Abstract
Purpose
High-dose methotrexate (HD-MTX) is widely used in pediatric and adult oncology treatment regimens. This study aimed to develop a population pharmacokinetic model to characterize pediatric and adult MTX exposure across various disease types and dosing regimens, and to evaluate exposure–toxicity relationships.
Methods
MTX pharmacokinetic data from pediatric and adult patients were collected. A population pharmacokinetic model was developed to determine the effects of age, liver function, renal function, and demographics on MTX disposition. The final model was used in Monte Carlo simulations to generate expected exposures for different dosing regimens. The association of toxicity, determined through chart review, and MTX area under the curve (AUC) was modeled using logistic regression.
Results
The analysis included 5116 MTX concentrations from 320 patients (135 adult, age 19–79 years; 185 pediatric, age 0.6–19 years). Estimated glomerular filtration rate (eGFR) and treatment cycle number were independent predictors of clearance (CL). CL varied 2.1-fold over the range of study eGFR values and increased 14% for treatment cycle numbers greater than 7. Higher MTX AUC was associated with higher risk of nephrotoxicity in adults, and neurotoxicity and hepatotoxicity in pediatrics.
Conclusions
This study represents one of the most comprehensive evaluations of HD-MTX PK across a wide range of ages and disease types. After accounting for differences in renal function, age did not impact CL, although toxicity patterns differed by age. The model allows for early identification of patients with slowed MTX clearance and at higher risk of toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Methotrexate (MTX) is a folate antimetabolite that inhibits DNA synthesis, repair, and cellular replication [1]. High-dose methotrexate (HD-MTX) is defined as a dosage higher than 500 mg/m2 and has a broad range of antitumor activity. It is an essential component of lymphoma, osteosarcoma, and acute lymphoblastic leukemia (ALL) therapy [2]. However, HD-MTX can cause significant toxicities including acute kidney injury, myelosuppression, mucositis, neurotoxicity, and hepatotoxicity, which can lead to significant morbidity and treatment delays [3]. Supportive care including aggressive intravenous hydration, urine alkalinization, rescue with leucovorin administration, and serial measurements of serum methotrexate, serum creatinine (SCR), and urine output is crucial for preventing toxicity [4, 5].
MTX drug levels can vary widely between patients even after accounting for renal function, subject size and other factors [6]. There is a nomogram published in 1983 that only covers a single dosing regimen for expected time-dependent decrease in MTX levels, with higher levels indicating an increased risk of toxicity [7]. The nomogram represents clinical data from nine patients, aged 9–26 years. Many treatment protocols reference this nomogram in serial monitoring of MTX levels to dictate the degree of supportive care needed following HD-MTX administration. The generalizability of the nomogram, however, is limited due to small sample size, narrow age range, and inclusion of only a single MTX dosage, whereas current methotrexate dosing regimens are used across a broad age range. While subsequent population PK models have been developed for HD-MTX, they have similar limitations in sample size, age range, and dosage range. The exact relationship between MTX levels and toxicity across various treatment regimens and patient populations also remains unclear. Additional information on the effects of age, renal function, and baseline demographics on MTX PK would be beneficial for assessing MTX dosing and toxicity.
Despite protocols for aggressive intravenous fluid hydration and urine alkalinization during HD-MTX therapy, renal dysfunction develops in 2–12% of patients [8]. Renal toxicity leads to impaired MTX clearance and prolonged exposure to toxic concentrations, which can further worsen renal function and non-renal adverse events. Toxic levels of MTX can be rapidly and effectively decreased by intravenous administration of glucarpidase, an enzyme that cleaves MTX into nontoxic metabolites, but the cost of a single dose can range from $100,000 to $200,000 [9, 10]. The dosing of glucarpidase is based on expected MTX exposure for a given MTX dose; however, information on expected MTX exposures is limited [11]. A robust population PK model with Monte Carlo simulations of various dosing regimens and patient populations can generate the expected range of MTX concentrations throughout therapy in diverse settings and can assist in predicting patients at highest risk for severe toxicity.
The current study aimed to develop a broadly applicable population PK model for HD-MTX from childhood into the adult years, and to examine the association between MTX exposure and toxicity. The final population PK model was used in simulations to help generate an updated profile of expected exposures for different MTX dosing regimens and age groups.
