Abstract
To determine the efficacy of zoledronic acid (ZA) in thalassemia major associated low bone mineral density. Prospective, open label, single arm trial. Bone mineral density (BMD) at lumbar, hip and forearm region were performed at baseline and after 1 year of therapy. Initial, 9 patients received a first dose of 4 mg. Due to severe adverse effects, further doses for these patients and all new recruited patients were 1 mg once every 3 months for 4 doses. All patients were receiving 500 mg of calcium carbonate twice daily and 0.25 μg alfacalcidol once daily before and during the entire study period. Dual energy X-ray absoptiometry was performed at baseline and after 1 year. Twenty-seven patients with transfusion dependent thalassemia with a median age 19.5 year (15–38 years) were eligible for ZA treatment. Seven patients had bony pains. Four patients developed grade 4 hypocalcemia (3 developed tetany) and 2 developed infusion related toxicity with initial dose of 4 mg. One mg dose was well tolerated. At the end of 1 year, bone pains had completely resolved. There was significant increase in BMD at lumbar (p = 0.002) and forearm regions (p = 0.04) and intertrochantric area (p = 0.041). The % change in BMD at 1 year was +3.7 ± 3.2%. ZA is an efficacious agent in treatment of low BMD in these patients. ZA produces significant adverse reactions at 4 mg dose but 1 mg dose is well tolerated and is efficacious.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low Bone mineral density (BMD) is emerging as an important cause of morbidity and disability in adults with transfusion dependent thalassemia [1]. Presence of osteopenia or osteoporosis in well-treated TM patients has been described in different studies with a frequency of approximately 40–50% [2]. We have recently documented 75–100% incidence of osteoporosis in Indian patients with thalassemia [3]. Merchant et al. [4] have documented an incidence of 81% osteoporosis in children from western Indian center. The overall fracture prevalence among all thalassemia syndromes was 12.1%, equally distributed between females (11.5%) and males (12.7%) [2]. We have earlier shown a fracture rate of 17% in our patients [3].
Bone mineral density (BMD) is a good index of bone status and the most important predictor of fracture risk [5]. Dual energy X-ray absorptiometry (DXA) is an excellent non-invasive choice for repeated measurements of any temporal changes of BMD because of 1% precision rate and low radiation exposure [6]. Bisphosphonates are potent inhibitors of osteoclastic bone resorption. They act by inhibiting osteoclastic recruitment and maturation, preventing the development of monocyte precursors into osteoclasts, inducing osteoclast apoptosis and interrupting their attachment to the bone [4]. In thalassemia osteoporosis, almost all generations of bisphosphonates have been used in an attempt to increase BMD and improve abnormal bone remodeling [1, 7].
One concern about administering oral bisphosphonates in thalassemia major is that many patients are unable to take these drugs due to poor tolerability; furthermore, gastrointestinal absorption of oral bisphosphonates is < 10%, and this absorption is further reduced by food containing milk or iron [2,3,4]. It is widely used for the treatment of osteolytic lesions of malignancies.
Zoledronic acid (ZA) in different doses has been shown to be effective in thalassemia associated low bone mineral density [8,9,10]. The intravenous route of administration is also an attractive alternative to oral bisphosphonates, as maintaining compliance with daily regimens for a predominantly asymptomatic condition represents a major problem [2]. Administration of treatment at intervals of 3 months, or even less frequently, is likely to be much more acceptable to patients and could reduce costs. This can be easily administered once patient is admitted for blood transfusion. One of the major risk associated with it has been osteonecrosis of jaw when used in patients with malignancies [11] and hypocalcemia [12].
There is lack of such data from India. This study was planned based on the hypothesis that zoledronic acid treatment would decrease bone resorption and thereby will reduce the fall in BMD or improve the bone mineral density (BMD) and reduce pain in thalassemia associated osteoporosis.
