Abstract
Background and Purpose
To describe our first experience using a small stent retriever specifically designed for thrombectomy in cerebral arteries with a small caliber (Acandis APERIO® 3.5/28) in patients with acute ischemic stroke.
Materials and Methods
All patients with an acute ischemic stroke, who underwent endovascular recanalization using the APERIO® thrombectomy device with a diameter of 3.5 mm, were identified in retrospect and included in the present analysis. Demographic and clinical data as well as data on the procedures performed were collected (patient sex, mean age, NIHSS, mRS, TICI score, and complications).
Results
Stent retriever-based thrombectomy with the Aperio® 3.5/28 alone (n = 10 vessels) or in combination with other devices (n = 13 vessels) was performed in 22 acute stroke patients with embolic occlusions of distal branches of the anterior and posterior circulations (median NIHSS = 8.5). For vessels treated with the Aperio® 3.5/28, we achieved a TICI 2b/3 reperfusion rate of 73.9%. One patient suffered a symptomatic intracerebral hemorrhage after thrombectomy; otherwise, no procedure-related complications were seen.
Conclusion
Our data suggest that mechanical thrombectomy of distal cerebral artery occlusions with the Aperio® 3.5/28 is feasible and in general safe, thus offering a promising option for endovascular stroke therapy. However, multicentric studies with larger patient cohorts are necessary to evaluate the clinical benefit.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Five recently published randomized clinical trials have shown that endovascular thrombectomy for patients presenting with acute ischemic stroke is superior to best medical treatment alone [1,2,3,4,5,6]. The trials focused on proximal large vessel occlusion of the anterior circulation, particularly the distal internal carotid artery (ICA) and the proximal middle cerebral artery (MCA) in the M1-Segment. However, occlusion of distal cerebral arteries including the second-order branches (M2) of the MCA, pericallosal artery, or posterior cerebral artery (PCA) can also lead to disabling ischemic strokes, depending on the eloquence of the dependent territory. The benefit of endovascular treatment of more distal occlusions is uncertain, as concerns have been raised about the procedural safety due to the small caliber, fragility, and tortuous anatomy of peripheral cerebral arteries [1, 7].
Recently, smaller devices for thrombectomy of more distal arteries have been introduced. First promising data have been published, suggesting that endovascular treatment of smaller caliber arteries is feasible and safe and results in high revascularization rates [8,9,10,11,12]. Besides a smaller diameter, the devices for peripheral cerebral arteries need sufficient radial force to integrate the clot and still have to be long enough to cover the thrombus and soft enough to avoid endothelial damage. The stent retriever introduced here is described to be suitable for vessels with a minimum diameter of 1.5 mm, making more distal arteries with a smaller caliber accessible for endovascular treatment.
The purpose of this study is to describe our first experiences using the Aperio® 3.5/28 for stent retriever-based thrombectomy in patients with acute ischemic stroke.
Materials and Methods
Patient Selection
This retrospective case series analysis was approved by the institutional review board. All patients with acute ischemic stroke, who underwent endovascular recanalization procedures using the Aperio® 3.5/28 at our institution, were identified. Demographic and clinical data as well as data on the procedures performed were retrospectively collected. Inclusion criteria for endovascular therapy were an arterial occlusion within the anterior or posterior circulations in CT- or MR angiography and a mismatch between symptoms and ischemic core. In general, patients had no signs of major infarctions according to the Alberta Stroke Program Early CT Score (ASPECTS Score > 5) on CT or MRI, and a baseline National Institute of Health Stroke Scale (NIHSS) Score ≥ 5, fluctuating symptoms or aphasia if the score was < 5. If not contraindicated, patients received intravenous thrombolysis.