Materials and methods
Patient population
The MTX dataset represented all adult and pediatric oncology patients treated with intravenous HD-MTX with MTX dosing information and concentrations measured as part of standard of care oncology treatment from Jan 1, 2009 through Jan 1, 2017 at the University of California, San Diego Health and Rady Children’s Hospital San Diego (RCHSD). HD-MTX was defined as a dose greater than or equal to 500 mg/m2. The protocol was approved by the University of California San Diego Institutional Review Board. Because this was a retrospective chart review, informed consent was not feasible and this requirement was waived.
Electronic extraction and chart review
MTX doses, MTX concentrations, laboratory values (SCR, ALT, total bilirubin), and demographics (age, weight, height, gender, disease type) were electronically extracted from electronic medical records (EMR) at the University of California, San Diego Health and RCHSD. For MTX assays, the ARK method was used in the CAPS/CLIA certified laboratory of both institutions. At the University of California, San Diego Health, the precision ranged from 11.1 to 12.5% across MTX concentrations from 0.07 to 0.80 µM, and at RCHSD the precision ranged from 3.4 to 13% across MTX concentrations from 0.07 to 50 µM. Prior to 2017, the RCHSD laboratory used the FPIA method with a precision of ≤ 10%. Toxicity data were collected by manual chart review of the EMR. All patient notes were reviewed from the date of first intravenous HD-MTX administration to 3 months after the final MTX administration to evaluate for the occurrence of nephrotoxicity, mucositis, neurotoxicity, myelosuppression, and hepatotoxicity. Only toxicities diagnosed and documented by the patient’s physician in chart notes as clearly attributable to HD-MTX were included for the analysis. The dataset was assembled using the statistical software R (version 3.4.1).
Pharmacokinetic analysis
Population PK modeling was completed with NONMEM (v. 7.3). The first-order conditional estimation method with interaction (FOCEI) was used. A two-compartment PK structural model (ADVAN3, TRANS4 subroutine) with linear elimination was used to describe the data. An exponential-normal distribution error model was used for between-subject variability.
Potential covariates were evaluated in a forward selection approach, with covariates that resulted in a reduction in the objective function value (OFV) of greater than 4 (p < ~ 0.05) being retained in the multivariate assessment. The multivariate assessment utilized a forward selection approach where covariates found to reduce the OFV by greater than 8 (p < ~ 0.005) were retained in the final model. PK parameters were scaled by subject size before evaluation of other potential covariates. An allometric approach was used with CL and Q scaled by allometric weight [(WT/70)0.75] and volume of distribution scaled by weight [(WT/70)1.0]. SCR, age, estimated glomerular filtration rate (eGFR), liver function (ALT, total bilirubin), disease type, treatment cycle number, and male gender were evaluated as potential covariates for CL, V1, and V2. SCR and eGFR were evaluated as time-varying covariates while the baseline values per cycle for other covariates were used. eGFR for adults was calculated using Cockcroft–Gault and normalized to a BSA of 1.73 m2 [12]. Pediatric eGFR was estimated using the Bedside Schwartz equation [13]. Time-varying SCR values were used in the eGFR calculations.
Empiric Bayesian estimates of the individual pharmacokinetic parameters were generated from the final model using the POSTHOC routine. A 1000-sample bootstrap assessment of the final model was performed using Wings for NONMEM (v. 7.4.1).
Exposure–toxicity analysis
Logistic regression (SAS v. 9.4) was used to determine the relationship between HD-MTX cycle 1 exposure and occurrence of toxicity. HD-MTX area under the curve (AUC) was calculated from individual Bayesian estimates from the final population PK model as MTX dosage divided by clearance. p values less than or equal to 0.05 were considered significant.
