Abstract
Objective
Anatomic variations have curicial importance during neck surgery. We present a fenestrated internal jugular vein variation and the accessory nerve passing through it. Also, we discuss preoperative diagnosis of this variation using ultrasonography.
Method
The possible recognition of this variation by ultrasonography is introduced.
Results
The accessory nerve in an internal jugular vein fenestration can be seen using ultrasonography.
Conclusion
Preoperative identification of this rare variation may secure surgeon from potential complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neck dissections are performed in order to resect cervical lymph nodes. According to Robbin’s classification, neck lymph nodes are divided into seven groups. Level 2 represents the superior jugular group, involving the internal jugular vein (IJV), accessory nerve (AN), carotid artery, vagus nerve, and hypoglossal nerve. Anatomic structures must be identified and preserved to perform dissections adequately and also to avoid morbidity and mortality. The IJV and AN have a close and variable interaction at the mediosuperior side of level 2. Instead of encountering a dangerous situation during surgery, it is better to recognize these variations preoperatively.
Therefore, we aimed to discuss a rare anatomic variation in the light of the literature and the possibility of its preoperative diagnosis.
Case report
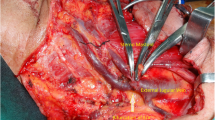
A 72-year-old male patient was admitted to our clinic with a T4N0M0 transglottic squamous cell larynx carcinoma. Total laryngectomy and bilateral neck dissection was performed. During a left level 2 dissection, a variation between the AN and IJV was observed (Fig. 1). In hope of obtaining information, the patient’s neck magnetic resonance images were reinvestigated in the operating room. However, there was no informative image related to the variation. With careful dissection, a variation of an IJV fenestration with the AN passing through was identified.
Encountering of such a variation without preoperative knowledge is stressful and hard to recognize from magnetic resonance and computed tomography. Therefore, with the hope of learning new information, we performed ultrasound imaging on the postoperative 20th day. From the ultrasonographic investigation, images showing AN echogenicity passing through the IJV were identified (Fig. 2).
Discussion
Neck dissections have been performed for nearly a century. It has been shown that neck lymphatics can be cleaned without excising the IJV, AN, and sternocleidomastoid muscle, and without compromising oncologic principles. Therefore, anatomic structures, their interactions, and variations gained more importance.
Saman et al. investigated the IJV and AN relation at the anterior triangle through a cadaveric study and found that the AN was located anterior to the IJV in 80% of cases, posterior in 19%, and in one case it pierced the IJV (1%) [1]. Surgical dissection studies by Taylor et al., Lee et al., and Hashimato et al. showed similar ratios as 1%, 2.8%, and 3.3%, respectively [3, 4, 9]. Contrera et al. identified a 1% (3/295) IJV variation rate [1]. Mumtaz et al. reviewed IJV variations, and they found 16 fenestration from 1197 cases [5]. Also, the AN does not always pass through fenestrations [2, 6, 8].
Although there are some theories about embryological basis of this variation, none of the them is enough to explain all reported cases. Vascular theory is the most accepted one. According to vascular theory, precardinal veins develops before nerve and capillary plexus posterior to IJV may cause venous duplication [3].
In the literature, diagnosis of variations by imaging modalities is rarely discussed. One of the three variations that Contrera et al. showed was a large duplication case that could only be detected preoperatively [1]. Also, Pegot et al. detected a fenestration in their retrospective analysis [6]. Sanchez et al. mentioned that variations could not be detected using CT [8]. Hashimato et al. mentioned that they visualized IJV fenestrations using contrasted CT [3]. Also, two fenestration cases were detected using CT angiography by Towbin and Kanal [10].
It has been clearly shown that IJV variations, either duplication or fenestration, have crucial importance regardless of whether the AN passes through or not. The literature reveals that this variation has life-threatening potential. Therefore, it is vital to identify this variation preoperatively. However, detecting small-sized fenestrations with contrasted MRI or contrasted CT is very difficult.
As is known, ultrasonography is an easy, cheap, radiation-free, and reproducible imaging modality frequently used in the head and neck region. We hypothesized that ultrasonographic imaging could be helpful for detecting variations of IJV fenestrations and the AN passing through. In ultrasound imaging, entrance of the AN into the fenestration could be seen as a density in the IJV. This image is easily recognizable by radiologists and also the echogenicity could be identified with Doppler ultrasonography.
Conclusion
As a result, because of the variations, AN dissection should not be performed before IJV dissection. Also, it is possible to recognize the variation of fenestration through an ultrasonographic investigation. Close working between surgeons and radiologists has a crucial role in the cautious approach.
Prospective controlled trials are required to understand the value and potency of ultrasonography for the detection of IJV fenestrations.
References
Contrera KJ, Aygun N, Ward BK, Gooi Z, Richmon ZD (2016) Internal jugular vein duplication and fenestration: case series and literature review. Laryngoscope 126:1585–1588
Cvetko E (2015) Unilateral fenestration of the internal jugular vein: a case report. Surg Radiol Anat 37:875–877
Hashimato Y, Otsuki N, Morimoto K, Saito M, Nibu K (2011) Four cases of spinal accessory nerve passing through the fenestrated internal jugular vein. Surg Radiol Anat 34:373–375
Lee SH, Lee JK, Jin SM, Kim JH, Park S, Chu HR, Ahn HY, Rho YS (2009) Anatomical variations of the spinal accessory nerve and its relevance to level IIb lymph nodes. Otololaryngol Head Neck Surg 141:639–644
Mumtaz S, Singh M (2019) Surgical review of the anatomical variations of the internal jugular vein: an update for head and neck surgeons. Ann R Coll Surg Engl. https://doi.org/10.1308/rcsann.2018.0185
Pegot A, Guichard B, Peron JM, Trost O (2015) Empty fenestration of the internal jugular vein: a rare phenomenon. Br J Oral Maxillofac Surg 53:78–80
Saman M, Etebari P, Pakdaman MN, Urken ML (2011) Anatomic relationship between the spinal accessory nerve and the jugular vein: a cadaveric study. Surg Radiol Anat 33:175–179
Sanchez MM, Vila CH, Garcia RG. Monje F (2015) Fenestrated internal jugular vein: a rare finding in neck dissection. Int J Oral Maxillofac Surg 44:1086–1087
Taylor CB, Boone JL, Schmalbach CE, Miller FR (2013) Intraoperative relationship of the spinal accessory nerve to the internal juguler vein: variation from cadever studies. Am J Otolaryngol 34:527–529
Towbin AJ, Kanal E (2004) A review of two cases of fenestrated internal jugular veins as seen by CT angiography. AJNR Am J Neuroradiol 25:1433–1434
Funding
None.
Author information
Authors and Affiliations
Contributions
MAA: Protocol/project development, Data collection, Data analysis, Manuscript writing, BMŞ: Protocol/project development, Data collection, Data analysis, BO: Data collection, Data analysis, Manuscript writing, RT: Protocol/project development, Data collection, Data analysis, GS: Protocol/project development, Data collection, Data analysis, Manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abakay, M.A., Şimşek, B.M., Olgun, B. et al. Ultrasonic identification of internal jugular vein fenestration. Surg Radiol Anat 41, 1079–1081 (2019). https://doi.org/10.1007/s00276-019-02226-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-019-02226-7