Abstract
Due to genetic heterogeneity of β-thalassemia (β-thal) patients, several efforts have been undertaken to determine the efficacy of hydroxyurea treatment. The aim of this work is to determine the responder and nonresponder for hydroxyurea treatment in β-thal intermedia based on γ-globin mRNA and fetal hemoglobin (HbF) induction in human erythroid progenitor cells purified from a patient’s peripheral blood. Eighteen β-thal/hemoglobin E patients [13 βE/codon41/42(-TCTT), 4 βE/codon17, and 1 βE/IVS-654], requiring blood transfusion occasionally, with Hb levels of 5.20–8.50 g/dl were studied. The relative levels of γ-globin mRNA was measured by real-time reverse-transcription polymerase chain reaction and HbF by high-performance liquid chromatography. The results indicated that erythroid progenitor cells treated with 30 μmol/l hydroxyurea for 96 h preferentially enhanced Gγ-and Aγ-globin mRNA. The mean values of Gγ-globin mRNA fold induction were higher than Aγ-globin mRNA (12±4 vs 4±0.30), the Pearson’s correlation of Gγ-and Aγ-globin mRNA was r=0.80. Induction of Gγ/Aγ globin mRNA is up to ninefold. A 30% increase in the proportion of HbF out of the total Hb was found in cultures derived from four patients, 20–30% in cultures from nine patients, and less than 20% in cultures from five patients. In cultures from only two patients, increase in the proportion of HbF was less than 3%, and Gγ/Aγ globin mRNA is less than 0.50.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Beta-thalassemia (β-thal) is characterized by insufficient production of adult β-globin chains with subsequent accumulation of aggregates of unpaired, insoluble α-globin chains, which lead to ineffective erythropoiesis and intramedullar degradation of erythroid cells [1, 2]. The phenotypic presentation correlate with the degree of α/β imbalance [1]. It has been suggested that increased levels of fetal hemoglobin (HbF) could improve the clinical features of β-thalassemia patients, due to an improvement in the balance of α/non-α globin chains [3, 4]. Several pharmacological agents such as erythropoietin, 5-azacytidine, butyrate derivatives, hydroxyurea and combinations of these drugs have been shown to possess γ-globin chain inducing activity [5–7]. Hydroxyurea has been reported to give pronounced increase of HbF production; a decrease in cell number due to inhibition of proliferation; an increase in hemoglobin content per cell; and an increase in cell size in a two phase erythroid cell culture system [8] and was proposed that this may recapitulate the enhanced proliferation of HbF-containing erythroid cells which is thought to occur in vivo. Some studies have reported a correlation between increased HbF and total Hb, while others have shown that patients with increased HbF levels did not show increase in total Hb after treatment with hydroxyurea [9, 10]. In this report, we therefore study the hydroxyurea response in erythroid progenitor cells from β-thalassemia/HbE patients peripheral blood, by determining the synthesis of γ-globin mRNA and HbF , to identify candidates for HbF induction by hydroxyurea.