Monte Carlo simulations
Monte Carlo simulations were performed using the final population PK model to compare differences in HD-MTX elimination between different age groups, disease types, and baseline renal function. Concentration profiles were generated for four age groups (0–5 years, 6–11 years, 12–16 years, and adults), and three disease types (ALL, lymphoma, osteosarcoma) with each age group-disease type combination represented by 1000 virtual subjects each (12,000 total). The adult age group was represented by subjects aged 20–60 years. Each subject was assigned the median eGFR values for each age group with a 25% variance applied in NONMEM. Uniform height and weight distributions for pediatric patients in the simulations were derived from CDC 50th percentile weights. All adults were assigned a height of 170 cm, and a uniform weight distribution was derived from summary statistics of the study population. Standard MTX dosages for adult and pediatric ALL, lymphoma, and osteosarcoma were used and were as follows:
ALL (pediatric): 500 mg/m2 over 0.5 h, then 4500 mg/m2 over 23.5 h (total 5000 mg/m2 over 24 h).
ALL (adult): 200 mg/m2 over 2 h, then 800 mg/m2 over 22 h (total 1000 mg/m2 over 24 h).
Lymphoma: 3000 mg/m2 over 3 h.
Osteosarcoma: 12,000 mg/m2 over 4 h.
Expected exposures for HD-MTX were generated using the median and 95% range of concentrations from the simulations for each unique combination of age group and disease type.
Results
Patients
The study population included 320 patients (135 adult, 185 pediatric). The majority of patients received multiple cycles of HD-MTX therapy and had multiple MTX concentrations measured in each cycle. The median number of MTX cycles per patient was 4, and the median number of MTX concentrations per cycle was 4. In the study, 18% of patients had only one cycle, and 3% of cycles had only one sample. Table 1 summarizes patient characteristics at first cycle of HD-MTX therapy. MTX concentrations for adults are shown in Fig. 1a and pediatric patients are in Fig. 1b. Of the total 5116 samples, 282 samples (5.5%) were drawn during the MTX infusion. MTX dosage ranged from 734 to 12,312 mg/m2.
Summary of high-dose methotrexate concentrations separated by a adult and b pediatric data. Solid black line represents median concentrations. Dotted black lines represent 95% range of concentrations. The wide range of concentrations represents different dosing regimens and infusion times included in the study. Horizontal grey line represents a methotrexate level of 0.1 µM. Time after dose is the time (h) after the beginning of the first infusion in a treatment cycle. Higher MTX concentrations are observed in pediatric patients compared to adult patients due to the use of higher MTX dosages in this population
Population pharmacokinetic analysis
A two-compartment structural model described the data well. Attempts to simplify the model to one compartment resulted in a poor fit to the data. After allometric scaling for weight, the following were significant covariates in the univariate screen: CL: eGFR, SCR, ALT, age, treatment cycle number; V1: age, osteosarcoma, eGFR, ALT; V2: ALT, total bilirubin, age, osteosarcoma. While eGFR and SCR were both identified as potential covariates in the univariate screen, eGFR was retained in the multivariate screen as it resulted in a more dramatic decrease in the OFV and better accounts for changes in renal function across the broad age spectrum of the study. Age was also no longer a significant covariate for clearance, once renal function was accounted for in a robust manner with eGFR. For treatment cycle number, a cut-off of greater than 7 cycles was used based on visual inspection of differences in CL ETA distributions across treatment cycles. After multivariate screening, significant covariates retained in the final model were eGFR and treatment cycle number on CL, age and ALT on V1, and ALT and osteosarcoma on V2. The covariates were not correlated. The strongest correlation was eGFR and age at R2 of 0.45, but age was part of the eGFR calculation. The next strongest correlation was total bilirubin and age at R2 of 0.17. Between-subject variability after inclusion of significant covariates on CL, V1, and V2 ranged from 37.3 to 57.4%. Inter-occasion variability (IOV) assessed on CL was 23.8%. The residual variability was best described by a combined proportional and additive error model.
eGFR modeled as a linear function of CL had the largest effect on CL. After eGFR was included as a covariate in the multivariate screen, age was no longer a significant covariate on CL. CL varied 2.1-fold over the range of eGFR values seen in the study, and CL increased by 14% for treatment cycle numbers greater than 7 (see Table 2, equations). After accounting for renal function, variability on CL was 37.3%.
