Abstract
Purpose
The aim of this study was to analyze the impact of using intra-procedural pre-ablation contrast-enhanced CT prior to percutaneous thermal ablation (pre-ablation CECT) of colorectal liver metastases (CLM) on local outcomes.
Materials and Methods
This retrospective analysis of a prospectively collected liver ablation registry included 144 consecutive patients (median age 57 years IQR [49, 65], 60% men) who underwent 173 CT-guided ablation sessions for 250 CLM between October 2015 and March 2020. In addition to oncologic outcomes, technical success was retrospectively evaluated using a biomechanical deformable image registration software for 3D-minimal ablative margin (3D-MAM) quantification. Bayesian regression was used to estimate effects of pre-ablation CECT on residual unablated tumor, 3D-MAM, and local tumor progression-free survival (LTPFS).
Results
Pre-ablation CECT was acquired in 71/173 (41%) sessions. Residual unablated tumor was present in one (0.9%) versus nine tumors (6.6%) ablated with versus without using pre-ablation CECT, respectively (p = 0.024). Pre-ablation CECT use decreased the odds of residual disease on first follow-up by 78% (CI95% [5, 86]) and incomplete ablation (3D-MAM ≤ 0 mm) by 58% (CI95% [13, 122]). The odds ratio for residual unablated tumor for larger CLM was lower when pre-ablation CECT was used (odds ratio 1.0 with pre-ablation CECT vs. 2.52 without). Pre-ablation CECT use was not associated with improvements on LTPFS.
Conclusions
Pre-ablation CECT is associated with improved immediate outcomes by significantly reducing the incidence of residual unablated tumor and by mitigating the risk of incomplete ablation for larger CLM. We recommend performing baseline intra-procedural pre-ablation CECT as a standard imaging protocol.
Level of evidence
Level 3 (retrospective cohort study).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Percutaneous thermal ablation for patients with colorectal liver metastasis can be performed alone or in conjunction with resection as long as all visible disease can be eradicated according to the guidelines of the European Society for Medical Oncology [1]. These procedures are most commonly performed under ultrasound or computed tomography (CT) imaging guidance. CT provides user-independent multiplanar cross-sectional imaging and is available in most health care centers. Moreover, with the rise of image fusion, ablation confirmation software, and stereotactic and robotic guidance technologies, CT is becoming the standard imaging modality for ablation guidance in many centers [2]. Despite the acknowledgment of CT as the optimal image-guidance modality for liver ablation, large parts of the image-guidance technique are not standardized which might contribute to wide variations in local tumor progression (LTP) rates [3].
Of all the factors known to be associated with LTP following percutaneous ablation of colorectal liver metastases (CLM) [3,4,5], the 3D-minimal ablative margin (3D-MAM) is the only modifiable factor during an ablation procedure. Complete ablation with sufficient margin, usually defined as ablation with a circumferential tumor-free margin of at least 5 mm [6], has been shown to be a strong predictor of LTP-free survival (LTPFS) [5, 7, 8]. To achieve and confirm 3D-MAM, it is important to clearly visualize the location and size of the tumor as well as the ablation zone, which requires contrast-enhanced CT (CECT) imaging. Intra-procedural CECT imaging can serve two distinct functions: pre-ablation for accurate depiction of tumor location and size; post-ablation for immediate ablation zone assessment. While CECT is recommended for procedure planning and ablation margin assessment [2], there is no clear evidence whether these images should be acquired intra-procedurally or peri-procedurally.
We hypothesize that the use of pre-ablation CECT in CT-guided thermal ablation of CLM prior to the ablation improves technical success and short-term oncological outcomes. The primary endpoint of this study was residual tumor at first imaging follow-up. Secondary endpoints were minimum ablative margins and LTPFS.
Materials and Methods
Study Population
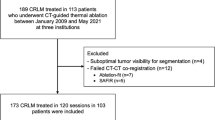
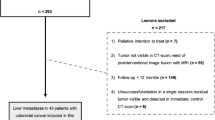
This was a single-institution retrospective review of a prospectively maintained liver ablation registry, approved by the institutional review board with a waiver of informed consent. The analysis included 173 consecutive CT-guided thermal ablation procedures performed between December 2015 and March 2020 for a total of 250 locoregional treatment naïve CLM in 144 patients (60% men; median age, 57 years [range, 32–84]). Selection criteria are presented in the flowchart in Fig. 1. This study was conducted according to the STROBE guidelines [9].
