Abstract
The aim of the study was to evaluate safety and feasibility of dobutamine cardiovascular magnetic resonance (CMR) in patients with proven or suspected coronary artery disease. Dobutamine CMR was evaluated retrospectively in 400 consecutive patients with suspicion of myocardial ischemia. Dobutamine was infused using an incremental protocol up to 40 μg/kg body weight per minute. All anti-anginal medication was stopped 4 days before the CMR study and infusion time of dobutamine was 6 min per stage. Hemodynamic data, CMR findings and side effects were reported. Patients with contraindications to CMR (metallic implants and claustrophobia) were excluded from analysis. Dobutamine CMR was successfully performed in 355 (89%) patients. Forty-five (11%) patients could not be investigated adequately because of non-cardiac side effects in 29 (7%) and cardiac side effects in 16 (4%) patients. Hypotension (1.5%) and arrhythmias (1%) were the most frequent cardiac side effects. One patient developed a severe complication (ventricular fibrillation) at the end of the study. There were no myocardial infarctions or fatal complications of the stress test. The most frequent non-cardiac side effects were nausea, vomiting and claustrophobia. Age >70 years, prior myocardial infarction and rest wall motion abnormalities showed no significant differences with side effects (P>0.05). Dobutamine CMR is safe and feasible in patients with suspicion of myocardial ischemia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dobutamine cardiovascular magnetic resonance imaging (CMR) is used to identify wall motion abnormalities of the left ventricle, indicative of myocardial ischemia in patients with proven or suspected coronary artery disease [1–4]. According to international guidelines, dobutamine is used to analyze wall motion abnormalities, while adenosine is mainly used to analyze perfusion abnormalities of the myocardium [5, 6]. Recent studies show that CMR is gaining an important role in diagnosing patients suspected of coronary artery disease [7–9]. With the use of myocardial tagging, dobutamine CMR has emerged as a reliable modality to detect myocardial ischemia and provide prognostic information as well [4, 10]. The presence of resting wall motion abnormalities (RWMA), in the absence of myocardial ischemia, has been shown to be a high risk factor for the development of future major cardiac adverse events [4]; however, the relation of RWMA to side effects during the dobutamine CMR study is unknown. No large clinical experience for the evaluation of side effects during dobutamine CMR has been reported so far. The purpose of the present study was to assess the safety and feasibility of dobutamine CMR over a period of 4 years at a single center.
Materials and methods
Study population
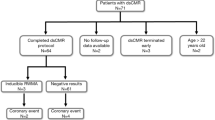
Between August 1999 and July 2003, 400 consecutive dobutamine CMR studies were acquired in our institution. Demographic and hemodynamic data were collected retrospectively. The patients were recruited from the outpatient clinic of the Department of Cardiology. All patients had chest pain and an inconclusive diagnosis of myocardial ischemia by means of history, ECG recording at rest and, if performed, during a bicycle exercise test. Patients with an acute coronary syndrome, atrial fibrillation, severe arterial hypertension (>220/120 mmHg), CMR-incompatible metallic implants or known claustrophobia were excluded from analysis. Many patients had known coronary artery disease, including previous myocardial infarction (37%), previous coronary revascularization (19%) or were receiving beta blockers (58%). Diabetes mellitus was present in 16% of the patients (Table 1). The local Ethical Committee approved the study protocol.
