Abstract
Although periodontal diseases during fixed appliance treatment are a common issue, few studies have focused on the clinical and microbial factors associated with orthodontic appliances. Hence, we investigated changes in the subgingival microbial community and their association with periodontal changes at the early stage of fixed appliance treatment. Subgingival plaques from ten female patients with fixed appliances were obtained at three time points: before, 1 month and 3 months after the placement of the brackets (T0, T1 and T2). The 16S rRNA gene sequencing was used to analyze the microbial community of the subgingival plaque. The Plaque Index (PI) and Gingival Bleeding Index (GBI) were also recorded. The GBI significantly increased at T2, and the PI showed a temporary increase without a significant difference. The alpha diversity indices were stable. However, the beta diversity was significantly higher at T2 compared to T0 and T1. The relative abundance of core microbiomes at the genus level was relatively stable. Four periodontal pathogens at the species level, including Prevotella intermedia (Pi), Campylobacer rectus (Cr), Fusobacterium nucleatum (Fn), and Treponema denticola (Td), increased without significant differences. The subgingival microbial community affected by fixed appliance treatment might cause transient mild gingival inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although most studies have suggested that permanent periodontal injuries rarely occur after orthodontic treatment, periodontal inflammation during orthodontic treatment, such as gingival hyperplasia and recession, is a common complication [8, 21]. The placement of the bracket and band promote plaque accumulation and influence plaque maturation [1, 14, 24]. In some cases, gingival inflammation, such as gingival bleeding and swelling, occurred in patients with poor oral hygiene [7]. Plaque is the primary etiological factor of gingival inflammation during orthodontic treatment [2, 20, 22]. In the presence of plaque, gingival inflammation can occur. Hence, long-term plaque control should be emphasized during orthodontic treatment. From the microbial viewpoint, periodontal inflammation is caused by microbial infection with periodontal pathogens in the subgingival biofilm. Previous studies have analyzed the frequency and prevalence of some putative periodontal pathogens to evaluate periodontal conditions [13, 14, 19, 27]. Yet shifts in the microbial community may play a more important role in the development of periodontal disease than changes in some specific pathogens [16]. The relationship between the microbial community and clinical periodontal changes during fixed appliance treatment remains unclear. Therefore, analyzing the microbial community would help to identify periodontal changes during fixed appliance treatment.
Traditional microbiological detection techniques, such as polymerase chain reaction (PCR) and culturing, do not reflect the whole microbial community. 16S rRNA gene sequencing is used to analyze the microbial community from a deeper view of structure and diversity [26]. 16S rRNA genes have been recognized as the most useful targets for microbial identification. However, only one study has used 16S rRNA gene sequencing to analyze changes in the microbial community during fixed appliance treatment [15]. It mainly focused on microbial changes in adolescent patients and did not take clinical periodontal changes into consideration.
Hence, more studies are needed to avoid periodontal complications for patients with fixed orthodontic appliances. In this preliminary investigation, we evaluated microbial changes and their association with clinical characteristic during the initial period of fixed appliance treatment.
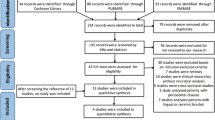
Materials and Methods
Sampling and Treatment
The Peking University Biomedical Ethics Committee (Beijing, China) (PKUSSIRB-2,012,063) approved the experimental protocol. Ten female patients were recruited from the orthodontic department of Peking University School and the Hospital of Stomatology to participate in our study. All patients were scheduled to have fixed appliance treatment and signed our written informed consent form.
Patients were included according to the following criteria: female, 18–40 years old, mild to moderate tooth crowding, no periodontitis (no periodontal attachment loss), good oral hygiene, no smoking, not pregnant and no intake of antibiotics or hormones 1 month before joining the study. Patients with missing first molars or first central incisors, or with crowns or fixed bridges, were excluded. All included patients had received subgingival ultrasonic scaling 1 month before the placement of the brackets. Then, Roth Shinye Brackets (Shinye, Hangzhou, China) were bonded using Transbond XT primer and adhesive paste (3M unitek, Monrovia, USA). Further oral health instructions were received by the participants. Periodontal treatment and mouthwash were not allowed within the first 3 months.