Patients and materials
Eighteen β-thal/HbE patients (who have never been treated with hydroxyurea) with various β-thal mutation (13 β E/codon 41/42(-TCTT), 4 βE/codon 17, and 1 βE/IVS-654) with normal α-globin genotype were studied. Genotyping of β-thal mutations was performed using reverse-dot blot hybridization, and β-thal mutation was determined by the gap polymerase chain reaction (PCR) [11, 12]. After informed consent was obtained, hematologic data, Hb analysis, and reticulocyte count were determined by conventional methods. Clinical assessment was based on severity of anemia, blood transfusion requirement and degree of growth impairment, and spleen enlargement. Primary erythroid progenitor cells were prepared by a modified method previously described [13, 14]. Thirty milliliters of human peripheral blood collected in vacuum glass tubes containing ethylenediamine tetracetic acid (EDTA) as an anticoagulant was obtained from β-thal/HbE patients. Light-density mononuclear cells were obtained by density centrifugation using Ficoll-Hypaque (1.07 g/ml, GIBCO BRL, Grand Island, NY). Red blood cells were lysed by suspending the mononuclear cell pellet in red cell lysis buffer (0.16 mol/l ammonium chloride, 10 mmol/l potassium bicarbonate, and 5 mmol/l EDTA). Platelets were removed by cell centrifugation at 200 g for 10 min through phosphate-buffered saline (PBS) containing 10% human serum albumin (HSA). Adherent cells were depleted by a 1 h incubation in a polystyrene tissue culture flask at 4°C. Nonadherent cells were then collected, and two cycles of negative selection were performed using anti-CD3, anti-CD11b, anti-CD15, and anti-CD45RA antibodies and immunomagnetic beads with Vario-Macs columns (Mitenyi Biotech, Auburn, CA). The remaining cells of 1–3×105 cells per milliliter were then cultured in Iscove’s modified Dulbecco’s medium (IMDM; GIBCO BRL) containing 15% heat-inactivated fetal calf serum, 15% pooled human AB serum, 2 U/ml erythropoietin (EPO), 20 ng/ml stem cell factor (SCF), 10 ng/ml interleukin (IL)-3, 100 U/ml penicillin, and 100 mg/ml streptomycin (GIBCO). The cells were incubated at 37°C in a high-humidity, 5% CO2, 95% air incubator (day 0). On day 3, the cells [late burst-forming unit erythroid (BFU-E)] were centrifuged and then collected and incubated under the same conditions in fresh medium, but without IL-3. The purity of the colony-forming unit erythroid (CFU-E) was determined by measuring the percentage of cells which can form erythroid colonies in the plasma clot assay [15–18]. The cells which cannot form erythroid colonies are mainly proerythroblast (BFU-E) and late erythroblast (late BFU-E), as shown by cytospin morphological studies [18].
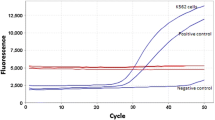
The cultured medium was changed, and hydroxyurea (Sigma) was added on day 6 and collected on day 10. The purity of day 6 erythroid progenitor cells with proerythroblast-like features was assessed by cytospin preparations in each experiment. The purity of the cells is important in this study because there is asynchronous synthesis of HbF and HbA during erythroblast maturation; HbF is produced predominantly in the early pro-and basophilic erythroblasts [19–21]. Viability of the cells was determined by trypan blue exclusion technique using a hemocytometer. The number of Hb-containing cells was determined by means of the benzidine-HCl procedure [12]. Hemoglobin types in the cell lysate were separated and quantitated of Hb A2, HbE, and HbF by automated high-performance liquid chromatography (HPLC) (VARIANT; BioRad, Hercules, CA, USA) [5]. RNA was extracted according to the method of Chomczynski [22]. The real-time quantitative competitive (QC) RT-PCR was performed as previously reported [23]. Synthetic oligonucleotide primers and the fluorescently labeled oligonucleotide hybridization probes were synthesized by PerkinElmer Applied Biosystem (Foster City, CA, USA). Primer and probe sequences are α-globin sense primer GAGGCCTGGAGGATGTTC, α-globin antisense primer CGTGGCTCAGGTCGAAGTG, and α-globin probe TGTCCTTCCCCACCACCAAGACCTACT; Gγ-globin sense primer CTGGCAGAAGATGGTGACTGG and Gγ-globin antisense primer CTCTGCATCATGGGCAGTGA; Aγ-globin sense primer CTGGCAGAAGATGGTGACTGC, Aγ-globin antisense primer CTCTGCATCATGGGCAAGAG, and Gγ-and Aγ-globin probe CAGTGCCCTGTCCTCCAGATACCACTGA. The α-and γ-globin probe was 5' end labeled with tetrachloro-6-carboxyfluorescein (TET) and VIC, respectively. All probes contained quencher fluor, 6-carboxytetramethylrhodamine (TAMRA) at the 3' end. All samples were assayed in triplicate in a MicroAmp Optical 96-well reaction plate (PerkinElmer). Reagents for the one-step RT-PCR were from the TaqMan Gold RT-PCR kit (PerkinElmer) using procedures recommended by the manufacturer. RNA from a normal sample and from cord blood was used as standards for quantitation of α-and γ-globin mRNA, respectively. RT-PCR thermal cycling reaction was performed as follows: 48°C for 30 min; 95°C for 10 min, 40 cycles of 95°C for 15 s, and 60°C for 1 min. Amplifications were carried out in an ABI PRISM 7700 sequence detection system (PE Applied Biosystem). Statistics were obtained with Student’s t test.
