316 patients. Radiother Oncol 43:133–137
Bauer J, Gries W, Bahmer FA (1995) Volume estimation of multicellular colon carcinoma spheroids using Cavalier's principle. Path Res Pract 191:1192–1197
Merkel S, Mansmann U, Siassi M, Papadopoulos T, Hohenberger W, Hermanek P (2001) The prognostic inhomogeneity of colorectal carcinomas stage III. Cancer 92:2754–2759
Merkel S, Mansmann U, Papadopoulos T, Wittekind C, Hohenberger W, Hermanek P (2001) The prognostic inhomogeneity in pT3 rectal carcinomas. Int J Colorectal Dis 16:298–304
Beets Tan RGH, Beets GL, Vliegen RFA, Kessels AGH, Van Boven H, De Bruine A, Meyenfeldt MF von, Baeten CGM, van Engelshoven JMA (2001) Accuracy of magnetic resonance imaging in prediction of tumor-free resection margin in rectal cancer surgery. Lancet 357:497–504
Compton CC, Fielding LP, Bugart LJ, Conley B, Cooper HS, Hamilton SR, Hammond SR, Hammond ME, Henson DE, Hutter RV, Nagle RB, Nielsen ML, Sargent DJ, Taylor CR, Welton M, Willett C (2000) Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 124:979–994
Michelassi F, Vannucci L, Montag A, Goldberg R, Chappel R, Dytch H, Bibbo M, Block GE (1998) Importance of tumor morphology for the long term prognosis of rectal adenocarcinoma. Am Surg 54:376–379
Roncucci L, Fante R, Losi L, Gregorio C di, Micheli A, Benatti P, Madenis N, Ganazzi D, Cassindari MT, Lauriola P, Ponz de Leon M (1996) Survival for colon and rectal cancer in a population-based cancer registry. Eur J Cancer 32A:295–302
Brodsky JT, Richard GK, Cohen AM, Minsky BD (1992) Variables correlated with the risk of lymph node metastasis in early rectal cancer. Cancer 69:322–326
Brown G, Richards CJ, Newcombe RG, Dallimore NS, Radcliffe AG, Carey DP, Bourne MW, Williams GT (1992) Rectal carcinoma: thin-section MR imaging for staging in 28 patients. Radiology 211:215–222
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Torkzad, M., Lindholm, J., Martling, A. et al. Retrospective measurement of different size parameters of non-radiated rectal cancer on MR images and pathology slides and their comparison. Eur Radiol 13, 2271–2277 (2003). https://doi.org/10.1007/s00330-003-1898-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-003-1898-4