In our study, the first molars and central incisors were selected as the index teeth. The periodontal examination and subgingival plaque sample collection of the index teeth were obtained at three time points: before the placement of the brackets (T0), 1 month after the placement of brackets (T1) and 3 months after the placement of the brackets (T2). At each time point, all patients were required to refrain from brushing tooth and eating food for 2 h. The clinical examinations and sample collection were performed before any orthodontic treatment.
As for clinical investigation, we choose Gingival Bleeding Index (GBI) and plaque index (PI) as the clinical parameter. An experienced periodontist recorded them at each time point. The Quigley–Hein Plaque Index was selected to measure the presence of plaque. Gingival Bleeding Index was assessed by inserting a WHO probe horizontally into the interproximal papilla of each index tooth with a 20 g probing force [12]. The PI and GBI scores for each patient are presented as the mean ± SD.
After clinical examination and removal of supragingival plaque, subgingival plaque samples were collected immediately from the labial or buccal surfaces of index teeth with a sterilized periodontal curette. All samples were pooled together into a microcentrifuge tube that contained 1.0 mL of sterilized saline water and were stored immediately at − 80 °C.
DNA Isolation and 16S rRNA Gene Sequencing
DNA was isolated from subgingival plaque samples using a commercial bacterial DNA mini kit (Tiangen Biotechnologies, Beijing, China) as described by Guo et al. [9]. NanoDrop ND1000 spectrophotometer (NanoDrop Technologies, Inc.) was used to measure the quality and quantity of DNA. The v3–v4 hypervariable regions of the 16S rDNA were amplified using PCR. The libraries were pyrosequenced on an Illumina MiSeq Platform at the Biomarker Institute (Biomarker Institute, Beijing, China). The sequence data obtained in this study have been deposited in the NCBI Short Reads Archive database under Accession Number SRP114894.
Sequence Processing and Statistical Analyses
The sequences were analyzed using the Mothur software and the Quantitative Insights Into Microbial Ecology (QIIME) pipeline. After the raw sequences were trimmed and filtered, the remaining high-quality sequences were clustered into the operational taxonomic units (OTUs) at 97% similarity. With the program UCLUST, the Human Oral Microbiome Database and the SILVA 16S rRNA reference alignment were used to identify and taxonomically place the sequences [4, 23]. We evaluated the differences of microbial diversity (alpha diversity and beta diversity) at different time points with one-way analyses of variance (ANOVA). The statistical significance of differences in relative abundance among groups was determined following the Metastats method. P < 0.05 was accepted as statistically significant.
Results
OTU Analyses
We used Illumina sequencing to analyze 30 subgingival plaque samples from ten subjects at three time points. The mean age of all female patients included in the study was 23.3 ± 3.7 years (range 19–30 years) at the start of the fixed appliance treatment. A total of 2,211,137 raw reads were generated with an average of 73,705 ± 5776 (ranging from 61,997–80,087) reads per sample. After data were trimmed and filtered, 1,646,231 high-quality reads were obtained with an average of 54,874 ± 5268 (ranging from 42,399–61,266) sequences per sample. The average length of the high-quality reads was 441 ± 2.1 bp (ranging from 437 to 445 bp). With all reads clustering into OTUs at 97% similarity cutoff, 417 OTUs were ultimately detected, with an average of 272 ± 49 (ranging from 124 to 337) OTUs per sample.
Clinical Results
The clinical information of included patients are presented in Table 1. The PI showed a temporary increase after the placement of the fixed appliance, but the change was not statistically significant. The overall mean GBI at T2 was 1.3 ± 0.7, which was significantly higher than at T0.
