Abstract
The relative frequency of the non-Hodgkin lymphoma (NHL) subtypes varies around the world. The objective of this study was to describe the general features of patients with lymphoma in Colombia. A total of 819 patients with a new diagnosis of lymphoma were included. Nighty-nine (12 %) of them had Hodgkin lymphoma (HL) and 720 (88 %) had NHL. Most cases had advanced stage disease at presentation (63.6 %). Diffuse large B cell lymphoma (DLBCL) was the most frequent diagnosis; it was seen in 40 % of patients with NHL and in 35 % of patients in the whole series. Overall survival rates at 3 years were 77 % for HL and follicular lymphoma, 54 % for DLBCL, and 45 % for T cell lymphomas. In conclusion, the distribution of specific NHL subtypes is similar to what has been reported previously in other tropical countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lymphoid neoplasms have a wide range of biological, clinical, and morphological features. Even if restricted to the group of non-Hodgkin lymphoma (NHL), there is a wide variety of entities with different clinical features [1]. In recent years, there has been a growing awareness regarding this type of neoplasms, and as a result, cancer registries around the world report an increasing number of such malignancies with detailed classifications according to the histological subtype.
In epidemiological studies, different incidence rates of the NHL subtypes had been noted according to geographical site. In fact, when comparing populations from North America with those of Europe or the Far East, striking differences are noted. This suggests that environmental factors could be linked to the frequency of such malignancies [2–5]. A few studies are available in Latin American individuals, and information regarding the epidemiology of lymphoproliferative disorders is very limited in Colombia. The 2010 yearbook of the Colombian National Cancer Institute reported that 64 % of lymphoid neoplasms correspond to cases of NHL, and 36 % were cases of Hodgkin lymphoma (HL). Unfortunately, all cases of lymphoproliferative disorders that occur in our country are not included in this series and information regarding specific subtypes is not available [6].
The objective of the present study is to describe the general characteristics and some epidemiologic features of patients with lymphoma in Colombia. In order to include individuals with relatively different backgrounds, information has been gathered as part of a multicentric cooperation that includes patients from large clinical centers in the major cities of the country.
Methods
Between January 2000 and February 2013, a retrospective cohort study was carried out, consecutive patients with a new diagnosis of any kind of NHL or HL according to the World Health Organization (WHO) classification presenting to one of the three participating centers were included, and a chart review was undertaken. Cases of B cell NHL were sub-classified as high grade (Burkitt lymphoma, diffuse large B cell lymphoma, mantle cell lymphoma, and lymphoblastic lymphoma) or low grade (the remaining entities). Demographic characteristics, disease stage according to the Ann Arbor classification, and response to therapy according to the International Working Group criteria were registered for each case if available [7].
The primary objective was to adequately characterize the population of individuals with lymphoma in our country. As a secondary objective, we sought to estimate overall survival (OS) according to lymphoma subtype. OS was calculated from the date of the confirmation of the histopathological diagnosis until the date of death due to any cause. Patients that did not experience any event by February 28 2013 were censored.
Therapeutic regimens
Patients were treated according to each participating center clinical practice protocols, which can be summarized as follows. Anthracycline-based therapy was given to most patients with diffuse large B cell lymphoma (DLBCL) or mantle cell lymphoma (MCL), with the possible addition of cytarabine for the latter group. Patients with HL received ABVD chemotherapy with radiotherapy if necessary, whereas those with follicular lymphoma (FL) or mucosa-associated lymphoid tissue (MALT) lymphoma received either CVP or CHOP. Individuals with small lymphocytic lymphoma (SLL) that needed systemic treatment received chemotherapy regimens that included either fludarabine or chlorambucil. Fit individuals with Burkitt lymphoma (BL) were managed with intensive chemotherapy that included cytarabine as well as methotrexate. It should be noted that after 2005, rituximab became widely available in our country and it has been included as part of therapy for CD20+ B cell lymphomas since then. Most patients with T-cell lymphomas received CHOP or CHOP-like chemotherapy.
Statistical analysis
Central tendency measures were presented as means or medians according to data distribution. The chi-square test (or Fisher’s exact test as required) was used for the comparison of categorical variables. Survival analysis was performed according to the non-parametric method of Kaplan–Meier, and a comparison of the probability of survival was carried out with the log-rank test. The threshold for statistical significance was set at p < 0.05. STATA 11.2 was the software used for analysis. The ethics committee of each one of the participating institutions granted permission for the development of this investigation.