Results
At day 0, peripheral blood cells are cultured in the presence of a combination of growth factors (2 U/ml EPO, 20 ng/ml SCF, and 10 ng/ml IL-3), and most of the cells are early erythroid-committed progenitors (BFU-E) [15–18]. The cells then proliferate and differentiate into late BFU-E after culture for 3 days. The cells then continue to proliferate and differentiate into more mature colony-forming unit-like progenitors (CFU-E) on day 6 [13]. The cells continue to proliferate and differentiate into more matured erythroid progenitors such as orthochromatic normoblasts. Most of the cells that were treated with 30 μM hydroxyurea at day 6 and collected at day 10 consisted of basophilic and polychromatophilic normoblasts, which were similar to the untreated culture control. Maturation of red cells to orthochromatophilic erythroblasts was observed when the hydroxyurea-treated cells were cultured on day 13 (Table 1). However, delayed cell maturation occurred when hydroxyurea was added earlier than day 3 of culture. The average number of viable erythroid cells of the untreated control and hydroxyurea-treated cells from days 3 to 10 was 2–6×106 and 0.50–1.50×106 cells per milliliter, respectively; from days 6 to 10, the average number was 2–6×106 and 1–5×106 cells per milliliter, respectively. Various concentrations of hydroxyurea have been evaluated for the minimal effect on cellular proliferation. Hydroxyurea at 30 μmol/l was previously found to have significantly increased fractional HbF contents in β-thal/HbE patients (data not shown). Hydroxyurea increased HbF production in all cultures derived from 18 â-thal/HbE patients with different degrees of stimulation; as the increase in the proportion of HbF out of the total Hb varied from 2 to 35% (Table 2), it is equal to the absolute amount (in HbF) of 0.53–2.68 g/dl. The real-time QC RT-PCR was used to determine the relative induction of Gγ-and Aγ-globin mRNA to α-globin mRNA to normalize the variation in the starting mRNA concentrations. The changes in the globin mRNA in â thal/HbE erythroid cultures with or without 30 μmol/l hydroxyurea treatment for 96 h is shown in Table 3. The results indicated that erythroid progenitor cells treated with 30 μmol/l hydroxyurea for 96 h preferentially enhanced Gγ-and Aγ-globin mRNA. The mean values of Gγ-globin mRNA fold induction were higher than Aγ-globin mRNA (12±4 vs 4±0.30), and the Pearson’s correlation of Gγ-and Aγ-globin mRNA was r=0.80. The addition of 30 μM hydroxyurea to human erythroid cell cultures preferentially enhanced γ-globin mRNA synthesis, either Gγ-and/or Aγ-globin mRNA, in all patients (Table 3). This is shown by the fold induction of transcripts calculated by setting the transcription levels of untreated control (without hydroxyurea) at 1. In conclusion, Gγ-globin mRNA in culture erythroid cells increased by 0.05-to 12-fold over the untreated control cultures, whereas the Aγ-globin mRNA fold induction was 0.20–4. The Pearson’s correlation of Gγ-and Aγ-globin mRNA was r=0.80. Stimulation of Gγ-globin gene expression as compared to Aγ-globin gene was determined as the Gγ/Aγ-globin mRNA, which was up to ninefold over the untreated control cultures.