The final population pharmacokinetic model described the data without significant bias as shown in Fig. 2a, b. The model fit the data well other than for samples drawn during infusion, the majority of which came from a single protocol. Shrinkage estimates for between-subject variability were 12.7% (V1), 5.6% (CL), and 33.9% (V2). Final model parameter and variance estimates are shown in Table 2. Bootstrap evaluation of the final model successfully converged with significant digits greater than or equal to 3.0 for 67% of the runs, and with significant digits greater than or equal to 2.0 for 79% of the runs. Parameter estimates for the two significant digit cut-offs were almost identical. Estimation results are summarized in Table 2. The median bootstrap parameter estimates were nearly identical to the final model. The 95% confidence intervals were reasonably tight for all parameters and the primary CL covariate of eGFR.
Population pharmacokinetic final model. a Plasma methotrexate concentrations from the study are compared with individual predictions for methotrexate levels. The dotted line represents the line of unity and demonstrates that the model describes the data without bias. The regression line is represented by the solid line. b The distribution of conditional weighted residuals (CWRES) over time from the final model is plotted and shows that the model describes the data with minimal bias over time. An early elevation in CWRES is seen due to the limited availability of early time points and collection during drug infusion
Exposure–toxicity analysis
Table 3 summarizes the toxicities seen in the study. A total of 230 toxicities were reported in the study population. A larger percentage of pediatric patients had reported toxicities than adults (74% vs. 64%). Hepatotoxicity (43%) was the most common toxicity in adult patients, and mucositis (67%) was the most common toxicity in pediatric patients. Myelosuppression was inconsistently documented for pediatric patients and was not included in the analysis.
Logistic regression results are summarized in Table 3. Odds ratios represent differences in risk for each 1000 µg × h/mL increase in AUC. MTX exposure was associated with an increased risk of nephrotoxicity (OR 7.1, p = 0.0004) in adult patients, and with an increased risk of neurotoxicity (OR 2.7, p = 0.01) and hepatotoxicity (OR 2.5, p = 0.001) in pediatric patients.
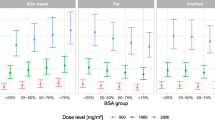
Monte Carlo simulations
Monte Carlo simulations demonstrate decreasing CL with decreased eGFR, with only a minor additional age effect (Fig. 3a). When eGFR decreased from 91–120 to 60–90 mL/min/1.73 m2 median CL values showed a decrease of 11.1–25.5% that varied by age group. Median and 2.5–97.5 percentile MTX concentrations for four age groups (0–5 years, 6–11 years, 12–16 years, and adults) and three disease types (ALL, lymphoma, osteosarcoma) are presented in Supplemental Fig. 1. Supplemental Fig. 2 represents the percentage of subjects from the simulation that have achieved a MTX value of less than 0.1 µM at each time interval. Figure 3b is the expected exposure percentile profile for a typical pediatric patient receiving an ALL regimen.
Monte Carlo simulation performed using the final model. a Median clearance (CL) with interquartile range (IQR) is plotted against estimated glomerular filtration rate (eGFR). Results are separated by age group (0–5 years, 6–11 years, 12–16 years, adults). The adult age group is represented in the simulations as patients age 20–60 years. Once differences in eGFR are accounted for, there is little difference between age groups in CL. b Expected exposure for methotrexate with Monte Carlo simulation using the final pharmacokinetic model following the most common pediatric methotrexate treatment regimen. Simulated standard dose for acute lymphoblastic leukemia. The solid line represents the median line, and the shaded area between the dotted lines represents the 95% range of the concentrations. The horizontal grey line represents a methotrexate level of 0.01 µM. Patients have estimated glomerular filtration rate (eGFR, mL/min/1.73 m2) greater than or equal to 60
Discussion
The current study represents one of the most comprehensive evaluations of HD-MTX PK to date representing a wide range of ages and disease types. HD-MTX population PK were well characterized by a two-compartment model. eGFR and cycle number were independent predictors of MTX clearance. eGFR was a better predictor of clearance than serum creatinine and the time-varying eGFR was a better predictor of clearance than baseline eGFR given the changes in renal function with therapy. The final model was used in simulations to generate expected exposures for different methotrexate dosing regimens and age groups given their differing renal functions. In simulations, clearance decreased with worsening renal function and placed patients at higher risk of toxicities. The cycle 1 AUC was found to relate to increased risk of neurotoxicity and hepatotoxicity in pediatric patients, and nephrotoxicity in adult patients.
