Abstract
One of the most common complications in thalassemia major patients is osteopenia and osteoporosis. In this study, we compare the therapeutic effect of two treatment protocols involving infusion of 45 mg of pamidronate injection every 6 weeks (P45) and 90 mg pamidronate infusion every 4 weeks (P90). Bone mineral density was measured using dual energy X-ray absorptiometry (DEXA). Z-score of lumbar vertebra (as L total) and the femoral head (as F total) were compared before and after administration of two protocols. Bone density between the two groups was compared by Student t test and by the paired t test before and after the intervention. Data were analyzed using SPSS (18). Ninety-one patients were treated with pamidronate 45 mg (P45), and 36 patients were treated with pamidronate 90 mg (P90). Ninety-one and 36 patients received P45 and P90 protocol, respectively. Mean age was 29.4 ± 8.1 and 30.9 ± 8.0 years old in P45 and P90 groups, respectively. Sixty-two and 58 % of P45 and P90 group were female. The means of F total were −1.73 ± 1.11 and −1.47 ± 0.92 before and after treatment in patients P45 (P = 0.01) and were −1.83 ± 0.75 and −1.57 ± 0.99 in group P90 (P = 0.005), respectively. Before treatment, the means of L total were −2.95 ± 0.81 and −2.92 ± 0.66 (P = 0.8) and after treatment were −2.53 ± 1.13 and 2.81 ± 0.98 (P = 0.1) in P45 and P90 groups, respectively. In P45, between the mean of L total was statistically significant difference before and after treatment (P < 0.0001); however, there was no significant difference in the P90 group (P = 0.3). The study showed effectiveness of both protocols. As the medication is expensive and should be administrated parenterally, we recommend P45 protocol which is less expensive with fewer injections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thalassemia major is an inherited hemoglobinopathy due to defect in the ability in synthesis of beta-globin chains [1]. Thalassemia causes a defect in bone metabolism as a chronic hematological disorder which the balance between osteoblasts and osteoclasts activities was disturbed [2–4]. Osteoporosis is considered as a major cause of morbidity in both sexes in thalassemia cases [5, 6]. Osteoporosis and osteopenia are complications of beta thalassemia major. The prevalence of osteoporosis and osteopenia has been reported in 40–50 % of patients with thalassemia. The rate is higher among patients who have insufficient transfusions, and almost all patients who reach adulthood are suffering from this disease [7, 8]. Hypoxia caused by anemia is the main risk factor. However, other risk factors such as genetic predisposition, hypogonadism, male gender, diabetes mellitus, and inadequate physical activity are involved [9–13]. Symptoms of osteoporosis include bone pain and in case of severe osteoporosis; pathologic fractures may complicate the situation [5, 14, 15]. Currently, the most sensitive method for diagnosis is measurement of bone mineral density using dual energy X-ray absorptiometry (DEXA). Different methods are used for the treatment of osteoporosis in thalassemia cases including exercise, daily intake of calcium and vitamin D, sex hormone replacement, appropriate iron chelation, and the use of bisphosphonates [16, 17]. There is no consensus about the type and duration of treatment [17]. This study aimed to compare the response to the two protocols of intravenous infusion of pamidronate in patients with thalassemia major who referred to the Thalassemia Research Center.
Materials and methods
This was conducted by reviewing a database of patients with beta-thalassemia major between 2008 and 2014. Demographic and clinical characteristics including gender, age, weight, height, prescribed medication, and date of changes in the type of treatment were extracted from medical records. Body mass index (BMI) was calculated by the standard methods. Bone mineral density was measured using DEXA. Z-scores of lumbar vertebra and femoral head as F total and L total were recorded. Z ≤ −2.5 was considered eligible for pamidronate injections and continued to Z-score ≥−2. Pamidronate, as 90 mg/10 ml ampoules (made in Iran, Abureihan Co.), was diluted in 500 ml normal saline and then administered for 3 to 4 h intravenously. For one group to avoid wasting medication, one vial was used at the same time for two patients and this protocol was named P45. For the second group, the amount of pamidronate increased to 90 mg every 4 weeks (P90).
SPSS 18 software was used, and descriptive statistics and paired t test were used for comparing the situation before and after. Student t test was used to compare between groups. P < 0.05 was statistically considered as significant.
Results
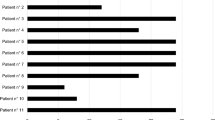
Ninety-one patients were treated with pamidronate 45 mg (P45), and 36 patients were treated with pamidronate 90 mg (P90). Demographic characteristics including, age, gender, body mass index, and duration of follow-up which were similar statistically (P < 0.05) are shown in Table 1.