Microbial Diversity
Alpha diversity is a measure of the microbial diversity within each group, while beta diversity is used to evaluate the variation in microbial community among groups. Four alpha diversity parameters were calculated and compared at three different time points. Both the microbial richness estimator (Chao 1 and ACE index values) and the microbial community diversity estimators (the Simpson and Shannon diversity indices) showed no significant differences (Fig. 1). The alpha diversities within each group were basically equivalent. The weighted UniFrac distance measurements were used to compare the microbial community structure at T0, T1, and T2. The variation in beta diversity across time points was significantly different. As shown in Fig. 2, the variation in the beta diversity at T2 was higher compared to that at T0 (P < 0.05) and T1 (P < 0.01), but there were no significant differences between T0 and T1.
Microbial Composition and Distribution
To further investigate the shift in the microbial community, the microbial composition and distribution at phyla, genera, and species levels were analyzed. Core microbiomes and periodontal pathogens, which are the important indicators of periodontal disease, were also investigated.
Cluster analyses detected 12 phyla. A heat map was used to illustrate changes in the microbial community profile at the phyla level (Fig. 3a). The microbial distribution of the top 10 phyla is illustrated in Fig. 3b. The predominant phyla were Firmicutes, Bacteroidetes, Actinobacteri, Proteobacteria, and Fusobacteria. Firmicutes was the most dominant phylum, representing 24.2% of all sequence reads at T0; it was less abundant at T1 (20.80%) and T2 (19.66%), but the differences were not statistically significant. The relative abundances of Fusobacteria and candidate division TM7 were slightly higher at T1 and T2 than at T0, but there were no statistically significant differences.
Cluster analyses detected 105 genera, and the top ten are shown in Fig. 4. The relative abundance was relatively stable during the first 3 months of fixed appliance treatment, although a significant change in microbial composition was found. The five most abundant genera at T0 were Streptococcus (12.89%), Prevotella (9.94%), Fusobacterium (7.29%), Corynebacterium (6.90%), and Actinomyces (6.72%). In addition, Metastats analyses indicated that the abundances of three genera significantly differed at different time points. The relative abundances of Actinobacillus and Capnocytophaga were significantly higher at T1 than at T0 (P < 0.05), and decreased at T2 (Fig. 5). Both of these two genera showed a temporary increase. Granulicatella showed a significantly reduced abundance between T0 and T2 (P < 0.05). Core genera were defined as those that were commonly shared and detected (relative abundance > 1.0%) among groups. The changes in the relative abundance of 20 core genera are illustrated in Fig. 6. In addition to core genera, the relative abundances of eight putative periodontal genera were analyzed and found no significant differences during the first 3 months of fixed appliance treatment (Fig. 7). These data imply that both the core genera and putative periodontal genera were relatively stable.
Relative abundances of microbiota that showed statistically significant differences among three different time points. According to Metastats analyses, the relative abundances of the genera Actinobacillus and Capnocytophaga were significantly higher at T1 than at T0, and those of Granulicatella and the species Streptococcus tigurinus were significantly higher at T0 compared to T1. All data are expressed as the mean ± standard deviation. P < 0.05 in ANOVA
Considering the limitation of sequencing v3–v4 hypervariable regions of the 16S rDNA, only four periodontal pathogens were detected and analyzed at the species level in our study (Fig. 7). The relative abundance of Prevella intermedia (Pi) and Campylobacer rectus (Cr) showed a temporary increase at T1, and returned to the pretreatment level at T2. Slight increases in the relative abundances of Fusobacterium nucleatum (Fn) and Treponema denticola (Td) were found at T2 compared to that at T0 and T1. Changes in the relative abundances of the four periodontal pathogens were not statistically significant. According to Metastats analyses, Streptococcus tigurinus was the only species that significantly changed and it decreased at T2 compared to T0 (P < 0.05). These data might indicate that there was a temporary increase in the relative abundance of periodontal pathogens at the species level.
Discussion
The periodontium damage is a major concern during fixed appliance treatment. There are many factors, such as the presence of brackets, hormonal characteristics, and patient compliance, that affect periodontal health and the microbial community during orthodontic treatment [18]. The effects of the bracket on periodontal health were emphasized in our study. To enhance the compliance of patients, standardized oral hygiene instructions were repeated at every visit to ensure the patients maintained proper oral hygiene.