There have been multiple prior population pharmacokinetic studies of HD-MTX. These 18 studies are summarized in Supplemental Table 1. The majority of prior studies were focused on pediatric ALL and osteosarcoma. The current study included all patients at UCSD and Rady Children’s Hospital receiving high-dose methotrexate thus includes ALL, lymphoma, and osteosarcoma in both pediatric and adult patients. Given the wide range of dosages administered in these cancer types, the pediatric population received MTX dosages between 935 and 12,312 mg/m2, and the adult population received dosages between 734 and 11,918 mg/m2. This provides a broader applicability for our model to all cancer patients receiving HD-MTX. The CL estimate for the current study is 0.25 L/h/kg for a typical patient in our population (56.7 kg). This is consistent with the published range of 0.10–0.42 L/h/kg from previous HD-MTX population PK models.
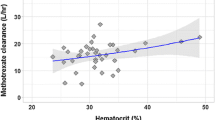
Renal function has been found to be an independent predictor of clearance in several prior studies. Baseline serum creatinine was found to be significant in 4 studies [14,15,16,17,18], while baseline eGFR was found to be significant in 3 studies [19,20,21]. A separate study used a time-varying serum creatinine as a model for MTX clearance. The current study used eGFR calculated using a time-varying serum creatinine. We found this better predicted CL than a baseline eGFR or serum creatinine. Because the body’s endogenous creatinine production differs in adult and pediatric populations, serum creatinine alone, relative to eGFR, is a weak biomarker for renal function. eGFR is normalized to BSA and better accounts for age and size-related differences in renal function. Treatment cycle number was tested due to the potential effect of repeated MTX exposure on CL. It was also found by Zhang et al. to have an effect on CL [14]. In both the current model and the model by Zhang et al., CL appears to increase with increasing MTX cycle number. This finding may be due to patients with higher MTX CL being able to tolerate more cycles of MTX therapy, with the resultant exclusion of patients with lower MTX CL from the later cycles. Prior studies also found that BSA [18], AST [17], ALT [20], hematocrit [22], hemoglobin [17] have an impact on MTX clearance. While ALT in the current study did not significantly impact CL, it did significantly impact V1 and V2. Elevated ALT is an indicator of liver dysfunction, which may lead to decreased albumin production. MTX binds to proteins in plasma and tissue, and therefore alterations in liver function tests may affect methotrexate binding and affinity in plasma and tissue. Hemoglobin and hematocrit values were not routinely available for all patients, so we did not test these variables in the model.
The incidence of methotrexate toxicity in the literature varies widely, with reported incidence ranging from 26 to 90% [23, 24]. A total of 64% of adult and 74% of pediatric patients in the current study had documented toxicities. We included all adverse events attributed to MTX reported in physician notes, while many other studies limited toxicity to higher grade toxicity which may account for the higher incidence seen in the current study. It is unclear if the higher incidence in pediatric than adult patients is a true difference or reflects documentation practices of physicians. Myelosuppression was notably excluded in the pediatric patients as a toxicity because the etiology was not clearly documented as attributable to MTX in physician notes. In adults, hepatotoxicity (43%) was the most common toxicity. This incidence is consistent with the range of 33–67% reported in literature for hepatotoxicity [24,25,26,27]. In pediatrics, mucositis (67%) was the most common toxicity, and is slightly higher than the range of 33–52% reported in literature, but these studies only included ALL and lymphoma patients [24,25,26,27].
The nomogram published by Abelson et al. suggests an increased risk of toxicity with higher MTX concentrations [7]. Studies have correlated MTX exposure with toxicities including neurotoxicity [28], hepatotoxicity [29, 30], mucositis [16], myelosuppression [17, 30], and nephrotoxicity [17]. We examined cycle 1 AUC to allow for early identification of patients at risk for toxicity in later cycles. AUC was found to be significantly correlated with nephrotoxicity in adults and with neurotoxicity and hepatotoxicity in pediatrics. No significant differences were found for mucositis or myelosuppression. Of the toxicities, prevention of nephrotoxicity and neurotoxicity are of particular clinical interest for early identification because nephrotoxicity may increase the risk for worsening renal function and non-renal adverse events, and neurotoxicity may manifest as seizures and leukoencephalopathy. The study by Comandone et al., which observed a correlation between nephrotoxicity and MTX exposure in adult osteosarcoma patients, included only grade 4 renal toxicity in the analysis. Bhojwani et al. observed a correlation between neurotoxicity and MTX exposure in pediatric ALL patients, and included leukoencephalopathy confirmed using brain MRIs. Despite differences in definition of adverse events between the current study and published studies, the current results are consistent with prior studies: nephrotoxicity is correlated with MTX exposure in the adult population, and neurotoxicity is correlated with MTX exposure in the pediatric population.