Discussion
Patients with β-thal/HbE have different degree of severity despite of the same genotype [24, 25]. Therefore, it is interesting to perform an in vitro study of HbF induction using hydroxyurea in β-thal/HbE patients. Human erythroid progenitor liquid culture was used as a model system for the investigation of agents that may affect globin gene expression. This model is considered to be superior to other similar systems such as erythroleukemia cell lines and semisolid cultures because it allows terminal differentiation of the erythroid cells. In addition, the human erythroid cultures allow us to determine the effect of various drugs added at various stages of erythroid maturation to be tested [8, 26, 27]. Our study using real-time QC RT-PCR, a rapid and sensitive technique for precise quantification of mRNA template, revealed diversity in the values of each transcript. In this report, hydroxyurea induced HbF production in cultures of cells derived from 18 β-thal/HbE patients with different degrees of response. The differences in hydroxyurea response were also reported in other HbF-modulating agents, which were used in different kinds of hemoglobinopathies [28, 29]. It is well established that increased HbF levels of 30% of the total Hb leads to a significant improvement of the clinical status of the patients with sickle cell disease and β-thal patients [29–31]. In our study, increased HbF levels over 30% of the total Hb were found in four patients, 20–30% in nine patients, and less than 20% in five patients. In cultures of cells derived from only two patients, the increase in HbF was less than 3%; hence, these patients may potentially be nonresponders (Table 2). It is of interest that all 18 β-thal/HbE patients studied are all thalassemia intermedia with Hb levels ranging from 5.2 to 8.5 g/dl. This study implied that patients with thalassemia intermedia, including β-thal/HbE patients, showed quite good response to hydroxyurea treatment in vitro because 11 βE/codon 41/42(-TCTT ), 4 βE /codon 17, and 1 βE /IVS-654 patients are responders, and only 2 βE /codon 41/42(-TCTT ) are nonresponders. A slight increase in α-globin mRNA demonstrated in this study is also similar to the previous study, which showed that treatment with hydroxyurea resulted in increases in α-and γ-globin levels [32]. The relative increase in each globin might be influenced not only by the particular β-globin genetic defect but also by other genetic modifiers such as demethylation of the γ-globin genes, leading to increased γ-globin gene activity in sickle-cell patients treated with hydroxyurea [33]. In this study, hydroxyurea stimulated HbF synthesis by induction of Gγ/Aγ-globin mRNA ratio up to ninefold (Table 3). The results also agree with previous work showing that the increased HbF reflects increased transcription and more efficient processing of the respective γ-globin mRNA [34]. Some erythroid cell culture from β-thal/HbE patients showed large increases in γ-globin mRNA but little increase in HbF; this indicated that γ-globin mRNA induction was affected mostly at the transcriptional level. However, the results also showed that hydroxyurea stimulates in some patients increase in alpha-globin mRNA together with gamma globin mRNA (Table 3). In this report, most of the cells in hydroxyurea-treated erythroid culture at day 10 (from day 6 to day 10) consisted of basophilic and polychromatophilic normoblast, which was similar to the untreated culture control in seven patients studied. Maturation of red cells to orthochromatophilic erythroblasts was observed when the hydroxyurea-treated cells were cultured on day 13 (Table 2). However, delayed cell maturation occurred when hydroxyurea was added earlier than day 3 of culture. Nevertheless, the entire mechanism whereby erythroid regeneration stimulates HbF production remains to be determined. In conclusion, our approach should be considered as a basis for further efforts to test novel potential pharmacological modulators of hemoglobin production.