Results
Epidemiologic features
A total of 819 patients were included in the study. Mean age was 54 years (SD ± 19); 30 % were older than 65 years. There was a slight predominance of male individuals (1.4:1). Most cases had advanced stage disease at presentation (63.6 %). Cases of B cell NHL were predominantly classified as high grade (73.8 %). Other characteristics can be found in Table 1.
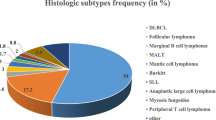
The distribution of cases according to histological diagnosis can be found in Table 2. Nighty-nine (12 %) of them had HL; their median age at diagnosis was 33 years (range 10–86 years). Meanwhile, 720 (88 %) individuals had NHL; their median age at diagnosis was 56 years (range 4–97 years). Most cases were of B cell origin (89 %). DLBCL was the most frequent diagnosis, as it was seen in 40 % of the patients with NHL. FL, SLL, and MALT lymphoma were seen in 11.7, 9, and 8 %, respectively. BL was diagnosed in 51 patients (7.1 %), with another 8 (1.1 %) having a diagnosis of B cell lymphoma, unclassifiable, with features intermediate between diffuse large B cell lymphoma and Burkitt lymphoma.
Response to therapy
Information regarding response to therapy was available for 457 patients. A complete response was achieved in 344 (75.2 %) and a partial response in 71 (15.6 %). Forty-two patients (9.2 %) had either stable or progressive disease.
Overall survival
Three hundred fifty-four patients with available information and a follow-up time of at least 3 months were included in this analysis. OS at 3 years was 77 and 62 % for patients with HL and NHL, respectively (p = 0.02; Fig. 1). In the group of patients with NHL, OS at 3 years was 64 and 45 % for individuals with B cell lymphomas and T cell lymphomas, respectively (p < 0.001). OS at 3 years for patients with DLBCL, FL, and SLL was 54, 77, and 61 %, respectively (Fig. 2). Notably, OS was substantially higher among patients with B cell lymphomas diagnosed and treated during the second half of the study period (OS at 3 years 86 vs 52 %, p = 0.003; Fig. 3).
Discusion
Lymphoid neoplasms comprise a heterogeneous group of malignancies with very diverse clinical features and prognosis. One key characteristic is the wide variation in the relative frequency of presentation of the specific subtypes according to the geographical location [2]. True epidemiology of lymphomas in a resource-limited country as Colombia is difficult to establish, as these neoplasms are not systematically reported to government agencies [6]. Some information derived from international cancer registries is available; however, it is uncertain if it is really representative of our population. [8]. The present study increases the information available on this topic in Latin America and is by far the largest on this subject carried out in our country.
Previously, it has been suggested that HL represents approximately 10 % of all lymphoma diagnosis and T cell lymphoma accounts for approximately 10 % of cases of NHL [2, 4, 5, 9–12]. Our findings confirm this, as the proportion of patients with HL and T cell lymphoma was 12 and 11 %, respectively. Interestingly, DLBCL was the most frequently diagnosed neoplasm. In fact, low-grade lymphomas even if grouped together were less frequent than DLBCL (23 vs 40 %, p = 0.03). A similar behavior was observed among Asian, European, and some Latin American populations [4, 5, 12–14]. However, this predominance of DLBCL over other subtypes has not been found in previous studies carried out in North American population, where indolent lymphomas are more prevalent [2, 15]. Laurini et al. in a large study that included individuals from Central and South America (CSA) found an increased relative frequency of high-grade B cell neoplasms among patients from Brazil, Guatemala, and Peru. When considering the region of origin, they also confirmed that DLBCL was significantly more frequent among patients from CSA than among North Americans (40 vs 29.2 %) [14]. Some explanations for these variations had been proposed. First, genetic influences as well as environmental factors could be responsible. Unfortunately, we do not have information regarding the specific genomic background or previous harmful exposure in our patients to elaborate more in this regard. Second, socioeconomic differences could also be relevant, as countries with a lower income per capita have a greater frequency of high-grade lymphomas [11, 14]. Third, it is well established that indolent lymphomas can transform into more aggressive entities, mainly DLBCL [16]. An intriguing hypothesis is that some cases of DLBCL seen by us were initially other lymphomas that have transformed. Difficulties in the access to health services could lead to a reporting bias; sicker individuals get admitted to hospitals whereas others with less severe presentations (i.e., indolent lymphomas) are not. As large reference centers were the source of patients for the present study, this situation could indeed influence our findings.