There are several limitations to the current study. Due to opportunistic utilization of clinical MTX concentration measurements, many patients were lacking full profiles and we had limited early time points. Many of the early time points came from pediatric data thus the estimation of the central volume of distribution is driven largely by pediatric data. In addition, a proportion of early concentrations were measured during MTX infusion. The difficulty of collecting accurate samples during drug infusion may contribute to the underprediction of early MTX concentrations by the final model. While we had osteosarcoma patients in the study, they were underrepresented compared to other disease types. The use of eGFR as an indicator of renal function in the current studies accounts for the filtration component of renal elimination, but not the renal excretion. While ALT and total bilirubin were included in covariate analysis, AST and alkaline phosphatase were not included. It is important to note the subjective nature of MTX toxicity reports in the current study that make the results susceptible to differences in physician judgment and documentation of toxicities. Due to the retrospective nature of this study, we were not able to form an adjudication panel to determine the validity of toxicity attribution.
While the retrospective design limited the exposure–toxicity analysis, the criteria of a physician chart note with an explicit statement of toxicity and causality, in addition to changes in laboratory values or symptoms, allowed for the exclusion of toxicities that may be caused by concomitant medications. This stringent requirement ensured that toxicities included in the study were clinically relevant and attributable to MTX therapy. In the toxicity analysis, while calculating AUC for the first cycle only had the potential to yield a weaker correlation, this approach was used to allow for prediction of toxicity. In addition, compared to published studies, different neurotoxicity endpoints and MTX parameters were used in our toxicity analysis, making a direct comparison between odds ratios of the current study and other studies difficult.
The current study developed a composite population PK model for HD-MTX from childhood into the adult years, and described the association between methotrexate exposure and toxicity. The final population PK model was used to simulate the expected exposure of MTX based on dosage regimen and patient characteristics. Because the current glucarpidase package insert recommends dosing based on expected MTX exposure, the simulation results can be applied to decision-making in glucarpidase dosing. The results of this study and the generated expected MTX exposures based on a broad study population will allow for more granular assessment of individual MTX concentrations in clinical practice and could improve early identification of patients at risk for slowed MTX clearance and toxic exposures.
References
Goldman ID, Matherly LH (1985) The cellular pharmacology of methotrexate. Pharmacol Ther 28(1):77–102
Ackland SP, Schilsky RL (1987) High-dose methotrexate: a critical reappraisal. J Clin Oncol 5(12):2017–2031. https://doi.org/10.1200/JCO.1987.5.12.2017
Howard SC, McCormick J, Pui CH, Buddington RK, Harvey RD (2016) Preventing and managing toxicities of high-dose methotrexate. Oncologist 21(12):1471–1482. https://doi.org/10.1634/theoncologist.2015-0164
Widemann BC, Adamson PC (2006) Understanding and managing methotrexate nephrotoxicity. Oncologist 11(6):694–703. https://doi.org/10.1634/theoncologist.11-6-694
Widemann BC, Balis FM, Kim A, Boron M, Jayaprakash N, Shalabi A, O’Brien M, Eby M, Cole DE, Murphy RF, Fox E, Ivy P, Adamson PC (2010) Glucarpidase, leucovorin, and thymidine for high-dose methotrexate-induced renal dysfunction: clinical and pharmacologic factors affecting outcome. J Clin Oncol 28(25):3979–3986. https://doi.org/10.1200/JCO.2009.25.4540