In previous studies that have evaluated periodontal status, traditional microbial culture and PCR have been used to analyze changes in the abundances of several periodontal pathogens following the fixed appliance treatment [8]. Some studies that have used 16S rDNA gene sequencing have found that periodontal diseases mainly occur due to an obvious shift in the microbial community rather than changes in individual periodontal pathogens [17]. Yet changes in the microbial community during orthodontic treatment have rarely been studied [16, 29]. One recent prospective study reported changes in the microbial community during orthodontic treatment in terms of microbial composition, but this change was not associated with clinical parameters and the patients included in the study were adolescents [15]. Because the hormonal changes during puberty could affect the periodontal status and subgingival microorganisms, our study focused on changes in the subgingival microbial community and their association with clinical parameters in female adults.
We observed a transient increase in PI and an increase in GBI at T2 (1.3 ± 0.7), indicating that mild gingivitis had occurred 3 months after the brackets were placed. The transient increase in PI might be a result of patient unfamiliarity with the maintenance of oral hygiene with brackets. Once they properly maintained oral hygiene, the PI would return to the normal level. The significant increase in GBI at T2 might be due to the lag effects of the gingival reaction to the accumulated plaque at T1. With strict plaque control, the GBI would return to the normal level.
Analyses of microbial diversity, consisting of alpha and beta diversity, were used to evaluate the stability and health status of the microbial community. More diverse communities are dominated by more microorganisms and thus are healthier and more stable [3]. In our study, the intergroup variability in alpha diversity was relatively stable. However, the beta diversity was significantly higher at T2 than at T0 and T1, which indicates that the structure and composition of the microbial community significantly changed at T2. In addition, these results were supported by changes in the microbial distribution and heat map results. Taken together, these results indicate that the microbial community was affected by orthodontic appliance.
Microorganisms of three genera, Actinobacillus, Capnocytophaga and Granulicatella, and one species, Streptococcus tigurinus, significantly changed between time points. Capnocytophaga and Granulicatella have both been reported as potential periodontal pathogens [10]. The changes in these two pathogens were different: Capnocytophaga showed a transient increase and Granulicatella showed a significant decrease at T2. S. tigurinus was recently reported to be a novel pathogen causing infective endocarditis and meningitis, and its role in periodontal disease has been studied [5, 28]. Dhotre et al. isolated Streptococcus tigurinus from patients with periodontitis and speculated that it might play a role in the disease process [5]. On the contrary, Zbinden et al. recorded S. tigurinus at a high prevalence in microbial flora, but reported that its occurrence did not increase in patients with periodontitis [28]. In our study, the relative abundance of S. tigurinus decreased during fixed appliance treatment. Further research is required to identify its role in periodontal disease.
Core microbiomes have been reported to play key roles in periodontal disease [6]. In general, core microbiomes are defined as the most common and shared inhabitants of the gingival sulcus that could influence the microbial community. In this study, 20 genera whose relative abundances were more than 1% and were shared among groups were selected as the core microbiomes. Among these, the relative abundances of most genera were stable. Besides that, the increased genus Actinomyces and stable genus Veillonella during the fixed appliance treatment were found in our study, which in accordance with Koopman et al. [15]. Both of these two core microbiomes were associated with periodontal status. However, their roles in periodontal inflammation should be determined on the species level, not the genus level, which is a limitation of our research. Koopman et al. and Huang et al. reported that Candidate division TM7, another core microbiome found in our study, might play a role in gingivitis [11, 15]. In our study, its relative abundance during the first 3 months of fixed appliance treatment tended to increase without a significant difference. The relatively stable core microbiomes might represent a relatively healthy periodontal status.