Procedure
All interventions were performed on a biplane angiography machine (Artis zee biplane, Siemens Health Care, Forchheim, Germany) under general anesthesia. In general, in case of an occlusion in the anterior circulation, an 8F balloon guide catheter (Cello 8F, Covidien, Irvine, USA) was placed into the ipsilateral internal carotid artery. For patients with a vertebrobasilar occlusion, a 6F (Envoy, Codman, Raynham, MA) guiding catheter was brought in the ipsilateral or dominant vertebral artery. The guiding catheter was continuously flushed with 2.4-mg nimodipine solute in 1000-ml 0.9% saline solution. With or without an additional aspiration catheter (SOFIA 5F, Microvention, Tustin, CA), the clot was subsequently passed with a 0.014-in microwire (Synchro, Stryker Neurovascular, Fremont, CA) and a microcatheter (Rebar 18, Covidien, Irvine, CA). Next, the tip of the microcatheter was placed beyond the distal end of the thrombus. The correct intraluminal positioning of the microcatheter was proven by contrast application via the microcatheter. The Aperio® 3.5/28 was advanced via the microcatheter and the distal marker of the device was positioned at the distal end of the catheter. Then, the microcatheter was pulled back to deploy the device and angiographic runs were performed to evaluate flow restoration. After a waiting period of about 5 min, the device was retrieved in its unfolded state and removed with the microcatheter under continuous manual aspiration using the guiding catheter or/and the intermediate catheter and proximal balloon protection to achieve flow arrest and avoid distal embolization [13]. Again, an angiogram was performed to confirm recanalization. In case of persistent occlusion or incomplete recanalization, the device was recaptured and the procedure was repeated. However, as an orientation, a maximum of three retrievals in the same vessel has been performed on the basis of the SWIFT PRIME trial. Due to the suspected higher risk for dissection and vasospasm of small arteries, the number of retrievals was decided individually for each patient at the discretion of the interventionalist.
The Aperio® 3.5/28 is described as a stent retriever, which features a hybrid cell design with small closed cells and large open cells with integrated anchoring elements to ensure good vessel wall apposition and clot retention. It is compatible with microcatheters with an inner luminal diameter of 0.0165–0.021 in.
Imaging Evaluation
Angiographic Data
The following angiographic parameters were noted: site of occlusion, accessibility of the occluding thrombus with the small Aperio® 3.5/28, recanalization by the Aperio® 3.5/28 alone or as an additional advice, number of passages, time from first to the final angiogram, and initial and final Thrombolysis in Cerebral Infarction (TICI) Score (successful recanalization was defined as a TICI Score ≥ 2b).
Outcome Data
Potential complications associated with the procedure such as iatrogenic vasospasm in the recanalized artery, emboli transferred into more distal arteries, or intracranial hemorrhage were evaluated using all available imaging data including DSA, CT, and/or MRI by two experienced neuroradiologists consensually. Approximately 24 h after the intervention a CT-Scan was obtained to rule out intracranial hemorrhage. The NIHS Score and the modified Rankin Scale (mRS) at admission and discharge were documented.
Results
Patients and Angiographic Data
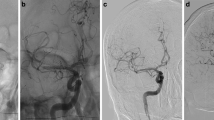
In total, 22 patients were treated with the Aperio® 3.5/28 (see Fig. 1) and 10 patients were women (45.5%). Mean age was 61 years (range 28–91 years). 11 of all 22 patients (6/14 distal occlusions and 5/8 proximal occlusions) received intravenous thrombolysis prior to thrombectomy. Mean vessel diameter treated with the Aperio® 3.5/28 was 1.6 ± 0.11 mm (Figs. 2 and 3).