Monjanel S, Rigault JP, Cano JP, Carcassonne Y, Favre R (1979) High-dose methotrexate: preliminary evaluation of a pharmacokinetic approach. Cancer Chemother Pharmacol 3(3):189–196
Abelson HT, Fosburg MT, Beardsley GP, Goorin AM, Gorka C, Link M, Link D (1983) Methotrexate-induced renal impairment: clinical studies and rescue from systemic toxicity with high-dose leucovorin and thymidine. J Clin Oncol 1(3):208–216. https://doi.org/10.1200/JCO.1983.1.3.208
Widemann BC, Balis FM, Kempf-Bielack B, Bielack S, Pratt CB, Ferrari S, Bacci G, Craft AW, Adamson PC (2004) High-dose methotrexate-induced nephrotoxicity in patients with osteosarcoma. Cancer 100(10):2222–2232. https://doi.org/10.1002/cncr.20255
Green JM (2012) Glucarpidase to combat toxic levels of methotrexate in patients. Ther Clin Risk Manag 8:403–413. https://doi.org/10.2147/TCRM.S30135
Ramsey LB, Balis FM, O’Brien MM, Schmiegelow K, Pauley JL, Bleyer A, Widemann BC, Askenazi D, Bergeron S, Shirali A, Schwartz S, Vinks AA, Heldrup J (2018) Consensus guideline for use of glucarpidase in patients with high-dose methotrexate induced acute kidney injury and delayed methotrexate clearance. Oncologist 23(1):52–61. https://doi.org/10.1634/theoncologist.2017-0243
Glucarpidase Package Insert (2019) https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/125327lbl.pdf. Accessed May 7 2019
Cockcroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16(1):31–41. https://doi.org/10.1159/000180580
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20(3):629–637. https://doi.org/10.1681/ASN.2008030287
Zhang W, Zhang Q, Tian X, Zhao H, Lu W, Zhen J, Niu X (2015) Population pharmacokinetics of high-dose methotrexate after intravenous administration in Chinese osteosarcoma patients from a single institution. Chin Med J (Engl) 128(1):111–118. https://doi.org/10.4103/0366-6999.147829
Min Y, Qiang F, Peng L, Zhu Z (2009) High dose methotrexate population pharmacokinetics and Bayesian estimation in patients with lymphoid malignancy. Biopharm Drug Dispos 30(8):437–447. https://doi.org/10.1002/bdd.678
Johansson AM, Hill N, Perisoglou M, Whelan J, Karlsson MO, Standing JF (2011) A population pharmacokinetic/pharmacodynamic model of methotrexate and mucositis scores in osteosarcoma. Ther Drug Monit 33(6):711–718. https://doi.org/10.1097/FTD.0b013e31823615e1
Comandone A, Passera R, Boglione A, Tagini V, Ferrari S, Cattel L (2005) High dose methotrexate in adult patients with osteosarcoma: clinical and pharmacokinetic results. Acta Oncol 44(4):406–411. https://doi.org/10.1080/02841860510029770
Mei S, Li X, Jiang X, Yu K, Lin S, Zhao Z (2018) Population pharmacokinetics of high-dose methotrexate in patients with primary central nervous system lymphoma. J Pharm Sci 107(5):1454–1460. https://doi.org/10.1016/j.xphs.2018.01.004
Fukuhara K, Ikawa K, Morikawa N, Kumagai K (2008) Population pharmacokinetics of high-dose methotrexate in Japanese adult patients with malignancies: a concurrent analysis of the serum and urine concentration data. J Clin Pharm Ther 33(6):677–684. https://doi.org/10.1111/j.1365-2710.2008.00966.x
Dupuis C, Mercier C, Yang C, Monjanel-Mouterde S, Ciccolini J, Fanciullino R, Pourroy B, Deville JL, Duffaud F, Bagarry-Liegey D, Durand A, Iliadis A, Favre R (2008) High-dose methotrexate in adults with osteosarcoma: a population pharmacokinetics study and validation of a new limited sampling strategy. Anticancer Drugs 19(3):267–273
Hui KH, Chu HM, Fong PS, Cheng WTF, Lam TN (2019) Population pharmacokinetic study and individual dose adjustments of high-dose methotrexate in Chinese pediatric patients with acute lymphoblastic leukemia or osteosarcoma. J Clin Pharmacol 59(4):566–577. https://doi.org/10.1002/jcph.1349