Dobutamine CMR protocol
To ensure cardiac response to dobutamine, all anti-anginal medication was stopped 4 days before the dobutamine-stress CMR examination. Before the patient entered the CMR suite, the presence of an acute coronary syndrome was ruled out by a physician. After the patient was positioned on the scanning table, intravenous access was established via an antecubital vein. ECG monitoring leads, a phased-array surface coil covering the heart and a brachial blood pressure cuff were applied. A single-lead ECG was continuously monitored on the MRI console. Systolic and diastolic blood pressures were recorded using an automatic device (Welch-Allyn, Emro-medical) at baseline and every 3 min throughout the procedure. Blood pressure and heart rate were recorded by the technicians throughout the study. The imaging methodology of dobutamine CMR has been described in detail previously [4]. In brief, MRI was performed using a standard 1-T system (Impact-Expert, Siemens Medical Systems, Erlangen). Three short-axis cine breath-hold CMR images of the left ventricle were taken at rest and during incremental dosage of dobutamine up to 40 μg/kg/min. An ECG-triggered segmented gradient-echo pulse sequence was used: FLASH/TR, 90 ms; TE, 6.1 ms; α, 25°; FOV, 325–350 mm; slice-thickness 8 mm; and matrix 256×256. Tagging was performed with a standard FLASH grid-sequence: TR, 96 ms; TE, 4.4 ms; α, 15°; FOV, 325–350 mm; slice-thickness 8 mm and matrix 256×256. Each cine breath-hold acquisition (one slice) took 15–19 heartbeats and was made in maximum inspiration. If the heart rate reached 100 beats per minute, the number of phases per acquisition was decreased to compensate for shortening of RR interval at higher heart rates. The basal plane was taken 1.5 cm below the mitral valves. The midventricular and apical short-axis views were divided equally over the remaining part of the left ventricle. In case a wall motion abnormality (WMA) was detected at baseline, infusion was started with 5 μg/kg/min, after which the dose of dobutamine was increased to 10, 20, 30 and 40 μg/kg/min. If no WMA was detected at baseline, we started with 10 μg/kg/min. Imaging began 6 min after each dose increase and required 3 min per dose increase. Imaging consisted of acquiring three short-axis cine images (basal, mid-ventricular and apical) without and two short-axis cine images (basal and mid-ventricular) with myocardial tagging. The images were scored according to the guidelines of the American Heart Association [11]. Short-axis images were divided into multiple segments with six segments in the basal and midventricular and four segments in the apical image. Segmental wall motion was qualitatively graded as 1, normal or hyperkinesis; 2, hypokinesis; 3, akinesis; 4, dyskinesis. Myocardial ischemia was defined as a new (induced) or worsening WMA in at least two segments at consecutive planes of the left ventricle during infusion of dobutamine. The absence of new or worsening wall motion abnormalities was defined as a negative dobutamine CMR study. A RWMA was defined as hypokinesia, akinesia or dyskinesia in one or more short-axis segments at rest. When new wall motion abnormalities were detected the dobutamine CMR study was followed by coronary angiography.
During the infusion of dobutamine, the radiologist and cardiologist were present in the CMR suite, to monitor the condition of the patient and to evaluate all the images directly. Via a microphone direct contact with the patient was maintained between the scanning of the images and throughout the examination. A defibrillator (not MR compatible) and medication for emergency treatment were present in the preparation room besides the scanner. A physician (cardiologist) trained in cardiovascular emergencies and resuscitation was present in the CMR suite. The condition of the patients was controlled clinically up to 30 min after the end of the dobutamine infusion.
Criteria for ending the dobutamine-CMR examinations were development of new wall motion abnormalities indicative for myocardial ischemia, fall of systolic blood pressure of >40 mmHg, marked hypertension >240/120 mmHg, severe chest pain, arrhythmias and intolerable side effects of dobutamine (nausea, vomiting).
Statistical analysis
Baseline clinical and dobutamine CMR characteristics are given as the mean value ± standard deviation for continuous variables and as a number (percent) for categorical variables. Patients were classified according to cardiac and non-cardiac side effects. Differences in categorical variables were assessed by chi-square analysis. Hemodynamic values were compared using a paired t-test. A P-value of 0.05 or less was considered to indicate statistical significance. The target heart rate (THR) rule was defined as 85% of the maximum exercise heart rate predicted for age and sex (220 minus age in men; 200 minus age in women) [12]. The THR rule was not used during the stress studies. Retrospectively, the data of the acquired heart rates were evaluated in relation to the THR rule and compared with dobutamine CMR findings.
Results
Hemodynamic data and the target heart-rate rule
Dobutamine CMR was successfully performed in 355 (89%) of the patients. The demographic and hemodynamic data are shown in Table 1. The rate-pressure product during dobutamine CMR increased from 11.902±3.506 to 21.169±4.444 (P<0.05), heart rate increased from 79±16 to 125±18 beats per minute (P<0.05) and systolic blood pressure from 149±26 mmHg to 169±27 mmHg (P<0.05). The total duration of the CMR study, including preparation of the patient and scan time, averaged 48 min (SD 11).