Intra-procedural pre-ablation CECT was defined as acquisition of a CECT image by the injection of intravenous contrast media immediately before placement of the ablation probe. Intra-procedural post-ablation CECT was defined as acquisition of at least one CECT image by the injection of intravenous contrast media immediately after ablation to evaluate completeness of ablation.
Procedure
Patients were eligible for percutaneous ablation of CLM if they had ≤ 5 CLM, measuring ≤ 5 cm each. All procedures were performed with curative-intent, under CT imaging-guidance, and the goal of completely ablating each CLM with a least ≥ 5 mm margin [10, 11]. However, during the study period there was no consensus regarding the use of specific software for intra-procedural margin assessment. All ablations were performed by one of nine board-certified interventional radiologists with 6–13 years of experience, with the patient under general anesthesia and breath hold during imaging acquisition. Administration of contrast media during pre- and/or post-ablation CT image acquisition was at the interventional radiologist’s discretion. Ablations were performed with radiofrequency (Cool-tip radiofrequency ablation system; Covidien, Boulder, Colorado, USA) or microwave (Certus probe, Certus 140 2·4-GHz microwave ablation system; NeuWave, Madison, Wisconsin, USA) according to the operator’s choice.
CECT Imaging Protocol
Until 2019, intra-procedural CECT for ablation planning was performed with no standard protocol in place. In early 2019, a standard protocol for dual phase CECT (arterial and portal venous phases) for ablation planning was developed and implemented across our operation (Supplementary Table 1). However, the use of contrast media was still at the interventional radiologist’s discretion.
Imaging Follow-up and Assessment
Imaging assessment was performed independently by two radiologists with 5 and 13 years of experience, and discrepancies in interpretation were resolved by consensus. Imaging-based assessment of oncologic outcomes was carried out independently from collection of clinical and procedural information (e.g., use of intra-procedural CECT). The initial post-ablation cross-sectional imaging assessment was performed within 2–8 weeks after ablation. Further assessments were performed as standard practice using CECT, positron emission tomography, or magnetic resonance imaging until death or loss to follow-up per our institutional practice [12].
To describe ablation endpoints, standardized terminology and reporting criteria were employed [12, 13]. Residual unablated tumor was defined as tumor foci within or at the edge of the ablation margin on the first cross-sectional imaging follow-up. LTPFS was defined as the time between the ablation and the first appearance of tumor foci within or at the edge of the ablation zone on cross-sectional imaging follow-up, or the last imaging follow-up.
Clinical Data Collection and Minimum Ablative Margin Analysis
Baseline characteristics, RAS mutation status, and laboratory values (within 45 days prior to ablation) for each patient were collected from the electronic medical records. The estimated glomerular filtration rate (eGFR) was collected within 90 days prior to ablation (eGFR before) and between 20 and 90 days after ablation (eGFR after). Procedural characteristics (e.g. tumor size, location, immediate complications) were retrieved from a structured report of each CT-guided ablation procedure. Tumors were categorized as perivascular if < 10 mm from a vessel ≥ 3 mm in diameter and subcapsular if < 10 mm from the liver capsule. The 3D-MAM was calculated retrospectively using biomechanical deformable image registration (DIR) software [14]. For this analysis, 3D-MAM ≤ 0 mm was defined as unsuccessful ablation (A2), 3D-MAM > 0 and < 5 mm as suboptimal ablation (A1) and 3D-MAM ≥ 5 mm as optimal ablation (A0) measured by DIR software. Details are described in Appendix I.
Statistical Analysis
For binary outcomes, Bayesian logistic regression was used to estimate effects pre-ablation CECT and tumor diameter on residual unablated tumor and technical success (A0 ablation). Potential confounders of anatomical location (i.e., left vs. right lobe, perivascular, subcapsular location, or operator) were adjusted for. Bayesian Cox proportional hazards regression was used to estimate effects of tumor diameter and use of pre-ablation CECT on LTPFS. Potential confounders of < 5 mm 3D-MAM and RAS mutation were controlled for. Right censoring was used when no event occurred during the follow-up period. Interaction terms were modeled and visualized with plots of conditional effects. Both analyses were conducted on a tumor level with the procedure as random effect to account for multiple measurements of pre-ablation CECT. Cumulative incidence curves were estimated on a procedure level and compared using the log-rank test with Bonferroni correction. Pre-ablation tumor growth was estimated using linear regression and is described in Supplementary Material 2.