Eight percent of patients with NHL had either BL or B cell lymphoma, unclassifiable, with features intermediate between diffuse large B cell lymphoma and Burkitt lymphoma. This rate is higher than what has been reported previously elsewhere, with the notable exception of a study done in Guatemala [2, 4, 12, 14, 17]. A possible explanation for the aforementioned finding is that Malaria (which is endemic in our country) and Epstein–Barr virus (EBV) infection might interact and predispose individuals to the development of these malignancies [18]. EBV infects a large number of B cells during primary viremia. This initial proliferative period is eventually controlled by the action of specific T cell subsets; however, EBV persists indefinitely in memory B cells [19]. Later on, a reactivation of EBV viremia occurs when the patient is exposed to plasmodium, as this infection is associated with an increased B cell activation [20]. This synergy among both pathogens could lead to an increased risk of lymphoma development. The role of human immunodeficiency virus infection as a risk factor for the development of BL is also well established [1, 11]. Unfortunately, we do not have serologic information of the individuals included in this study to draw any meaningful conclusions.
We found an OS rate at 36 months of 77 % for HL and FL, 61 % for SLL, 54 % for DLBCL, and 45 % for T cell lymphomas. These rates are comparable to those reported in large contemporary international series where patients received similar therapy as the ones included in the present study [3, 21, 22]. Nevertheless, the outcome of patients with SLL and DLBCL was suboptimal, as recent series report a median OS greater than 3 years for most patients [23–25]. An explanation for this discrepancy is not entirely clear; the uneven use of rituximab could be partly responsible. In fact, when we analyzed OS according to the study period, we noted a higher survival rate among patients diagnosed and treated after 2005, the year that this medication became widely available in Colombia. Other factors could also be responsible and deserve mention; Shenoy et al. conducted a retrospective analysis of patients with DLBCL classified according to their ethnicity and found inferior outcomes among African American individuals [26]. Socioeconomic differences were stated as potentially accountable for the poor outcomes and could also be operative in our population. Finally, a consideration should be made regarding the possibility of inclusion of a more infirm population of patients in the present study. Individuals with SLL are usually elder and have a significant burden of comorbid states. The age of the individuals with this diagnosis in the present series was higher than that of the patients included in a recent large study (66 vs 61 years) [25]. As a formal comorbid assessment was not done by us, the impact of other disease states cannot be accounted for.
The fact that the present study represents a collaborative multicenter effort is its principal strength. Patients were evaluated in large teaching hospitals located in one of the three major cities of the country. Even though a central pathology review was not carried out, each one of the pathology specimens was evaluated by trained hematopathologists according to WHO criteria. Notably, this study is the largest description of this type of neoplasms in our country, and we strongly believe that is also a reflection of real-life practice. Besides what has been stated previously, the retrospective design has to be taken into consideration among its limitations. Due to differences in the registration of information, response to therapy was not available for each episode. The possibility of misdiagnosis of some cases, a relatively frequent phenomenon as mentioned by Laurini et al. has to be acknowledged as well [14]. Also, the increased frequency of DLBCL should be studied further. Details regarding the neoplastic cell of origin would be helpful and could explain the poor prognosis among these individuals. Last, patient follow-up was rather limited, especially for indolent lymphomas which nowadays have long survival times.
In summary, we provide a description of general features of lymphoma in Colombia. The relative frequency of specific subtypes of NHL is similar to what has been reported in other tropical countries as Brazil or Peru. Our findings lend further support to the hypothesis that genetic and environmental factors are strong influences that determine the frequency of presentation of specific malignancies. OS of patients with DLBCL was somewhat lower than what has been previously reported.