Retrospectively, the peak heart rates were evaluated according to the THR rule, which is used frequently in dobutamine stress studies. The values are presented in Table 2. Differentiation was made in three groups: THR±10 beats, >10 beats and <10 beats. The THR was not reached in 93 (35%) of 261 patients with a negative dobutamine CMR study. A major part of the positive dobutamine CMR studies (40%) was found at higher peak heart rates then calculated by the THR rule.
End points of dobutamine CMR studies
Side effects led to premature termination of the procedure in 45 (11%) dobutamine CMR studies (Table 3). Out of 355 patients who completed the infusion protocol without side effects, 94 (26%) had inducible myocardial ischemia. The mean maximum dose of dobutamine for detecting ischemia was 33 μg/kg/min (SD 8.3). The majority of the new wall motion abnormalities (76%) were detected at high-dose dobutamine (30 μg and 40 μg), whereas only 24% were detected at low-dose dobutamine (20 μg). The mean maximum dose of dobutamine of all the patients was 37.8±5 μg/kg/min. Coronary angiography showed significant coronary artery disease in 89 (95%) of these 94 patients. One-vessel disease was found in 32 (36%), and two-vessel or three-vessel disease in 57 (64%) of the patients. During the examinations, 211 (59%) of the patients had chest discomfort, but in only 84 of them (24%) was myocardial ischemia shown to be present. During the examinations, 84 of 94 (89%) of the patients with ischemia developed angina; however, 10 (11%) patients did not reveal any pain sensation. Five of them were known to have diabetes mellitus.
The end of the protocol was reached in 261 (74%) of 355 CMR studies after the maximum dose of dobutamine (40 μg/kg/min) and a negative dobutamine CMR test.
RWMA were detected in 57 (22%) of the 261 patients with a negative dobutamine CMR study. The patients with and without side effects were correlated with RWMA, age >70 years, myocardial infarction and use of beta blockers, 4 days prior to the study (Table 4). No significant differences were found between these characteristics and the appearance of side effects (P>0.05). Nitroglycerin during or at the end of the study was required for four (1%) patients.
Cardiac side effects and test termination
Cardiac side effects and reasons for test termination are shown in Table 3. One (0.25%; 95% CI 0.000016–0.014) major complication (i.e., death, myocardial infarction, or ventricular fibrillation) occurred in 400 patients. This patient developed ventricular fibrillation during infusion of dobutamine (40 μg/kg/min). The patient was successfully resuscitated and recovered well after coronary bypass grafting.
The most frequent minor complication was symptomatic and severe hypotension, which occurred in six (1.4%) patients. All patients completely recovered, usually after discontinuation of dobutamine. Two patients required short-term inpatient observation because of hypotension, bradycardia and severe chest pain. Treatment consisted of sublingual nitroglycerine, fluids and observation. Hypertension (systolic blood pressure >220 mmHg) occurred in one patient. Blood pressure normalized spontaneously after termination of dobutamine infusion.
Arrhythmias developed in four patients (1%): two patients with persistent premature ventricular contractions and two patients with atrial fibrillation. Premature ventricular contractions were seen in six (1.5%) patients, which disappeared in four of them at a higher dose of dobutamine. One patient showed shortness of breath at the onset of the stress study. It was concluded that he had unstable angina, probably the result of stopping his anti-anginal medication. The dobutamine CMR study was not performed and he was admitted to the emergency unit. He recovered well and no myocardial infarction was found. No other side effects were seen in the other 399 patients as the result of stopping the medication.
Non-cardiac side effects and test termination
Non-cardiac side effects occurred in 27 (7%) patients (Table 3). The most common were nausea and or vomiting (2.8%). In nine of ten patients (mean age 66 years), nausea started at a dobutamine dose of 30 μg. Claustrophobia and breath-hold artifacts are typically CMR-related side-effects (3.8%). In three patients there was no heart rate increase during the study due to the fact that the beta blocker medication was not stopped before the study.
Discussion
The present study of 400 consecutive examinations shows that dobutamine CMR is a safe test and well tolerated in the majority of the patients. Feasibility of dobutamine CMR is hampered by claustrophobia and breath-hold imaging artifacts, which are typical CMR side effects. In spite of the pretest screening for claustrophobia, the dobutamine CMR test failed in 2.3% of the patients because of anxiety. The non-cardiac side effects were comparable to those reported by other dobutamine CMR studies [2–4, 10]. If we exclude the typical CMR side effects, including the patients who did not stop their anti-anginal medication, the number of non-cardiac side effects was 2.7%, which is comparable to dobutamine stress echocardiography (DSE) (3%) [13–15]. The use of shorter or more open magnets might reduce the number of patients with claustrophobia in the future.