Selective angiogram of the left internal carotid artery shows the occluded ipsilateral A2 segment (arrow) on the ap- (A) and lateral view (B). An APERIO® stent retriever 3.5 × 28 was deployed covering the thrombus (arrow heads indicate the distal stent marker) (C, D). After 5 min the APERIO® stent retriever was removed under constant aspiration showing a TICI 3 recanalization (E + F)
Selective Angiography of the left vertebral artery showing a right P2 occlusion in lateral oblique- (A) and ap-projection (B). The APERIO® stent retriever 3.5 × 28 was positioned in the right P2 segment spanning the occlusion (C + D) (arrow heads indicate the distal stent marker) and removed after 5 min. A follow-up angiogram demonstrates complete revascularization of the P2 segment in oblique- (E) and ap-projection (F)
First-Line Use of Aperio® 3.5/28
In 9 patients/10 vessels (one patient received a thrombectomy with the Aperio® 3.5/28 in two separate vessels, see Table 1), the Aperio® 3.5/28 was used first line and the mechanical recanalization was performed using the Aperio® 3.5/28 alone. In these patients, the primary targets were smaller vessels (M2 segment n = 7, A3 segment n = 1, hypoplastic basilar artery n = 1, and P1 segment n = 1). In four patients, additional internal carotid stent implantation was necessary due to an ipsilateral proximal high-grade stenotic lesion to achieve successful recanalization (Table 1).
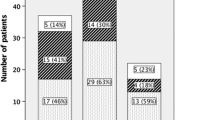
Evaluation of the angiographic data revealed a TICI score of 0 before treatment in 7 patients and a TICI score of 1 in 2 patients. In 7 vessels treated with the Aperio® 3.5/28 alone, a TICI score ≥ 2b could be achieved. In two vessels, a recanalization rate of TICI 2a was observed. A mean number of 1.5 passages has been performed. Mean procedure time from first to final angiograms was 81.1 ± 42.1 min (Table 2).
Second Line Use of Aperio® 3.5/28
In 13 patients, the Aperio® 3.5/28 was used as an additional device and in 11 patients, second due to secondary or remaining occlusion of peripheral arteries (M2 segment n = 9, A1 segment n = 1, P2 segment n = 2, and PICA n = 1) after thrombectomy of a proximal artery. In two patients with primary peripheral occlusion, the Aperio® 3.5/28 was used as first-line device and dragged the thrombus in proximal cerebral arteries, where a larger stent retriever was additionally used to remove the proximal thrombus remnants. The primary used devices are listed in Table 1. Of those, another two patients received additional stenting of a high-grade proximal stenosis of the ipsilateral internal carotid artery.
In this group of patients, a mean number of 1.3 passages with the Aperio® 3.5/28 had been performed. TICI before treatment was 0 in all 13 patients. In the 13 patients treated with a combination of devices, the overall TICI score was 3 in 2 patients, 2b in 9 patients, and 2a in 2 patients. In this group, complete reperfusion (TICI 3) of the vessel treated with the Aperio® 3.5/28 could be achieved in 5 patients and TICI 2b in 4 patients, which results in a successful recanalization rate of 84.6% (11 out of 13). Persisting occlusion of the target vessel (TICI 0) was observed in 3 patients.
Mean time for procedures with Aperio® 3.5/28 as an additional device was 100.2 ± 37.9 min (see Table 2).
Outcome Data
Overall median NIHS score at admission was 8.5 (range 0–20), and median NIHSS for proximal occlusions was 8.5 (range 1–16) and 8.5 (range 0–20) for distal occlusions. Median NIHSS at discharge was 2 (range 0–21). The median mRS at discharge was 2 (range 0–6). A favorable clinical outcome (mRS ≤ 2) was achieved in 12 patients (54.5%) and a moderate outcome (mRS 3 or 4) was noted in 3 patients (16.6%). Poor outcome (mRS 5 or 6) was observed in 7 patients (31.8%). Two patients died during the hospital stay, one from preexisting pneumonia and one from pneumonia due to aspiration.
Mild vasospasm were observed in 5 out of 22 patients, which subsided quickly. In the follow-up CT imaging obtained 24 h after thrombectomy, one patient exhibited a parenchymal bleeding in the corpus callosum after mechanical recanalization of the pericallosal artery. Otherwise, no complications including parenchymal bleedings or signs of infarction due to emboli associated with the intervention were observed.