We further investigated the acknowledged periodontal pathogens at the genus and species level. Eight genera were analyzed and there were no significant changes in any of them. Although it is more precise to evaluate the role of periodontal pathogens in periodontal inflammation at the species level, only a limited number of species could be discriminated in consideration of the limited information obtained from the V3–V4 hypervariable regions of 16S rDNA. Hence, only four periodontal pathogens at the species level, including Pi, Cr, Fn, and Td, were identified. Pi, which was associated with periodontal disease, has been reported to increase during fixed appliance treatment [25]. In our study, Pi and Cr transiently increased at T1, and returned to the pretreatment level at T2, whereas Fn and Td showed an increasing trend during the first 3 months of fixed appliance treatment. Although the changes in the relative abundance of these four periodontal pathogens were not statistically significant, these increasing trends might suggest a risk for mild periodontal inflammation.
Although the alpha diversity and core microbiomes were relatively stable, we still observed changes in the relative abundance of a few microorganisms, including increases in periodontal pathogens. In addition, the fixed appliance induced significant changes to the structure and composition of the microbial community. In general, the microbial changes confirmed the results of the periodontal changes which contribute to a tendency toward mild gingival inflammation. We speculate that the fixed appliance might have caused a transient mild gingival inflammation in the early stages of treatment. However, the lack of long-term observations and the small sample size are the limitations of our study.
Conclusions
Our study provides a preliminary investigation of the changes in the subgingival microbial community and its association with periodontal change during the first 3-month fixed appliance treatment. The results of our study suggest that fixed appliance treatment may lead to a transient change of the subgingival microbial community, which might cause transient mild gingival inflammation. However, a long-term study with a large sample size is required to verify our findings.
References
Atack NE, Sandy JR, Addy M (1996) Periodontal and microbiological changes associated with the placement of orthodontic appliances. A review. J Periodontol 67:78–85
Boke F, Gazioglu C, Akkaya S, Akkaya M (2014) Relationship between orthodontic treatment and gingival health: a retrospective study. Eur J Dent 8:373–380
Camelo-Castillo A, Novoa L, Balsa-Castro C, Blanco J, Mira A, Tomas I (2015) Relationship between periodontitis-associated subgingival microbiota and clinical inflammation by 16S pyrosequencing. J Clin Periodontol 42:1074–1082
Dewhirst FE, Chen T, Izard J, Paster BJ, Tanner AC, Yu WH et al (2010) The human oral microbiome. J Bacteriol 192:5002–5017
Dhotre SV, Mehetre GT, Dharne MS, Suryawanshi NM, Nagoba BS (2014) Isolation of Streptococcus tigurinus—a novel member of Streptococcus mitis group from a case of periodontitis. FEMS Microbiol Let 357:131–135
Duran-Pinedo AE, Chen T, Teles R, Starr JR, Wang X, Krishnan K et al (2014) Community-wide transcriptome of the oral microbiome in subjects with and without periodontitis. ISME J 8:1659–1672
Guo L, Feng Y, Guo HG, Liu BW, Zhang Y (2016) Consequences of orthodontic treatment in malocclusion patients: clinical and microbial effects in adults and children. BMC Oral Health 16:112
Guo R, Lin Y, Zheng Y, Li W (2017) The microbial changes in subgingival plaques of orthodontic patients: a systematic review and meta-analysis of clinical trials. BMC Oral Health 17:90
Guo R, Zheng Y, Liu H, Li X, Jia L, Li W (2018) Profiling of subgingival plaque biofilm microbiota in female adult patients with clear aligners: a three-month prospective study. Peer J 6:e4207
Holdeman LV, Moore WE, Cato EP, Burmeister JA, Palcanis KG, Ranney RR (1985) Distribution of capnocytophaga in periodontal microfloras. J Periodontal Res 20:475–483