High-dose dobutamine stress imaging may cause severe complications in about 3 per 1,000, including infarction, ventricular fibrillation and sustained ventricular tachycardia [13–15]. Neither death nor myocardial infarction occurred in this study. Ventricular fibrillation occurred in one patient (0.25%), with good clinical outcome. This 71-year-old man had diabetes mellitus and a history of myocardial infarction 2 years before the study. The cine images at rest showed minor septal wall motion abnormalities of the left ventricle. The myocardium was ischemic at a level of 20 μg and we “overstressed” the patient with higher doses of dobutamine. After review of the images it was obvious that myocardial ischemia was already present at 20 μg and 30 μg, which was not noted during the study. Also, the patient did not report any chest discomfort or pain during the study, probably the result of the presence of diabetes. According to our experience, it is advisable to test safety and emergency procedures regularly, together with the MR technicians.
The most frequent cardiac side effects in this study were hypotension and arrhythmias, which were well tolerated and comparable to DSE [13–15]. The cardiac side effects seem not to be the result of stopping all anti-anginal medication 4 days before the study. Only one patient had unstable angina prior to the dobutamine CMR study and was admitted for 1 day to the hospital. The dobutamine CMR study, which was performed 2 weeks later, showed inducible ischemia. Although patients were subjected to a prolonged dobutamine infusion protocol, only one patient developed hypertension necessitating termination of the study. The remaining dobutamine-related side effects seem to be comparable to those reported for DSE [13–15], which favors a prolonged infusion protocol like the one used in this study.
Safety of CMR protocol
The most important limitation of current CMR technology is inadequate monitoring and concern over patient safety. Routine clinical performance of dobutamine CMR requires detection of arrhythmias and inducible ischemia [16]. In dobutamine CMR, the ECG is used to monitor heart rate and rhythm and not to analyze ST segments to diagnose ischemia. Myocardial ischemia is detected by analyzing changes in systolic wall motion of the left ventricle, which generally precede ECG changes and chest pain [17, 18]. Patients must perform repeated breath-holds of about 6–12 s throughout the study, which may hinder communication with the patient. The acquired images reflect only a short period of wall motion during the infusion of dobutamine. So the onset of myocardial ischemia can be masked for several minutes. Stress echocardiography overcomes all the above-mentioned safety issues. Real time CMR imaging in the new generation CMR scanners will overcome this problem [19, 20]. Continuous evaluation of the left ventricle will create an additional safety margin for the detection of ischemia and arrhythmias.
Feasibility of dobutamine protocol
In this study, a different stress protocol was used compared to the methods in previously reported high-dose dobutamine CMR studies [2, 3]. To ensure cardial response to dobutamine, we stopped all anti-anginal medication 4 days before the dobutamine CMR examination. In most imaging protocols, beta blocker medication is withhold only 1 day before the study and atropine is applied to increase heart rate in patients who fail to reach the THR [2, 3, 21]. A recent report showed that the presence and severity of CAD may be underestimated in patients receiving beta blocker therapy [22]. Most of our patients use beta blockers (metoprolol) with long half-lives (e.g., 20 h) and should be stopped at least 3–4 days to minimize their activity. The risk of beta blocker withdrawal, including severe hypertension or an unstable coronary syndrome, is mainly based on literature regarding propranolol [23–25], which is not used in our institution for the treatment of angina pectoris and myocardial ischemia. In our study, only one patient appeared to have an acute coronary syndrome before the start of the study.
During the stress studies, the THR rule was not applied to this group of patients. In cardiac stress testing, this equation provides an approximation of the maximal heart rate to be reached at peak aerobic exercise, whereas dobutamine stress imaging aims to uncover wall motion abnormalities by increasing contractility and heart rate and by creating flow heterogeneity between myocardial regions subtended by normal coronary arteries and those subtended by stenotic coronary arteries. However, the variance of the maximal heart rate for any given age is considerable [26]. The main source of error is that there is a significant reduction and variability in heart rate with increasing age, particularly in patients with coronary artery disease [26, 27]. Peak heart rate by itself is an unreliable index of relative load [12]. The chronotropic and inotropic reserve of the heart defines the myocardial aerobic capacity, which is estimated by the product of the heart rate and the systolic blood pressure. Measurements of the rate-pressure product during exercise make it feasible to determine in the individual patient the threshold of myocardial ischemia [27]. The peak rate-pressure product in this study was similar to that reported by other dobutamine stress studies [2, 21], which indicate that in this study the stress level was at least as high as reported in former studies.