Patients and Methods
This is an open label, non-comparative, prospective single arm trial. Informed written consent was taken from all patients for this study. This was part of DM thesis. Institutes ethics committee cleared the study. Inclusion criteria included patient of transfusion dependent thalassemia with low bone mineral density. Exclusion criteria were non-transfusion dependent thalassemia, hypocalcemia, previous treatment with bisphosphonates for at least 12 months before the initiation of this study. Duration of the study period for each patient was 12 months from the initiation of therapy. Response Criteria were: significant decrease in the number of painful sites experienced by the patients, significant increase in their lumbar spine, femoral neck, trochanter, and total hip and forearm bone mineral density (BMD) measurements over the 12-month period.
Reconstituted ZA diluted with 100 ml of 0.9% w/v sodium chloride solution and was given as a single 15-min intravenous infusion. All patients were receiving 500 mg of calcium carbonate twice daily and 0.25 μg alfacalcidol once daily before and during the entire study period.
With first dose of 4 mg ZA, 4 patients developed grade 4 hypocalcemia and 3 developed tetany [13]. All 4 patients were treated with intravenous calcium gluconate. Joint swelling with pain and fever were present in another patient, which started 24 h after the drug injection. Fever subsided the same day, pain resolved in 4 days and joint swelling resolved after 11 days. There was no recurrence with repeat dose of 1 mg. Another girl developed fever with chills and joint pains which resolved with paracetamol. Joint symptoms abetted in 8–10 h and fever resolved after 36 h. She reported excessive sleepiness with the second dose. This lasted for 2 days. After these side effects, an in-house committee reviewed the protocol. It was felt that due to high prevalence of osteopenia/osteoporosis in our patients, ZA should be given to all patients. Committee reduced dose of ZA to 1 mg as one study had already shown efficacy of 1 mg ZA in thalassemia associated osteoporosis [8]. Girl with hypoparathyroidism was not administered any further doses of zoledronic acid. Other 3 patients with hypocalcemia, however, received subsequent doses at 1 mg.
All new enrolled 18 patients were subsequently given 1 mg ZA. There were no episodes of hypocalcemia after 1 mg ZA dose in these and any of the subsequent patients enrolled. After the revised schedule of 1 mg dose, one patient developed body pain and fever 10–12 h after the dose. The symptoms lasted for 5–6 h and responded to paracetamol. There was no recurrence with repeat doses. Another girl developed nausea and dizziness after the second dose. The symptoms started 8 h after the injection and lasted for about 6 h. Remaining all patients tolerated the drug well.
Data were analyzed using SPSS software (version 10; SPSS Inc., Chicago, Ill, USA). Students’ t test was applied to compare the means. Association between variables was compared using Pearson’s Chi Square test. p < 0.05 was considered significant.
Results
Forty patients were screened. Seven (17.5%) patients complained of bone pain. Pain scores of 1, 3, 4 and 5 were reported by 1, 2, 3 and 1 patient respectively. There were ten fractures in 7 patients (17.5%) at different sites on review of their history. Thirty five patients had low bone mineral density with forearm being the worst site with lowest BMD [3].
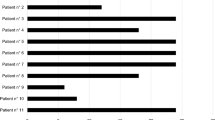
Figure 1 shows the consort diagram for study population. Twenty-seven patients were enrolled for ZA trial. In the initial phase of the study, 9 patients received a first dose of 4 mg. We observed significant side effects in our patient population [13]. Thus the dose of the drug was reduced to 1 mg every 3 months for 1 year for subsequent patients.
Bone pains had significantly decreased after ZA. After one dose only, 5 of 6 patients reported resolution of pain. In one girl, pain disappeared after second dose. There were no fracture episodes in the patients who took the injection while one (of 6 patients) who refused consent had a fracture of femoral shaft during the study period.
Table 1 shows the change in BMD in 21 patients who took ZA injections regularly. There was significant increase in BMD at lumbar and forearm regions. BMD also increased significantly at intertrochantric area and showed an improving trend at neck and trochanter. However, the net hip BMD was not significantly improved. Overall, the median BMD change after ZA was 0.028 g/cm2 (− 0.081 to 0.043 g/cm2). Three patients showed loss of BMD despite ZA treatment. Table 2 shows the bone mineral density changes and % changes at different sites. The mean change in BMD was 3.7 ± 3.2% while median change was 3.2% (− 12.4 to 27.8%). There was no difference in patients who received a first dose of 4 mg and subsequent 3 doses of 1 mg or throughout 1 mg dose.