References
Higgs DR, Thein SL, Woods WG (2001) The physiology of the thalassemia. In: Weatherall DJ, Clegg B (eds) The Thalassemia Syndromes, 4th ed. Blackwell Science Ltd, Oxford, pp 265–284
Weatherall DJ (2001) The thalassemias. In: Stamatoyannopoulos G, Majerus PW, Perimutter RM, Varmus.H (eds) The molecular basis for blood disorders, WB Saunders, Philadelphia PA, pp 183–226
Charache S, Terrin ML, Moore RD et al (1995) Effect of hydroxyurea on the frequency of painful crises in sickle cell anemia. N Engl J Med 332:1317–1322
Fucharoen S, Siritanaratakul N, Winichagoon P, Chowthaworn J, Siriboon W, Muangsup W, Chaicharoen S, Poolsup N, Chindavijak B, Pootrakul P, Piankijagum A, Schechter AN, Rodgers GP (1996) Hydroxyurea increases hemoglobin F levels and improves the effectiveness of erythropoiesis in beta-thalassemia/hemoglobin E diseases. Blood 87:887–892
Fucharoen S, Winichagoon P, Wisedpanichkij R, Sae-Ngow B, Sripanich R, Oncoung W, Muangsapaya W, Chowthaworn J, Kanokpongsakdi S, Bunyaratvej A, Piankijagum A, Dewaele C (1998) Prenatal diagnoses of thalassemias and hemoglobinopathies by HPLC. Clin Chem 44:740–748
Maier-Redeiersperger M, De Montalembert M, Flahault A et al (1998) Fetal hemoglobin and F-cell responses to long-term hydroxyurea treatment in young sickle cell patients. Blood 91:4472–4479
Rodgers GP, Sauntharajah Y (2001) Advances in experimental treatment of beta thalassemia. Exp Opin Invest Drugs 10:925–934
Fibach E, Burke LP, Schechter AN, Nogusi CT, Rodgers GP (1993) Hydroxyurea increases fetal hemoglobin in cultured erythroid cellsderived from normal individuals and patients with sickle cell anemia. Blood 81:1630–1635
Aker M, Dover G, Schrier S, Rachmilewitz EA (1995) Combination of erythropoietin and hydroxyurea results in improved quality and quantity of RBC in 7 patients with thalassemia intermedia. In: Beuzard Y, Lubin B, Rosa J (eds) Sickle cell disease and thalassemias: new trends in therapy, John Libbey Eurotext, London, pp 197
Huang S-Z, Ren Z-R, Chen M-J, Xu H-P, Zeng Y-T, Rodgers GP (1994) Treatment of β-thalassemia with hydroxyurea (HU)-Effects of HU on globin gene expression. Sci China B 37:1350–1359
Chang SS, Boehm CD, Higgs DR, Cutting GR (2000) Single -tube multiplex-PCR screen for common determinants of β-thalassemia. Blood 95:360–362
Winichagoon P, Saechan V, Sripanich R, Nopparatana C, Kanokpongsakdi S, Maggio A, Fucharoen S (1999) Prenatal diagnosis of β-thalassemia by reverse dot blot hybridizaion. Prenatal Diag 19:428–435
Choi I, Muta K, Wickrema A, Krantz SB, Nishimura J, Nawata H (2000) Interferon gamma delays apoptosis of mature erythroid progenitor cells in the absence of erythropoietin. Blood 95:3742–3749
Matsushima T, Nakashima M, Oshima K, Abe Y, Nishimura J, Nawata H, Watanabe T, Muta K (2001) Receptor binding cancer antigen expressed on SiSo cells, a novel regulator of apoptosis of erythroid progenitor cells. Blood 98:313–321
Sawada K, Krantz SB, Kans JS, Dessypris EN, Sawyer S, Glick AD, Civin CI (1987) Purification of human erythroid colony-forming units and demonstration of specific binding of erythropoietin. J Clin Invest 80:357–366
Muta K, Krantz SB (1993) Apoptosis of human erythroid colony-forming cells is decreased by stem cell factor and insulin like growth factor I as well as erythropoietin. J Cell Physiol 156:264–271
Sui X, Krantz SB, Zhao Z (1997) Identification of increased protein tyrosine phosphatase activity in polycythemia vera erythroid progenitor cells. Blood 90:651–657