In the descriptive statistics, Fisher’s exact and Kruskal–Wallis test were used to compare proportions and continuous baseline characteristics, respectively. Statistical significance in the regression analyses was defined as probability of direction (pd) > 97.5% and % in region of practical equivalence (ROPE) < 5% [15]. High-density intervals (HDI) were used to report 95% credible intervals (CI95%). All statistical analyses were performed using R (R Foundation for Statistical Computing, Vienna, Austria) and RStudio. Bayesian analysis was performed using the brms package [16] (v2.16.1) with weakly informative priors (\(\sim Normal(0, 2.5\))) [17]. Plots were created using ggplot2 (v3.3.5) and ggpubr (v0.4.0) [18, 19]. The code for the statistical analysis can be found in the supplementary materials.
Results
Table 1 shows the procedure-level and tumor-level characteristics of the groups with and without administration of contrast media in pre-ablation CT. The median time interval between the last diagnostic CECT and the ablation procedure (32 days, IQR = [21, 41.5] vs 28 days, IQR = [18.3, 39.5]: p = 0.4) and the median follow-up time (20.1 months, IQR = [13.3, 30.0] vs. 24.6 months, IQR = [15.0, 36.3]; p = 0.072) were not different between groups. In this cohort, residual tumor and LTP occurred in 10 (4%) and 32 (12.8%) ablated tumors, respectively.
The only significant differences between the procedures with and without pre-ablation CECT were the proportion of multiple CLM (p = 0.038) and the tumor locations (bilobar/left lobe vs. right lobe; p = 0.028), which were more frequent among the procedures where pre-ablation CECT was acquired. The frequency of pre-ablation CECT acquisition did not change significantly after the introduction of the standardized ablation specific CT protocol in early 2019 (38.6% vs 44.4%; p = 0.4). The proportion of CLM with < 5 mm 3D-MAM did not differ between the ablations with and without pre-ablation CECT(57.3% vs 57.4%; p > 0.9). There was one operator who performed 50% of the procedures who had a preference for acquiring pre-ablation CECT compared to the other operators (57% vs. 25.3%; p < 0.001) (Table 2). However, there was no difference in the rate of residual unablated tumor (5.8% vs. 4.6%; p = 0.7), 0 mm 3D-MAM (24.0% vs. 16.9%; p = 0.3), or < 5 mm 3D-MAM (69.7% vs. 67.5%; p = 0.8).
Effect of Pre-ablation CECT on Residual Unablated Tumor
For residual tumor at the first follow-up, the odds ratio (OR) with pre-ablation CECT use was 0.22 (CI95% [0.05, 0.86], pd = 98.7%, 0.3% in ROPE) and the OR per cm increased tumor size was 2.02 (CI95% [1.02, 4.2], pd = 97.1%, 4.7% in ROPE). The full model outputs with all covariates are available in Supplementary Material 1.
In the interaction model (Fig. 2, top), the ORs per cm increase in tumor size were 1.0 (CI95% [0.32, 2.71], pd = 50.2%, 28.1% in ROPE) and 2.52 (CI95% [1.15, 5.39], pd = 98.7%, 0.7% in ROPE) when pre-ablation CECT was used versus not used, respectively.
Effect of Pre-ablation CECT on LTPFS
There was no significant effect of pre-ablation CECT use on LPTFS after adjusting for A0 ablation (3D-MAM ≥ 5 mm) and RAS mutation status. In the interaction model, the hazard ratios for LTPFS per cm increase in tumor size were 2.2 (CI95% [1.05, 5.15], pd = 98.3%, 0.8% in ROPE) and 3.2 (CI95% [1.48, 7.79], pd ≥ 99.9%, ≤ 0.1% in ROPE) when pre-ablation CECT was used versus not used, respectively.