Discussion
Rapid recanalization of the occluded vessel is the main goal in the treatment of acute ischemic stroke. With recanalization rates up to more than 70% [1,2,3,4,5,6], endovascular stent retriever-based thrombectomy has proven to be superior to i.v. thrombolysis alone in proximal cerebral arteries. However, for more distally located arteries, intravenous thrombolysis is still regarded as standard treatment, although successful recanalization is reported to occur in only 44.2% [14]. Until recently, appropriate devices for endovascular thrombectomy with diameters adapted to the smaller vessel sizes have not been available. However, meanwhile, few smaller stent retrievers have come to the market, and initial results have shown promising results [8, 9].
In our study, we describe our initial experiences of stent retriever-based recanalization of distal cerebral arteries using the Aperio® 3.5/28. This stent retriever was introduced to allow stent retriever-based thrombectomy of smaller cerebral arteries. While established devices are restricted to vessel diameters of 2 mm and larger, this device is suitable for smaller cerebral arteries with a diameter from 1.5 to 3 mm, which allows not only treatment of peripheral branches of the MCA, but also the anterior cerebral artery (ACA) and the PCA as well as cerebellar arteries. In our patient series, the occluded target vessel could be reached in all patients, and the Aperio® 3.5/28 could be deployed in its full length in all cases. Overall recanalization rate (TICI 2b/3) of the Aperio® 3.5/28-target vessel was 73.9%. Even against the background of our relative small and selected series, the recanalization rate of 73.9% exceeds the recanalization results of i.v. thrombolysis [14] and is comparable to the randomized trials of proximal cerebral artery thrombectomy with recanalization rates up to 71% as well as to the recanalization rates of smaller vessels with other adapted endovascular devices describing 70–85.7% [8, 9]. The radial force of a stent retriever, which is crucial to press the clot into the meshes of the stent [15], depends inter alia on the relationship between vessel diameter and diameter of the device, and it is assumed that the smaller the difference of both diameters, the better the radial force. This might explain the results of a study focusing on the anterior circulation that reports a recanalization rate (≥ TICI 2b) for M2 occlusions of 93.3% (14/15 patients) using the Solitaire Fr 4/20 [10], which is recommended by the manufacturer for a vessel diameter not smaller than 2 mm. The diameter at the M2 origins is reported to be 2.4 ± 0.4 mm and the proximal PCA diameter 2.2 ± 0.4 mm, measured on CT angiography [16, 17], which may allow the use of a conventional stent retriever. However, the risk of vessel injury including dissection or severe vasospasm should increase with increasing size of a device and decreasing size of the artery. Along the Sylvian fissure, MCA branches typically measure between 0.25 and 1.7 mm, making smaller devices necessary [18]. Accordingly, in our series, the mean vessel diameter of the target vessel treated with the Aperio® 3.5/28 was with 1.6 ± 0.11 mm smaller than 2 mm and the accesses with a bigger device would not have been favorable. On the other hand, in our series, the thrombus was dislocated from distal into proximal cerebral arteries in two patients and a larger stent retriever was necessary to remove the remnants from the proximal artery. This also supports the idea that a small difference between the diameter of stent retriever and target vessel is crucial for successful clot retrieval, indicating that the application of a small retriever in proximal arteries is not beneficial. Still, we did not observe a relevant difference between successfully treated target vessels (1.59 ± 0.11 mm) and unsuccessfully treated vessels (1.64 ± 0.1 mm).
In our series, one patient (4.5% of patients, 4.3% of vessels) suffered a parenchymal bleeding of the corpus callosum after thrombectomy of the pericallosal artery probably due to injury of perforating branches from the pericallosal artery to the corpus callosum. Although the pericallosal artery showed a diameter larger than 1.5 mm, this arterial segment might be more exposed to radial forces and, therefore, an increased risk of perforator injury. As a consequence, stent retrievers should be used with special caution in this arterial segment. Otherwise, we did not observe any periprocedural complications including secondary peripheral embolization or vessel dissection with subsequent parenchymal or subarachnoid hemorrhage. Furthermore, no severe vasospasm (> 50% of the target vessel’s lumen) occurred after retrieving the Aperio® 3.5/28. Mild vasospasm was seen in 5 out of 22 patients following a retrieval maneuver, but subsided quickly, because routinely, the guiding catheter was continuously flushed with nimodipine solute. Using other small thrombectomy devices, such as the Trevo XP ProVue 3 × 20 technical complications, were observed in 10.5% with non-target arterial embolization and asymptomatic parenchymal hematomas [8]. Thus, the device introduced here shows with a complication rate of 4.5% a good safety profile compared to other devices.