Sui X, Krantz SB, Zhao Z (2000) Stem cell factor and erythropoietin inhibit apoptosis of human erythroid progenitor cells through different signalling pathways. Br J Haematol 110:63–70
Dover GJ, Boyer SH (1980) Quantitation of hemoglobins within individual red cells: asynchronous biosynthesis of fetal and adult hemoglobin during erythroid maturation in normal subjects. Blood 56:1082–1091
Wood WG, Jones RW (1981) Erythropoiesis and hemoglobin production: a unifying model involving sequential gene activation. In: Stamatoyannopoulos G, Nienhuis AW (eds) Hemoglobins and Development in Differentiation, Alan R Liss Inc, New York, pp 243–261
Papayannopoulou Th, Kalmantis T, Stamatoyannopoulos G (1979) Cellular regulation of hemoglobin switching: evidence for inverse relationship between fetal hemoglobin synthesis and degree of maturity of human erythroid cells. Proc Natl Acad Sci USA 76:6420–6424
Chomczynski P (1993)A reagent for the single-step simultaneous isolation of RNA, DNA and proteins from cell and tissue samples. Biotechniques 15:532–537
Watanapokasin Y, Winichagoon P, Fucharoen S, Wilairat P (2000) Relative quantitation of mRNA in β-thalassemia/HbE using real-time polymerase chain reaction. Hemoglobin 4:105–116
Winichagoon P, Fucharoen S, Wilairat P, Cihara K, Fukumaku Y (1995) Role of alternatively spliced beta E-globin mRNA on clinical severity of beta-thalassemia/hemoglobin E disease. Southeast Asian J Trop Med Public Health 26(S1):241–245
Winichagoon P., Fucharoen S, Chen P, Wasi P (2000) Genetic Factors Affecting Clinical Severity in Thalassemia Syndromes. J Pediatr Hematol Oncol 22:573–580
Fibach E, Manor D, Oppenheim A, Rachmilewitz EA (1989) Proliferation and maturation of human erythroid progenitors in liquid culture. Blood 73:100–103
Fibach E, Manor D, Treves A, Rachmilewitz EA (1991) Growth of normal erythroid progenitors in liquid culture: a comparison with colony growth in semisolid culture. Int J Cell Cloning 9:57–64
Hopp C, Vichinsky E, Lewis B, Foote D, Styles L (1999) Hydroxyurea and sodium phenylbutyrate therapy in thalassemia intermedia. Am J Hematol 62:221–227
Rodgers GP, Rachmilewitz EA (1995) Novel treatment options in the severe β-globin disorder. Br J Haematol 91:263–268
Atweh GF, Sutton M, Nassif I, Boonsaild V, Dover GJ, Wallenstein S, Wright E, McMahon L, Stamatoyannopoulos G, Faller DV, Perrine SP (1999) Sustained induction of fetal hemoglobin by pulse butyrate therapy in sickle cell disease. Blood 93:1790–1797
Rodgers GP, Rachmilewitz EA (1995) Novel treatment options in the severe β-globin disorder. Br J Haematol 91:263–268
Zeng YT, Huang SZ, Ren ZR, Lu ZH, Zeng FY, Schechter AN, Rodgers GP (1995) Hydroxyurea therapy in β-thalassemia intermedia: improvement in haematological parameters due enhanced β-globin synthesis. Br J Haematol 90:557–563
Janes SM, Cunningham JM (1998) Understanding fetal globin gene expression: a step towards effective HbF reactivation in haemoglobinopathies. Br J Hematol 102:415–422
Smith RD, Constance JL, Noguchi T, Schechter AN (2000) Quantitative PCR analysis of HbF inducers in primary human adult erythroid cells. Blood 95:863–869
Acknowledgement
This work was supported by The Thailand Research Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Watanapokasin, R., Sanmund, D., Winichagoon, P. et al. Hydroxyurea responses and fetal hemoglobin induction in β-thalassemia/HbE patients’ peripheral blood erythroid cell culture. Ann Hematol 85, 164–169 (2006). https://doi.org/10.1007/s00277-005-0049-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-005-0049-1