Nader A, Zahran N, Alshammaa A, Altaweel H, Kassem N, Wilby KJ (2017) Population pharmacokinetics of intravenous methotrexate in patients with hematological malignancies: utilization of routine clinical monitoring parameters. Eur J Drug Metab Pharmacokinet 42(2):221–228. https://doi.org/10.1007/s13318-016-0338-1
Relling MV, Fairclough D, Ayers D, Crom WR, Rodman JH, Pui CH, Evans WE (1994) Patient characteristics associated with high-risk methotrexate concentrations and toxicity. J Clin Oncol 12(8):1667–1672. https://doi.org/10.1200/JCO.1994.12.8.1667
Widemann BC, Balis FM, Murphy RF, Sorensen JM, Montello MJ, O’Brien M, Adamson PC (1997) Carboxypeptidase-G2, thymidine, and leucovorin rescue in cancer patients with methotrexate-induced renal dysfunction. J Clin Oncol 15(5):2125–2134. https://doi.org/10.1200/JCO.1997.15.5.2125
Tsurusawa M, Gosho M, Mori T, Mitsui T, Sunami S, Kobayashi R, Fukano R, Tanaka F, Fujita N, Inada H, Koh K, Takimoto T, Saito A, Fujimoto J, Nakazawa A, Horibe K, Lymphoma committee of the Japanese Pediatric Leukemia/lymphoma Study G (2015) Statistical analysis of relation between plasma methotrexate concentration and toxicity in high-dose methotrexate therapy of childhood nonHodgkin lymphoma. Pediatr Blood Cancer 62(2):279–284. https://doi.org/10.1002/pbc.25305
Rask C, Albertioni F, Bentzen SM, Schroeder H, Peterson C (1998) Clinical and pharmacokinetic risk factors for high-dose methotrexate-induced toxicity in children with acute lymphoblastic leukemia–a logistic regression analysis. Acta Oncol 37(3):277–284
Buchen S, Ngampolo D, Melton RG, Hasan C, Zoubek A, Henze G, Bode U, Fleischhack G (2005) Carboxypeptidase G2 rescue in patients with methotrexate intoxication and renal failure. Br J Cancer 92(3):480–487. https://doi.org/10.1038/sj.bjc.6602337
Bhojwani D, Sabin ND, Pei D, Yang JJ, Khan RB, Panetta JC, Krull KR, Inaba H, Rubnitz JE, Metzger ML, Howard SC, Ribeiro RC, Cheng C, Reddick WE, Jeha S, Sandlund JT, Evans WE, Pui CH, Relling MV (2014) Methotrexate-induced neurotoxicity and leukoencephalopathy in childhood acute lymphoblastic leukemia. J Clin Oncol 32(9):949–959. https://doi.org/10.1200/JCO.2013.53.0808
Hegyi M, Gulacsi A, Csagoly E, Csordas K, Eipel OT, Erdelyi DJ, Muller J, Nemes K, Lautner-Csorba O, Kovacs GT (2012) Clinical relations of methotrexate pharmacokinetics in the treatment for pediatric osteosarcoma. J Cancer Res Clin Oncol 138(10):1697–1702. https://doi.org/10.1007/s00432-012-1214-2
Joerger M, Huitema AD, Krahenbuhl S, Schellens JH, Cerny T, Reni M, Zucca E, Cavalli F, Ferreri AJ (2010) Methotrexate area under the curve is an important outcome predictor in patients with primary CNS lymphoma: a pharmacokinetic-pharmacodynamic analysis from the IELSG no. 20 trial. Br J Cancer 102(4):673–677. https://doi.org/10.1038/sj.bjc.6605559
Acknowledgements
The authors would like to thank Dr. Sam Martinez, Dr. Jeremiah Momper, Dr. Lawrence Alejandro, and Dr. Don Barkauskas for help with the project. Funding support was provided by a Research in Pediatric and Developmental Pharmacology NIH grant (1U54HD090259-01, Dr. Capparelli).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Capparelli serves on the data safety and monitoring board for Melinta Pharmaceuticals, Cempra Pharmaceuticals and The Medicines Company.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kawakatsu, S., Nikanjam, M., Lin, M. et al. Population pharmacokinetic analysis of high-dose methotrexate in pediatric and adult oncology patients. Cancer Chemother Pharmacol 84, 1339–1348 (2019). https://doi.org/10.1007/s00280-019-03966-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-019-03966-4