There was a significant difference in the cumulative incidence of LTP in the subgroup without pre-ablation CECT between A1/A2 (3D-MAM < 5 mm) versus A0 ablation (3D-MAM ≥ 5 mm) (p < 0.001) (Fig. 3, left). Further, there was a significant difference in the cumulative incidence of LTP in the subgroup without pre-ablation CECT between ≥ 2 cm and < 2 cm tumor size (p = 0.028) (Fig. 3, right). The full model outputs with all covariates are available in Supplementary Material 1.
Effect of Pre-ablation CECT on 3D-MAM
The OR for A2 ablation (3D-MAM ≤ 0 mm) was 0.42 (CI95% [0.13, 1.22], pd = 95.1%, 3.8% in ROPE) with pre-ablation CECT use and 2.41 (CI95% [1.28, 89], pd = 99.7%, ≤ 0.1% in ROPE) per cm increase in tumor size. In the interaction model (Fig. 2, middle), the ORs for A2 ablation per cm increase in tumor size were 1.81 (CI95% [0.89, 3.56], pd > 95.9%, 5.4% in ROPE) and 3.12 (CI95% [1.62, 7.81], pd > 99.9%, < 0.1% in ROPE) with versus without pre-ablation CECT use, respectively.
Relevantly, there were no significant effects of pre-ablation CECT on the ability of achieving an A0 ablation (≥ 5 mm 3D-MAM) (Fig. 2, bottom). The full model outputs with all covariates are available in Supplementary Material 1.
Immediate Complications and Effect on Kidney Function
The overall complication rates were 5.6 and 4.9% in the procedures with and without pre-ablation CECT, respectively. No immediate contrast media-related complications were reported. Further, eGFR levels dropped from > 60 mL/min/1.73 m2 to < 60 mL/min/1.73 m2 in 6 patients after a procedure without pre-ablation CECT and in 1 patient after a procedure with pre-ablation CECT (Table 1).
Discussion
This study shows the benefit of the intravenous administration of contrast media in pre-ablation CT during percutaneous CT-guided ablation of CLM. From a risk/benefit standpoint, administering contrast media in pre-ablation CT seems justified as it was associated with a 78% relative and a 5.7% absolute risk reduction of residual unablated tumor at the first imaging follow-up. Additionally, the inherent increased risk of residual tumor associated with larger CLM was eliminated by the use of contrast media in pre-ablation CT (OR 1.0 vs. 2.52 per cm increase in tumor size with vs. without pre-ablation CECT, respectively). This effect is mainly driven by similarly 58% decreased odds of having A2 ablation (3D-MAM = 0 mm) as measured by DIR software and potentially increased tumor size since the last diagnostic imaging (Fig. 4, Supplementary Fig. 1). Both highlight the importance of administrating contrast media in pre-ablation CT for proper tumor size depiction and adequate procedure planning. Looking beyond the first imaging follow-up, our analysis showed that the pre-ablation CECT did not have a significant effect on LTPFS after controlling for A0 ablation (3D-MAM ≥ 5 mm). This underscores the importance of ablation confirmation software to improve 3D-MAM and, potentially, reduce long-term LTP rates. To date, such potential benefit of ablation confirmation software has only been shown in retrospective series [21, 22].
A 68 old male with colorectal liver metastasis, received a contrast-enhanced CT 50 days before the ablation procedure ablation where the tumor (arrowhead) measured 17 mm (A). Immediately prior to the ablation the patient received a non-contrast CT (B) where the tumor was not clearly visible and a contrast-enhanced CT with the tumor measured 29 mm (C). The post-ablation contrast-enhanced CT shows complete coverage of the tumor (D)
The incidence of complications was not significantly different among the groups with and without use of contrast media in pre-ablation CT (5.6% and 4.9%, respectively; p > 0.9), and the observed complications were not caused by the additional CECT scan or contrast media dose. Most importantly, our longitudinal study of eGFR did not demonstrate significant changes in overall renal function in either patient cohort.