Mean procedure time (from first to final angiogram) was 91.5 ± 39.7 min, which is longer compared to other studies that report procedure times of 49.3 ± 28.6 min [10] or 78 min (range 13–240 min) [8] for the mechanical recanalization of distal arterial occlusions with different stent retrievers. However, in our series, the Aperio® 3.5/28 was used in combination with other devices in 59% of patients, because tandem occlusions including carotid artery stenosis or occlusion of proximal arteries required time-consuming additional procedures including carotid stent implantation (27.3%) and thrombectomy of proximal arteries (31%).
A good neurological outcome (mRS ≤ 2) at discharge was achieved in 54.4% of patients. One patient died from preexisting, non-stroke-related pneumonia, one patient from pneumonia following aspiration. Other studies focusing on neurological outcome after mechanical thrombectomy of distal cerebral arteries report a good neurological outcome in 60% [7, 10] and 56.5% [8]. Though the neurological outcome is comparable, our results have to be interpreted with caution due to the small cohort and the lack of long-term outcome data at 90 days.
Our study is limited by its retrospective nature and small patient cohort without a control group. Furthermore, the cohort is not homogenous. Occlusions of the anterior und posterior circulation, with and without previous intravenous thrombolysis were included, causing heterogeneity of the study population. In addition, we included patients in whom the Aperio® 3.5/28 was used as first line or second device, which might have influenced times of procedure and clinical outcome.
Conclusion
Our initial data suggest that mechanical thrombectomy of distal cerebrovascular occlusions in small cerebral arteries using the Aperio® 3.5/28 is feasible and safe and results in good recanalization rates and clinical outcome data. However, the use of stent retrievers in small vessels with regard to ideal targets and effect on the long-term clinical outcome still needs to be determined with larger cohort, multicenter studies for further evaluation.
References
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723–31. https://doi.org/10.1016/S0140-6736(16)00163-X.
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11–20. https://doi.org/10.1056/NEJMoa1411587.
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–30. https://doi.org/10.1056/NEJMoa1414905.
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA versus t-PA alone in stroke. N Engl J Med. 2015;372(24):2285–95. https://doi.org/10.1056/NEJMoa1415061.
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009–18. https://doi.org/10.1056/NEJMoa1414792.
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 h after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296–306. https://doi.org/10.1056/NEJMoa1503780.
Coutinho JM, Liebeskind DS, Slater LA, Nogueira RG, Baxter BW, Levy EI, et al. Mechanical thrombectomy for isolated M2 occlusions: a post hoc analysis of the STAR, SWIFT, and SWIFT PRIME studies. AJNR Am J Neuroradiol. 2016;37(4):667–72. https://doi.org/10.3174/ajnr.A4591.
Kuhn AL, Wakhloo AK, Lozano JD, Massari F, De Macedo RK, Marosfoi MG, et al. Two-year single-center experience with the ‘Baby Trevo’ stent retriever for mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg. 2017;9(6):541–6. https://doi.org/10.1136/neurintsurg-2016-012454.
Kurre W, Aguilar-Perez M, Martinez-Moreno R, Schmid E, Bazner H, Henkes H. Stent retriever thrombectomy of small caliber intracranial vessels using pREset LITE: safety and efficacy. Clin Neuroradiol. 2016. https://doi.org/10.1007/s00062-016-0497-0.