Huang S, Yang F, Zeng X, Chen J, Li R, Wen T et al (2011) Preliminary characterization of the oral microbiota of Chinese adults with and without gingivitis. BMC Oral Health 11:33
Kilian M, Chapple IL, Hannig M, Marsh PD, Meuric V, Pedersen AM et al (2016) The oral microbiome—an update for oral healthcare professionals. Br Dental J 221:657–666
Kim K, Jung WS, Cho S, Ahn SJ (2016) Changes in salivary periodontal pathogens after orthodontic treatment: an in vivo prospective study. Angle Orthod 86:998–1003
Kim SH, Choi DS, Jang I, Cha BK, Jost-Brinkmann PG, Song JS (2012) Microbiologic changes in subgingival plaque before and during the early period of orthodontic treatment. Angle Orthod 82:254–260
Koopman JE, van der Kaaij NC, Buijs MJ, Elyassi Y, van der Veen MH, Crielaard W et al (2015) The effect of fixed orthodontic appliances and fluoride mouthwash on the oral microbiome of adolescents—a randomized controlled clinical trial. PLoS ONE 10:e0137318
Kumar PS, Leys EJ, Bryk JM, Martinez FJ, Moeschberger ML, Griffen AL (2006) Changes in periodontal health status are associated with bacterial community shifts as assessed by quantitative 16S cloning and sequencing. J Clin Microbiol 44:3665–3673
Li Y, He J, He Z, Zhou Y, Yuan M, Xu X et al (2014) Phylogenetic and functional gene structure shifts of the oral microbiomes in periodontitis patients. ISME J 8:1879–1891
Mombelli A, Lang NP, Burgin WB, Gusberti FA (1990) Microbial changes associated with the development of puberty gingivitis. J Periodontal Res 25:331–338
Naranjo AA, Trivino ML, Jaramillo A, Betancourth M, Botero JE (2006) Changes in the subgingival microbiota and periodontal parameters before and 3 months after bracket placement. Am J Orthod Dentofac Orthop 130:275
Ong MM, Wang HL (2002) Periodontic and orthodontic treatment in adults. Am J Orthod Dentofac Orthop 122:420–428
Petti S, Barbato E, Simonetti D’Arca A (1997) Effect of orthodontic therapy with fixed and removable appliances on oral microbiota: a six-month longitudinal study. New Microbiol 20:55–62
Pinto AS, Alves LS, Zenkner J, Zanatta FB, Maltz M (2017) Gingival enlargement in orthodontic patients: effect of treatment duration. Am J Orthod Dentofac Orthop 152:477–482
Pruesse E, Quast C, Knittel K, Fuchs BM, Ludwig W, Peplies J et al (2007) SILVA: a comprehensive online resource for quality checked and aligned ribosomal RNA sequence data compatible with ARB. Nucleic Acids Res 35:7188–7196
Ren Y, Jongsma MA, Mei L, van der Mei HC, Busscher HJ (2014) Orthodontic treatment with fixed appliances and biofilm formation—a potential public health threat? Clin Oral Invest 18:1711–1718
Ristic M, Vlahovic Svabic M, Sasic M, Zelic O (2008) Effects of fixed orthodontic appliances on subgingival microflora. Int J Dent Hyg 6:129–136
Sturgeon A, Stull JW, Costa MC, Weese JS (2013) Metagenomic analysis of the canine oral cavity as revealed by high-throughput pyrosequencing of the 16S rRNA gene. Vet Microbiol 162:891–898
Thornberg MJ, Riolo CS, Bayirli B, Riolo ML, Van Tubergen EA, Kulbersh R (2009) Periodontal pathogen levels in adolescents before, during, and after fixed orthodontic appliance therapy. Am J Orthod Dentofac Orthop 135:95–98
Zbinden A, Aras F, Zbinden R, Mouttet F, Schmidlin PR, Bloemberg GV et al (2014) Frequent detection of Streptococcus tigurinus in the human oral microbial flora by a specific 16S rRNA gene real-time TaqMan PCR. BMC Microbiol 14:231
Zijnge V, Ammann T, Thurnheer T, Gmur R (2012) Subgingival biofilm structure. Front Oral Biol 15:1–16
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Rights and permissions
About this article
Cite this article
Guo, R., Liu, H., Li, X. et al. Subgingival Microbial Changes During the First 3 Months of Fixed Appliance Treatment in Female Adult Patients. Curr Microbiol 76, 213–221 (2019). https://doi.org/10.1007/s00284-018-1610-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-018-1610-1