Chronotropic incompetence (patients who reached a submaximal heart rate) according to THR rule was present in 33% of the patients (Table 2), which is similar to previous reports [28]. Elhendy et al. reported that premature ventricular contractions occurred more commonly in patients with chronotropic incompetence, with the exception of other forms of arrhythmias [28], which are comparable to our findings. In this study, four patients who revealed a submaximal heart rate response in all four studies showed temporary premature ventricular contractions.
In this study, infusion time was prolonged from 3 to 6 min, mainly for imaging reasons. The multiple breath-hold cine CMR sequences (at least five series per infusion level) could not be made within 3 min, and especially older patients need a few minutes rest between the infusion levels to avoid breath-hold artifacts. In our experience, even with the use of a 1.5-T MR system a 3 min infusion interval is too short to perform all these multiple breath-hold cine images. Real-time CMR imaging with sufficient image quality may overcome this problem in the future [29]. There is also an advantage of this 6 min infusion protocol. This prolonged dobutamine infusion protocol induces better steady states of dobutamine. The effect of the additional stress factor of the prolonged infusion time is unknown, but is probably reflected in the high number (40%) of positive studies found at a much higher heart rate than can be calculated by the THR rule. If we had stopped the study at the reached THR, 40% of the positive studies would have been missed.
Conclusions
The results of this single-center study of 400 consecutive studies confirm that the dobutamine CMR protocol is safe and feasible in patients with known or suspected coronary artery disease. Because of potential cardiac side effects, a cardiologist should be present during the studies to monitor potential arrhythmias and complaints of the patients.
References
Pennell DJ, Underwood SR, Manzara CC, Swanton RH, Walker JM, Ell PJ, Longmore DB (1992) Magnetic resonance imaging during dobutamine stress in coronary artery disease. Am J Cardiol 70:34–40
Nagel E, Lehmkuhl HB, Bocksch W, Klein C, Vogel U, Frantz E, Ellmer A, Dreysse S, Fleck E (1999) Noninvasive diagnosis of ischemia-induced wall motion abnormalities with the use of high-dose dobutamine stress MRI: comparison with dobutamine stress echocardiography. Circulation 99:763–770
Hundley WG, Hamilton CA, Thomas MS, Herrington DM, Salido TB, Kitzman DW, Little WC, Link KM (1999) Utility of fast cine magnetic resonance imaging and display for the detection of myocardial ischemia in patients not well suited for second harmonic stress echocardiography. Circulation 100:1697–1702
Kuijpers D, Ho KYJAM, Dijkman PRM van, Vliegenthart R, Oudkerk M (2003) Dobutamine cardiovascular magnetic resonance for the detection of myocardial ischemia using myocardial tagging. Circulation 107:1592–1597
American Heart Association, American College of Cardiology (1997) Guidelines for exercise testing. J Am Coll Cardiol 30:260–315
American Heart Association, American College of cardiology (2002) Guideline update for exercise testing. Circulation 106:1883–1892
Lipton MJ, Bogaert J, Boxt LM, Reba RC (2002) Imaging of ischemic heart disease. Eur Radiol 12:1061–1080
Sandstede JJ (2003) Assessment of myocardial viability by MR imaging. Eur Radiol 13:52–61
Dewey M, Borges AC, Kivelitz D, Taupitz M, Wagner S, Baumann G, Hamm B (2004) Coronary artery disease: new insights and their implications for radiology. Eur Radiol 14:1048–1054
Hundley WG, Morgan TM, Neagle CM, Hamilton CA, Rerkpattanapipat P, Link KM (2002) Magnetic resonance imaging determination of cardiac prognosis. Circulation 106:2328–2333
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging. Circulation 105:539–542
Sheffield LT (1988) Exercise stress test. In: Braunwald E (ed) Heart disease: a textbook of cardiovascular medicine, 4th edn. Saunders, Philadelphia, pp 223–241