Dorn F, Lockau H, Stetefeld H, Kabbasch C, Kraus B, Dohmen C, et al. Mechanical thrombectomy of M2-occlusion. J Stroke Cerebrovasc Dis. 2015;24(7):1465–70. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.04.013.
Navia P, Larrea JA, Pardo E, Arce A, Martinez-Zabaleta M, Diez-Gonzalez N, et al. Initial experience using the 3MAX cerebral reperfusion catheter in the endovascular treatment of acute ischemic stroke of distal arteries. J Neurointerv Surg. 2016;8(8):787–90. https://doi.org/10.1136/neurintsurg-2015-011798.
Premat K, Bartolini B, Baronnet-Chauvet F, Shotar E, Degos V, Muresan P, et al. Single-center experience using the 3MAX reperfusion catheter for the treatment of acute ischemic stroke with distal arterial occlusions. Clin Neuroradiol. 2017. https://doi.org/10.1007/s00062-017-0594-8.
Wenger KJ, Berkefeld J, Wagner M. Flat panel detector computed tomography for the interaction between contrast-enhanced thrombi and stent retrievers in stroke therapy: a pilot study. Clin Neuroradiol. 2014;24(3):251–4. https://doi.org/10.1007/s00062-013-0246-6.
Saqqur M, Uchino K, Demchuk AM, Molina CA, Garami Z, Calleja S, et al. Site of arterial occlusion identified by transcranial Doppler predicts the response to intravenous thrombolysis for stroke. Stroke. 2007;38(3):948–54. https://doi.org/10.1161/01.STR.0000257304.21967.ba.
Wenger K, Nagl F, Wagner M, Berkefeld J. Improvement of stent retriever design and efficacy of mechanical thrombectomy in a flow model. Cardiovasc Intervent Radiol. 2013;36(1):192–7. https://doi.org/10.1007/s00270-012-0420-2.
Rai AT, Hogg JP, Cline B, Hobbs G. Cerebrovascular geometry in the anterior circulation: an analysis of diameter, length and the vessel taper. J Neurointerv Surg. 2013;5(4):371–5. https://doi.org/10.1136/neurintsurg-2012-010314.
Rai AT, Rodgers D, Williams EA, Hogg JP. Dimensions of the posterior cerebral circulation: an analysis based on advanced non-invasive imaging. J Neurointerv Surg. 2013;5(6):597–600. https://doi.org/10.1136/neurintsurg-2012-010549.
Ring BA, Waddington MM. Intraluminal diameters of the intracranial arteries. Vasc Surg. 1967;1(3):137–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Müller-Eschner has nothing to disclose. Dr. You has nothing to disclose. Dr. Jahnke has nothing to disclose. Dr. Kammerer has nothing to disclose. Dr. Foerch reports personal fees from Boehringer Ingelheim (honorarium) and Prediction Bioscience (honorarium), outside the submitted work. Dr. Pfeilschifter reports grants and personal fees from Stryker Neurovascular, grants and personal fees from Boehringer Ingelheim, personal fees from Sanofi-Aventis, grants from Novartis, outside the submitted work. Dr. Lauer has nothing to disclose. Dr. Berkefeld reports personal fees from Member of the scientific advisory board of Acandis, Pforzheim, Germany, other from Scientific cooperation with Siemens healthcare, Forchheim, Germany, outside the submitted work. Dr. Wagner reports personal fees from Acandis GmbH, during the conduct of the study.
Ethical Approval
For this type of study, formal consent is not required. This retrospective case series analysis was approved by the institutional review board.
Informed Consent
For this type of study, informed consent is not required.
Consent for Publication
For this type of study, consent for publication is not required.
Rights and permissions
About this article
Cite this article
Müller-Eschner, M., You, SJ., Jahnke, K. et al. Introducing the New 3.5/28 Microstent Retriever for Recanalization of Distal Cerebral Arteries in Acute Stroke: Preliminary Results. Cardiovasc Intervent Radiol 42, 101–109 (2019). https://doi.org/10.1007/s00270-018-2039-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-2039-4