The Z-score index at lumbar spine and the femoral head before and after treatment in the groups is shown in Tables 2 and 3. Severity of osteoporosis was not statistically different before the intervention (P < 0.05). After the treatment period, bone density index showed significant improvement in the femoral head in both groups. Bone mineral density in the lumbar spine showed improvement by P45 protocol; however, the difference was not statistically significant by P90 protocol (P < 0.05). Mean of changes in bone density of the femoral neck was 0.29 ± 0.78 (S.E. 0.09) in the P45 group and 0.29 ± 0.54 (S.E. 0.09) in the P90 group (P = 0.9). Also the means in differences of Z-score in lumbar vertebra in P45 and P90 were 0.40 ± 0.88 (S.E. 0.01) and 0.15 ± 0.89 (S.E. 0.15), respectively, which did not have a statistically significant difference (P = 0.1). Most patients complained of bone pain and fever (flu like) which were felt to a few hours for several days after drug administration and was managed with non-steroidal pain killers.
Discussion
The research showed that pamidronate was effective in the treatment of osteoporosis in patients with thalassemia major. Both protocols were equally effective in femoral head region; however, P90 protocol was not effective in lumbar vertebra. The duration of administration in P90 was 6 months shorter, but the difference was not significant statistically. Still one could argue that the intervention just prevented the osteoporosis from getting worse.
Voskaridou et al., in 2003, used pamidronate with doses of 30 mg per month, for 18 and 60 mg per month, for eight subjects, for a 12-month period in patients with thalassemia major. Their patients were in average 10 years older than ours. The severity of osteoporosis was similar in both groups and less than our patients. In both protocol, the Z-score of mineral density in the lumbar spine showed at least +0.4 improvement (P < 0.001). However, the difference of mineral density in the femoral head was not statistically significant in both protocols [3].
Naderi et al., in 2014, treated 20 female patients with thalassemia major who had osteoporosis by the infusion of 30 mg pamidronate monthly for 12 months [18]. The average age of patients was 23 years, younger than ours. BMI index was 18.1 kg/m2 according to the weight and height of patients. Their patients were thinner than ours but were similar in terms of the severity of osteoporosis. Their index was measured in grams per square centimeter in hip and lumbar spine place, not comparable with our study. Z-score of lumbar and hip was −2.98 ± −0.956 and −1.96 ± 0.727, respectively, and after the end of treatment had been recorded to be −2.44 ± 0.886 (P = 0.001) and −1.47 ± 0.856 (P = 0.003), respectively. The Z-score changes of +0.51 had been observed in the hip and +0.54 were statistically significant. The authors did not mention but if one vial of pamidronate was used for three patients, a good saving has been achieved. They conclude that their sample size was small and further studies were recommended [18].
Results of a meta-analysis showed that bisphosphonates, particularly zoledronic acid, had improved the bone density of cases with osteoporosis, while clodronic acid had not been effective [19].
Regarding the mechanism of action of the medication, Voskaridou et al. have investigated several indexes of bone metabolism before and after administration of pamidronate in thalassemic patients and age-matched healthy controls. N-Telopeptide of collagen (NTX), tartrate-resistant acid phosphatase isoform-5b (TRACP-5b), osteocalcin (OC), and bone-alkaline phosphatase (bALP) were significantly higher in thalassemic patients. Osteoprotegerin (OPG) was higher in healthy subjects. The soluble receptor activator of nuclear factor-kappa B ligand (sRANKLE) in thalassemic patients was within the normal range. Pamidronate reduced NTX, TRACP-b, OPG, and OC in thalassemic patients. They concluded that pamidronate inhibits the activity of osteoclasts [3].
Treatment with pamidronate is parenteral and complicated, expensive, and lengthy. Regarding the price, using only one vial every month for three patients as Naderi et al. showed is the least expensive protocol. Comparing P45 with P90 protocols of ours, the P45 would be cheaper if one vial was used for two patients. P90 protocol is the most expensive plan. Our previous report showed that the effectiveness of an Iranian generic product was comparable with a more expensive imported brand [20].
Regarding the duration of treatment, there is no agreement for the minimum time to treat such patients yet. Voskarido et al. and also Naderi et al. continued the treatment for 12 months [3, 21]. However, in this study, patients were treated and followed for 3 years.
At the end of the study, it was shown that bisphosphonates are effective in improving of bone density and prevent its decline. Comparison between two treatment protocols P90 and P45 showed that P45 increased the density of the lumbar spine and hip bone while P90 only increased the mineral density of hip bone. Slight improvement was observed in lumbar spine that was not statistically significant and perhaps had prevented the increasing of intensity. As a result, P45 protocol is recommended as a useful treatment because of cost-effectiveness, need to a lower dose, as well as the patients need to less refer. One of the main limitations of this study was that lack of the control group. The reason was ethical as there was evidence for beneficial effect of pamidronate. In this study, the genetic factors contributing to osteoporosis as well as indicators of osteoclasts activity were not investigated. Also effect on bone pain and quality of life was not assessed because of the lack of control group, so the high risk of bias.