In all, 3 of 21 patients showed loss in BMD, one patient had same BMD and rest 17 patients showed gain in BMD at lumbar region. At hip and forearm regions, 4 patients showed loss in BMD and rest 17 patients showed gain in BMD. Hypogonadism, iron overload and hepatitis C infection had no effect on improvement of BMD after ZA.
During follow-up, 2 patients died of restrictive cardiopmyopathy. One patient had hepatic encephalopathy in addition.
Discussion
Management of osteoporosis in thalassemia follows general principles. Treatment of thalassemic osteoporosis should be considered if osteoporosis is present or there is a history of fragility fracture, or in the setting of osteopenia with a high risk for fracture [7]. Oral alendronate, IV zoledronate, neridronate, and clodronate have been tested in randomized controlled trials. Even if head-to-head trials have not been done, zoledronate and neridronate has been suggested as first-line agents in the management [7].
The intravenous route of administration is an attractive alternative to oral bisphosphonates, as maintaining compliance with daily regimens for a predominantly asymptomatic condition represents a major problem [9, 10]. Administration of treatment at intervals of 3 months, or even less frequently, is likely to be much more acceptable to patients and could reduce costs. This can be administered in same setting when patient is admitted for transfusion. We had to reduce the dose of ZA to 1 mg to significant side effects primarily symptomatic hypocalcemia at 4 mg dose.
Overall, there was significant improvement in BMD at lumbar, intertrochantric region and forearm while there was an improving trend at neck and trochanter of femur. This increase was accompanied by dramatic reductions in bone pain. A 2-year follow-up showed continued increase in BMD and no added adverse effects in these patients [9]. Patients who refused ZA did not have an increase in BMD at any site.
A previous study showing that the percentage increase of BMD was greater in patients receiving ZA every 3 monthly as compared to those receiving it 6 monthly suggest that ZA needs to be given at least every 3 months in order to have a beneficial effect on BMD in thalassemic patients [14].
The increase in lumbar and forearm BMD observed was not associated with a similar increase in hip region BMD. This suggests that dynamics of bone formation and resorption may be different at different sites. Faster improvement of BMD in the forearm than other sites has been shown earlier and longer follow-up periods may be needed to reveal improvements in hip [9].
There was worsening of BMD at the studied sites in 3 patients. One patient was HIV positive. It is difficult to speculate what role HIV infection or concurrent antiretroviral therapy may have played in this patient. Going by the improvement in other patients, it is possible that there BMD might have decreased to greater extent if the drug was not administered.
We saw only one fracture incidence in one patient who had refused injection. This may reflect the short period of follow-up.
Bisphosphonates, in general have a good safety profile. Though mild biochemical hypocalcemia is common with administration of bisphosphonates, there are anecdotal reports of patient developing symptomatic hypocalcemia following IV administration of or ZA [12, 15]. The significant adverse effects at standard dose of 4 mg could be due to high prevalence of vitamin D deficiency in our population, unmasking of hypoparathyroidism and lower weight in our population [13].
However, if this reduction in dose has compromised the efficacy cannot be assessed at this stage. We saw a mixed response of the drug at different sites. Even Voskaridou and Terpos [1] who used the dose of 4 mg, could demonstrate improvement in BMD at lumbar spine only with negligible effect at hip and wrist. Acute systemic inflammatory reaction is often self-limited and becomes less intense during subsequent treatments [8, 10, 16].
Conclusions
Zoledronic acid at a dose of 1 mg every 3 months is effective in increasing the BMD of the forearm, femoral trochanter and intertrochantric region in patients with beta thalassemia major and pain scores are significantly reduced.