This study has limitations arising from its retrospective nature. The choice of whether to acquire pre-ablation CECT scans immediately before the ablation was made by the performing interventional radiologist. Based on the available data, it seems that pre-ablation CECT was acquired for potentially more challenging procedures (e.g., patients with multiple or left-sided/bilobar CLM). Further, it could be that pre-ablation CECT acquisition was associated with more extensive procedure planning, which led to better short-term outcomes. In this case, the causal effect would be due to improved planning rather than the CECT alone, which we cannot assess retrospectively. During the follow-up period, different imaging modalities were used which have different sensitivity for detection of progressive disease. However, the primary endpoint of residual disease is most likely accurately captured with any of those imaging modalities. Further, the effect of intra-procedural post-ablation CECT could not be analyzed since this was done in almost all cases during the study period. Such an analysis would allow us to evaluate when contrast media administration would be more beneficial in patients who can only tolerate a limited dose. However, based on the analysis of eGFR, only a small proportion of patients could not receive contrast media due to limited renal function.
In conclusion, pre-ablation CECT led to improved immediate local tumor control by significantly reducing the rates of residual tumor. Based on our findings, we recommend performing baseline intra-procedural pre-ablation CECT as a standard procedure. The lack of effect of contrast media use on pre-ablation CT on LTPFS might be a consequence of its use not being able to increase 3D-MAMs to ≥ 5 mm, for which ablation confirmation software packages are required for accurate quantitative evaluation, which is being currently evaluated by ongoing clinical trials [23].
References
Van Cutsem E, Cervantes A, Adam R, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27(8):1386–422.
Gillams A, Goldberg N, Ahmed M, et al. Thermal ablation of colorectal liver metastases: a position paper by an international panel of ablation experts, the interventional oncology sans frontieres meeting 2013. Eur Radiol. 2015;25(12):3438–54.
Lin YM, Paolucci I, Brock KK, Odisio BC. Image-guided ablation for colorectal liver metastasis: principles, current evidence, and the path forward. Cancers. 2021;13(16):3926.
Peng S, Huang P, Yu H, et al. Prognostic value of carcinoembryonic antigen level in patients with colorectal cancer liver metastasis treated with percutaneous microwave ablation under ultrasound guidance. Medicine. 2018;97(10): e0044.
Shady W, Petre EN, Gonen M, et al. Percutaneous radiofrequency ablation of colorectal cancer liver metastases: factors affecting outcomes–a 10-year experience at a single center. Radiology. 2016;278(2):601–11.
Shady W, Petre EN, Do KG, et al. percutaneous microwave versus radiofrequency ablation of colorectal liver metastases: ablation with clear margins (A0) provides the best local tumor control. J Vasc Interv Radiol. 2018;29(2):268-275 e261.
Calandri M, Yamashita S, Gazzera C, et al. Ablation of colorectal liver metastasis: interaction of ablation margins and RAS mutation profiling on local tumour progression-free survival. Eur Radiol. 2018;28(7):2727–34.
Han K, Kim JH, Yang SG, et al. A single-center retrospective analysis of periprocedural variables affecting local tumor progression after radiofrequency ablation of colorectal cancer liver metastases. Radiology. 2021;298(1):212–8.
Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12(12):1500–24.
Solbiati L, Ahmed M, Cova L, Ierace T, Brioschi M, Goldberg SN. Small liver colorectal metastases treated with percutaneous radiofrequency ablation: local response rate and long-term survival with up to 10-year follow-up. Radiology. 2012;265(3):958–68.
Sofocleous CT, Petre EN, Gonen M, et al. CT-guided radiofrequency ablation as a salvage treatment of colorectal cancer hepatic metastases developing after hepatectomy. J Vasc Interv Radiol. 2011;22(6):755–61.
Ahmed M, Solbiati L, Brace CL, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria–a 10-year update. J Vasc Interv Radiol. 2014;25(11):1691-1705 e1694.
Puijk RS, Ahmed M, Adam A, et al. consensus guidelines for the definition of time-to-event end points in image-guided tumor ablation: results of the SIO and DATECAN initiative. Radiology. 2021;301(3):533–40.
Anderson BM, Lin YM, Lin EY, et al. A novel use of biomechanical model-based deformable image registration (DIR) for assessing colorectal liver metastases ablation outcomes. Med Phys. 2021;48(10):6226–36.
Makowski D, Ben-Shachar MS, Chen SHA, Ludecke D. Indices of effect existence and significance in the bayesian framework. Front Psychol. 2019;10:2767.
Bürkner P-C. Brms: an r package for bayesian multilevel models using stan. J Stat Softw. 2017;80:1.