References
Wonke B, Jensen C, Hanslip J, Prescott E, Lalloz M, Layton M et al (1997) Genetic and acquired predisposing factors and treatment of osteoporosis in thalassaemia major. Journal of pediatric endocrinology & metabolism: JPEM 11:795–801
Terpos E, Voskaridou E (2010) Treatment options for thalassemia patients with osteoporosis. Ann N Y Acad Sci 1202(1):237–43
Voskaridou E, Terpos E, Spina G, Palermos J, Rahemtulla A, Loutradi A et al (2003) Pamidronate is an effective treatment for osteoporosis in patients with beta-thalassaemia. Br J Haematol 123(4):730–7
Voskaridou E, Kyrtsonis MC, Terpos E, Skordili M, Theodoropoulos I, Bergele A et al (2001) Bone resorption is increased in young adults with thalassaemia major. Br J Haematol 112(1):36–41
Voskaridou E, Terpos E (2004) New insights into the pathophysiology and management of osteoporosis in patients with beta thalassaemia. Br J Haematol 127(2):127–39
Kosaryan M, Vahidshahi K, Jamali AE, Sarparast L (2012) Bone mineral density (BMD) of patients with beta thalassemia, Thalassemia Research Center, 2007. Journal of Mazandaran University of Medical Sciences (JMUMS) 22(86)
Di Stefano M, Chiabotto P, Roggia C, Garofalo F, Lala R, Piga A et al (2004) Bone mass and metabolism in thalassemic children and adolescents treated with different iron-chelating drugs. J Bone Miner Metab 22(1):53–7
Origa R, Fiumana E, Gamberini M, Armari S, Mottes M, Sangalli A et al (2005) Osteoporosis in β-thalassemia: clinical and genetic aspects. Ann N Y Acad Sci 1054(1):451–6
Dundar U, Kupesiz A, Ozdem S, Gilgil E, Tuncer T, Yesilipek A et al (2007) Bone metabolism and mineral density in patients with beta-thalassemia major. Saudi Med J 28(9):1425–9
Pietrapertosa A, Minenna G, Colella S, Santeramo T, Renni R, D'Amore M (2009) Osteoprotegerin and RANKL in the pathogenesis of osteoporosis in patients with thalassaemia major. Panminerva Med 51(1):17–23
Voskaridou E, Terpos E (2008) Pathogenesis and management of osteoporosis in thalassemia. Pediatric endocrinology reviews: PER 6:86–93
Scacchi M, Danesi L, Cattaneo A, Valassi E, Giraldi FP, Argento C et al (2008) Bone demineralization in adult thalassaemic patients: contribution of GH and IGF-I at different skeletal sites. Clin Endocrinol (Oxf) 69(2):202–7
Mahachoklertwattana P, Pootrakul P, Chuansumrit A, Choubtum L, Sriphrapradang A, Sirisriro R et al (2006) Association between bone mineral density and erythropoiesis in Thai children and adolescents with thalassemia syndromes. J Bone Miner Metab 24(2):146–52
Vogiatzi M, Autio K, Schneider R, Giardina PJ (2004) Low bone mass in prepubertal children with thalassemia major: insights into the pathogenesis of low bone mass in thalassemia. J Pediatr Endocrinol Metab 17(10):1415–22
Perrotta S, Cappellini MD, Bertoldo F, Servedio V, Iolascon G, D'agruma L et al (2000) Osteoporosis in β-thalassaemia major patients: analysis of the genetic background. Br J Haematol 111(2):461–6
Christoforidis A, Kazantzidou E, Tsatra I, Tsantali H, Koliakos G, Hatzipantelis E et al (2007) Normal lumbar bone mineral density in optimally treated children and young adolescents with B-thalassemia major. Hormones 6:334–40
Morabito N, Lasco A, Gaudio A, Crisafulli A, Di Pietro C, Meo A et al (2002) Bisphosphonates in the treatment of thalassemia-induced osteoporosis. Osteoporos Int 13(8):644–9
Naderi M, Zakeri Z, Dorgalaleh A, Alizadeh S, Tabibian S, Bamedi T (2014) Effect of pamidronate on osteoporosis in patients with β-thalassemia major. Iranian Journal of Blood and Cancer 6(3):149–53
Tsartsalis A, Lambrou G, Savvidis C, Chrousos G, Kattamis A (2015) Thalassemia-induced osteoporosis and bisphosphonate treatment: a systematic review and meta-analysis. 17th European Congress of Endocrinology EP 286. doi:10.1530/endoabs.37.EP286
Kosaian M (2011) The effect of intravenous biphosphonates in thalassemic patients with osteoporosis. In: 12th International Conference on Thalassemia, Turkey, 11–18 May
Giusti A (2014) Bisphosphonates in the management of thalassemia-associated osteoporosis: a systematic review of randomised controlled trials. J Bone Miner Metab 32(6):606–15
Acknowledgments
This research has been supported by Mazandaran University of Medical Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kowsaryan, M., Zafari, M. Which pamidronate protocol is the best for treating osteoporosis in beta-thalassemia major?. Ann Hematol 95, 383–386 (2016). https://doi.org/10.1007/s00277-015-2564-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-015-2564-z