References
Voskaridou E, Terpos E (2004) New insights into the pathophysiology and management of osteoporosis in patients with beta thalassaemia. Br J Haematol 127(2):127–139
Cunningham MJ, Macklin EA, Neufeld EJ, Cohen AR (2004) Complications of b-thalassemia major in North America. Blood 104:34–39
Naithani R, Seth T, Tandon N, Chandra J, Pati H, Saxena R et al (2018) Fractures and low bone mineral density in patients with beta thalassemia major. Indian J Hematol Blood Transfus 34(1):163–165
Merchant R, Udani A, Puri V, D’cruz V, Patkar D, Karkera A (2010) Evaluation of osteopathy in thalassemia by bone mineral densitometry and biochemical indices. Indian J Pediatr 77(9):987–991
Morabito N, Lasco A, Gaudio A, Crisafulli A, Di Pietro C, Meo A, Frisina N (2002) Bisphosphonates in the treatment of thalassemia-induced osteoporosis. Osteoporos Int 13:644–649
Bansal D, Venkateshwaran S, Khandelwal N, Marwaha RK (2011) Quantitative computed tomography is unreliable for measurement of bone mineral density in inadequately chelated adolescent patients with β-thalassemia major: a case-control study. Pediatr Blood Cancer 56(3):409–412
Piga A (2017) Impact of bone disease and pain in thalassemia. Am Soc Hematol Educ Progr 2017(1):272–277
Perifanis V, Vyzantiadis T, Tziomalos K, Vakalopoulou S, Garipidou V, Athanassiou-Metaxa M et al (2007) Effect of ZA on markers of bone turnover and mineral density in osteoporotic patients with beta-thalassaemia. Ann Hematol 86(1):23–30
Voskaridou E, Christoulas D, Konstantinidou M, Tsiftsakis E, Alexakos P, Terpos E (2008) Continuous improvement of bone mineral density two years post ZA discontinuation in patients with thalassemia-induced osteoporosis: long-term follow-up of a randomized, placebo-controlled trial. Haematologica 93(10):1588–1590
Gilfillan CP, Strauss BJ, Rodda CP, Bowden DK, Kean AM, Obaid M et al (2006) A randomized, double blind, placebo-controlled trial of intravenous zoledronic acid in the treatment of thalassemia-associated osteopenia. Calcif Tissue Int 79(3):138–144
Kastritis E, Melea P, Bagratuni T, Melakopoulos I, Gavriatopoulou M, Roussou M et al (2017) Genetic factors related with early onset of osteonecrosis of the jaw in patients with multiple myeloma under zoledronic acid therapy. Leuk Lymphoma 58(10):2304–2309
Maalouf NM, Heller HJ, Odvina CV, Kim PJ, Sakhaee K (2006) Bisphosphonate induced hypocalcaemia: report of 3 cases and review of literature. Endocr Pract 12:48–53
Naithani R, Seth T, Tandon N, Chandra J, Pati H, Choudhry VP (2017) Safety of zoledronic acid in patients with thalassemia associated low bone mineral density. Indian J Hematol Blood Transfus. https://doi.org/10.1007/s12288-017-0858-0
Voskaridou E, Anagnostopoulos A, Konstantopoulos K, Stoupa E, Spyropoulou E, Kiamouris C et al (2006) Zoledronic acid for the treatment of osteoporosis in patients with beta-thalassemia: results from a single-center, randomized, placebo-controlled trial. Haematologica 91(9):1193–1202
Singh D, Khaira NS, Sekhon JS (2004) Symptomatic hypocalcaemia after treatment with zoledronic acid in a patient with multiple myeloma. Ann Oncol 15:1848
Giusti A (2014) Bisphosphonates in the management of thalassemia-associated osteoporosis: a systematic review of randomised controlled trials. J Bone Miner Metab 32(6):606–615
Funding
Financial support was obtained from Shantha Biotech for DXA scans of these children. Zoledronic acid injections were provided by Shantha Biotech free of cost.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed Consent
Informed consent was obtained from all individual participants included in the study. This was part of DM thesis.
Rights and permissions
About this article
Cite this article
Naithani, R., Seth, T., Tandon, N. et al. Zoledronic Acid for Treatment of Low Bone Mineral Density in Patients with Beta Thalassemia Major. Indian J Hematol Blood Transfus 34, 648–652 (2018). https://doi.org/10.1007/s12288-018-0953-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-018-0953-x