Gelman A, Hill J, Vehtari A, Regression and other stories, 2020
Alboukadel Kassambara , ggpubr: 'ggplot2' Based Publication Ready Plots 2020
Wickham H. ggplot2: elegant graphics for data analysis. New York: Springer-Verlag; 2016.
Media ACoDaC (2021) ACR Manual on Contrast Media
Ruiter SJS, Tinguely P, Paolucci I, et al. (2021) 3D quantitative ablation margins for prediction of ablation site recurrence after stereotactic image-guided microwave ablation of colorectal liver metastases: a multicenter study. Front Oncol. 2021 ;11
Laimer G, Jaschke N, Schullian P, et al. Volumetric assessment of the periablational safety margin after thermal ablation of colorectal liver metastases. Eur Radiol. 2021;31(9):6489–99.
Lin YM, Paolucci I, Anderson BM, et al. Study protocol COVER-ALL: clinical impact of a volumetric image method for confirming tumour coverage with ablation on patients with malignant liver lesions. Cardiovasc Intervent Radiol. 2022;45:1860–1867. https://doi.org/10.1007/s00270-022-03255-3
Anderson BM, Lin EY, Cardenas CE, et al. Automated contouring of contrast and noncontrast computed tomography liver images with fully convolutional networks. Adv Radiat Oncol. 2021;6:100464.
Acknowledgements
We thank Stephanie Deming, Research Medical Library, MD Anderson Cancer Center, for editing the manuscript
Funding
Iwan Paolucci is funded by a PostDoc Mobility fellowship from the Swiss National Science Foundation under Project Nr P2BEP3_195444. Research reported in this publication was supported in part by the National Cancer Institute of the National Institutes of Health under award number R01CA235564 and P30CA016672, and the Image Guided Cancer Therapy Research Program at The University of Texas MD Anderson Cancer Center.
Author information
Authors and Affiliations
Contributions
IP and BCO: Study design; IP, YML, and BCO: Writing and editing; IP, YML, AKJ, and BCO: Data collection and data review; IP: Statistical analysis; IP, YML, AKJ, KKB, and BCO: Critical review and editing; BCO: Supervision of the project. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Bruno Odisio received grants from Siemens Healthineers, which were not related to this manuscript. The other authors declare no conflict of interest.
Ethical Approval
For this type of study, formal consent is not required. This study was approved by the local IRB under protocol Nr: 2021-0340.
Informed Consent
This study has obtained IRB approval from the local IRB of the University of Texas MD Anderson Cancer Center, and the need for informed consent was waived.
Consent for Publication
For this type of study, consent for publication is not required.
Presentation at SIR scientific meeting
An abstract of the presented work was presented at the annual scientific meeting of the Society of Interventional Radiology 2022 in Boston under the title “The added value of intra-procedural contrast enhanced CT prior to thermal ablation of colorectal liver metastasis”.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
270_2022_3333_MOESM4_ESM.pdf
Supplementary Figure 1: Tumor growth between last diagnostic CECT and ablation where CECT was available for both. (PDF 11 KB)
Appendix
Appendix
To calculate the 3-dimensional minimum ablative margin (3D-MAM) retrospectively, the last diagnostic CECT image preceding the ablation procedure and, if available, the intra-procedural pre-ablation and post-ablation CECT images were sent to an image processing software (RayStation 10B, RaySearch Laboratories, Sweden). The liver, tumor, and ablation zone were segmented using a custom-built artificial intelligence segmentation algorithm [24] and reviewed and corrected by a trained engineer (IP) and a radiologist (YML). The images were registered using biomechanical deformable image registration (DIR). The 3D-MAM was calculated as the closest Euclidean distance between the ablation and the mapped tumor contour [14]. For this analysis, 3D-MAM = 0 mm was defined as unsuccessful ablation (A2), 3D-MAM > 0 and < 5 mm as suboptimal ablation (A1) and 3D-MAM ≥ 5 mm as optimal ablation (A0) measured by DIR software.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Paolucci, I., Lin, YM., Jones, A.K. et al. Use of Contrast Media During CT-guided Thermal Ablation of Colorectal Liver Metastasis for Procedure Planning is Associated with Improved Immediate Outcomes. Cardiovasc Intervent Radiol 46, 327–336 (2023). https://doi.org/10.1007/s00270-022-03333-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-022-03333-6