References
Swerdlow SH (2008) WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th edn (International Agency for Research on Cancer. World Health Organization, Lyon
Anderson JR, Armitage JO, Weisenburger DD (1998) Epidemiology of the non-Hodgkin’s lymphomas: distributions of the major subtypes differ by geographic locations. Non-Hodgkin’s Lymphoma Classification Project. Ann Oncol 9:717–720
Vose J, Armitage J (2008) Weisenburger D; International T-Cell Lymphoma Project. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol 26:4124–4130
Yang QP, Zhang WY, Yu JB et al (2011) Subtype distribution of lymphomas in Southwest China: analysis of 6,382 cases using WHO classification in a single institution. Diagn Pathol 6:77
Yoon SO, Suh C, Lee DH et al (2010) Distribution of lymphoid neoplasms in the Republic of Korea: analysis of 5318 cases according to the World Health Organization classification. Am J Hematol 85:760–764
Murillo RH, Piñeros M, Acosta JA, Castellanos VH (2012) Instituto Nacional de Cancerología Anuario Estadístico 2010. Volumen 8 (Instituto Nacional de Cancerología: Bogotá, Colombia)
Cheson BD, Pfistner B, Juweid ME (2007) Revised response criteria for malignant lymphoma. J Clin Oncol 25:579–86
Parkin DM (2006) The evolution of the population-based cancer registry. Nat Rev Cancer 6:603–612
Townsend W, Linch D (2012) Hodgkin's lymphoma in adults. Lancet 380:836–847
Roman E, Smith AG (2011) Epidemiology of lymphomas. Histopathology 58:4–14
Shankland KR, Armitage JO, Hancock BW (2012) Non-Hodgkin lymphoma. Lancet 380:848–857
Novelli S, Briones J, Sierra J (2013) Epidemiology of lymphoid malignancies: last decade update. Springerplus 2:70
Luminari S, Cesaretti M, Rashid I et al (2007) Incidence, clinical characteristics and survival of malignant lymphomas: a population based study from cancer registry in northern Italy. Hematol Oncol 25:189–197
Laurini J, Perry A, Boilesen E et al (2012) Classification of non-Hodgkin lymphoma in Central and South America: a review of 1028 cases. Blood 120:4795–4801
Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS (2006) Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood 107:265–76
Montoto S, Fitzgibbon J (2011) Transformation of Indolent B-Cell Lymphomas. J Clin Oncol 29:1827–34
Perry AM, Molina-Kirsch KH, Nathwani BN et al (2011) Classification of non-Hodgkin lymphomas in Guatemala according to the World Health Organization system. Leuk Lymphoma 52:1681–1688
Morrow RH Jr (1985) Epidemiological evidence for the role of falciparum malaria in the pathogenesis of Burkitt's lymphoma. IARC Sci Publ 60:177–86
Thorley-Lawson DA, Gross A (2004) Persistence of the Epstein–Barr virus and the origins of associated lymphomas. N Engl J Med 350:1328–1337
Chene A, Donati D, Orem J et al (2009) Endemic Burkitt's lymphoma as a polymicrobial disease: new insights on the interaction between Plasmodium falciparum and Epstein-Barr virus. Semin Cancer Biol 19:411–20
Diehl V, Franklin J, Pfreundschuh M et al (2003) Standard and increased-dose BEACOPP chemotherapy compared with COPP-ABVD for advanced Hodgkin's disease. N Engl J Med 348:2386–95
Hiddemann W, Kneba M, Dreyling M et al (2005) Frontline therapy with rituximab added to the combination of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) significantly improves the outcome for patients with advanced-stage follicular lymphoma compared with therapy with CHOP alone: results of a prospective randomized study of the German Low-Grade Lymphoma Study Group. Blood 106:3725–32
Sehn LH, Donaldson J, Chhanabhai M et al (2005) Introduction of combined CHOP plus rituximab therapy dramatically improved outcome of diffuse large B-cell lymphoma in British Columbia. J Clin Oncol 23:5027–33
Cunningham D, Hawkes EA, Jack A et al (2013) Rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone in patients with newly diagnosed diffuse large B-cell non-Hodgkin lymphoma: a phase 3 comparison of dose intensification with 14-day versus 21-day cycles. Lancet 381:1817–26
Hallek M, Fischer K, Fingerle-Rowson G et al (2010) Addition of rituximab to fludarabine and cyclophosphamide in patients with chronic lymphocytic leukaemia: a randomised, open-label, phase 3 trial. Lancet 376:1164–74
Shenoy PJ, Malik N, Nooka A et al (2011) Racial differences in the presentation and outcomes of diffuse large B-cell lymphoma in the United States. Cancer 117:2530–40
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Combariza, J.F., Lombana, M., Torres, A.M. et al. General features and epidemiology of lymphoma in Colombia. A multicentric study. Ann Hematol 94, 975–980 (2015). https://doi.org/10.1007/s00277-015-2301-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-015-2301-7