Secknus MA, Marwick TH (1997) Evolution of dobutamine echocardiography protocols and indications: safety and side effects in 3,011 studies over 5 years. J Am Coll Cardiol 29:1234–1240
Picano E, Mathias WJ, Pingitore A, Bigi R, Previtali M (1994) Safety and tolerability of dobutamine-atropine stress echocardiography: a prospective multicentre study. Echo dobutamine international cooperative study group. Lancet 344:1190–1192
Mertes H, Sawada SG, Ryan T, Segar DS, Kovacs R, Foltz J, Feigenbaum H (1993) Symptoms, adverse effects and complications associated with dobutamine stress echocardiography. Experience in 1118 patients. Circulation 88:15–19
Zoghbi WA, Barasch E (1999) Dobutamine MRI: a serious contender in pharmacological stress imaging. Circulation 99:730–732
Nesto RW, Kowalchuk GJ (1987) The ischemic cascade: temporal sequence of hemodynamic, electrocardiographic and sypmtomaric expressions of ischemia. Am J Cardiol 59:23C–30C
Heyndrikx CR, Baic H, Nelkins P (1978) Depression of regional blood flow and wall thickening after brief coronary occlusion. Am J Physiol 234:653–660
Nagel E, Schneider U, Schall S, Ibrahim T, Schnackenburg B, Bornstedt A, Klein C, Lehmkuhl HB, Fleck E (2000) Magnetic resonance real time imaging for the evaluation of left ventricular function. J Cardiovasc Magn Reson 2:7–14
Schalla S, Klein C, Paetsch I, Lehmkuhl H, Bornstedt A, Schnackenburg B, Fleck E, Nagel E (2002) Real-time MR image acquisition during high-dose dobutamine hydrochloride stress for detecting left ventricular wall-motion abnormalities in patients with coronary artery disease. Radiology 224:845–851
Poldermans D, Fioretti PM, Boersma E, Bax JJ, Thomson IR, Roelandt JRTC, Simoons ML (1999) Long-term prognostic value of dobutamine-atropine stress echocardiography in 1737 patients with proven or suspected coronary artery disease. Circulation 99:757–762
Taillefer R, Ahlberg AW, Masood Y, White CM, Lamargese I, Mather JF, McGill CC, Heller GV (2003) Acute beta-blockade reduces the extent and severity of myocardial perfusion defects with Dipyridamole Tc-99m Sestamibi SPECT imaging. J Am Coll Cardiol 42:1475–1483
Miller RR, Olson HG, Amsterdam EA, Mason DT (1975) Propranolol withdrawal rebound phenomenon. Exacerbation of coronary events after abrupt cessation of antianginal therapy. N Engl J Med 293:416–418
Lindenfeld J, Crawford MH, O’Rourke RA, Levine SP, Montiel MM, Horwitz LD (1980) Adrenergic responsiveness after abrupt propranolol withdrawal in normal subjects and in patients with angina pectoris. Circulation 62:704–711
Myers MG, Wisenberg G (1977) Sudden withdrawal of propranolol in patients with angina pectoris. Chest 71:24–26
Kasser IS, Bruce RA (1969) Comparative effects of aging and coronary heart disease on submaximal and maximal exercise. Circulation 39:759–774
Blomqvist CG (1971) Use of exercise testing for diagnostic and functional evaluation of patients with arteriosclerotic heart disease. Circulation 44:1120–1136
Elhendy A, van Domburg RT, Bax JJ, Nierop PR, Geleijnse ML, Ibrahim MM, Roelandt JRTC (1999) The functional significance of chronotropic incompetence during dobutamine-stress test. Heart 81:398–403
Wintersperger BJ, Nikolaou K, Dietrich O, Rieber J, Nittka M, Reiser MF, Schoenberg SO (2003) Single breath-hold real-time cine MR imaging: improved temporal resolution using generalized autocalibrating partially parallel acquisition (GRAPPA) algorithm. Eur Radiol 13:1931–1936
Acknowledgment
We are indebted to Dr W.J. Post for data analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuijpers, D., Janssen, C.H.C., van Dijkman, P.R.M. et al. Dobutamine stress MRI. Part I. Safety and feasibility of dobutamine cardiovascular magnetic resonance in patients suspected of myocardial ischemia. Eur Radiol 14, 1823–1828 (2004). https://doi.org/10.1007/s00330-004-2425-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-004-2425-y



