Abstract
Purpose
Most recent guidelines recommend the use of stent retriever devices in endovascular treatment of acute ischemic stroke with large vessel occlusion (LVO). Recently published data reported convincing results with thromboaspiration devices such as the Penumbra System (Penumbra, Alameda, CA, USA) combined with supple reperfusion catheters by using the ADAPT (A Direct Aspiration First-Pass Thrombectomy) technique. The aim of this study was to report our initial experience with the 3MAX (3.8 F) reperfusion catheter for the recanalization of distal intracranial arteries.
Methods
From August 2015 to December 2016, 32 consecutive patients (16 females, 50%; mean age = 67.4 ± 18.7 years, range: 22–91) for 38 distal occlusions underwent mechanical thrombectomy (MT) by thromboaspiration using the 3MAX. Median NIHSS score at admission was 14 (IQR: 9–19). Distal occlusions were distributed as follows: M2 (n: 23), M3 (n: 6), P1 (n: 3), P2 (n: 2), P3 (n: 2), A3 segment (n: 1) and superior cerebellar artery (n: 1).
Results
In 1/38 (2.6%) target artery, the 3MAX could not be navigated. Of the 37 (59.5%) remaining arteries, 22 were successfully reperfused (TICI 2b/3) after ADAPT with the 3MAX alone. Additional stent retriever thrombectomy allowed a 76.3% final reperfusion rate. Good functional outcome (mRS ≤2) was obtained in 45.5% of patients at 3 months. Three (9.4%) 3MAX-related complications occurred: 2 emboli to new territory (ENT) and one vascular perforation.
Conclusions
The 3MAX is well-navigable in distal arteries making it useful as a frontline technique. However, the reperfusion rate with the 3MAX catheter alone seems lower than the ones reported with stent retrievers for such distal occlusions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The management of acute ischemic stroke (AIS) in patients with large vessel occlusion (LVO) has been drastically modified by the positive results of 5 randomized clinical trials testing mechanical thrombectomy (MT) compared to the standard guideline-based therapy [1,2,3,4,5]. These studies led the American Stroke Association and American Heart Association to edict guidelines in June 2015 recommending that patients with AIS caused by LVO should be referred to MT by preferentially using stent retriever devices [6]. The direct aspiration first-pass thrombectomy (ADAPT) technique using supple reperfusion catheters has shown convincing results in terms of reperfusion rates and procedure time reduction for LVO [7, 8]. However, only scant data are available for smaller catheters like the 3MAX in distal occlusions [9, 10].
The primary endpoint of the study was the successful (i. e. Thrombolysis In Cerebral Infarction [TICI] score 2b/3) reperfusion rate using ADAPT with the 3MAX. Secondary evaluation criteria were 3MAX-related complications and good clinical outcome (defined as a modified Rankin Scale [mRS] ≤2) at 3 months.
Materials and Methods
We conducted a single center, retrospective analysis of all consecutive patients with AIS for whom the 3MAX was used at least once in distal MT. We sought to evaluate the navigability, the safety, and the ability of the 3MAX catheter to successfully reperfuse distal arterial occlusions. Distal occlusions were defined as follows: anterior cerebral artery (ACA) occlusions (from A2), middle cerebral artery (MCA) occlusions (from M2), posterior cerebral artery (PCA) occlusions (from P1), cerebellar arteries occlusions. The M2 (aka insular) segment was defined as the part of the MCA from the genu to the circular insular sulcus.
From August 2015 to December 2016, 32 consecutive patients (16 females [50%] and 16 males [50%]; mean age = 67.4 ± 18.7 years, [range: 22–91]) for 38 distal occlusions underwent MT using the 3MAX. Five patients were treated for multiple occlusions. Of the 32 patients included in this study, 4 patients (12.5%) underwent MT subsequently to iatrogenic thromboembolic events, 3 among them occurred during neurointerventional procedures: the first patient had left acute M2 occlusion during the endovascular treatment of a vasospasm at day 10 after embolization of a ruptured anterior communicating artery (AcomA) aneurysm, the second patient had acute right M3 occlusion during the coiling of a ruptured AcomA aneurysm, and the third patient presented multiple M3 occlusions in the aftermath of a periprocedural rupture of an AcomA aneurysm. The last patient had acute left M2 occlusion during a diagnostic coronarography. Of the 32 patients, 5 (15.6%) had tandem occlusions (two vertebrobasilar tandem occlusions and three internal carotid artery/middle cerebral artery tandem occlusions).
Device
The Penumbra 3MAX is the smallest reperfusion catheter designed to perform the most distal thrombectomies. The distal outer and inner diameters are respectively 3.8 F (1.27 mm, 0.050 inches) and 2.7 F (0.89 mm, 0.035 inches) with a proximal outer diameter of 4.7 F (1.57 mm, 0.062 inches) and a 153 cm working length. It is designed to be mounted over a compatible 5–6 F intermediate supple catheter to provide better support to the system. Thromboaspiration can be performed manually by linking a 20–50 ml syringe to the 3MAX or by connecting an electric aspiration pump.
Preoperative care
Preoperative evaluation included a medical examination with neurological assessment performed by a stroke neurologist using the National Institute of Health Stroke Scale (NIHSS) swiftly followed by brain magnetic resonance imaging (MRI). According to our local guidelines, MRI was preferred to CT scan in patients with suspicion of AIS eligible for intravenous thrombolysis (IVT) and/or MT. Of the 32 patients, 18 patients (56.3%) had IVT (r-TPA) before the endovascular procedure in a bridging fashion. All patients underwent this preoperative standardized management except for those whose thromboembolic event was depicted during neurointerventional procedures. In these latter cases, the NIHSS could not be evaluated.
MT Procedure
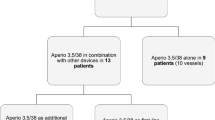
All MT procedures were performed under general anesthesia (n = 19 [59.4%]) or conscious sedation (n = 13 [40.6%]). According to the ADAPT technique, an intermediate aspiration catheter (5MAX/ACE/ACE64 [Penumbra] or 6 F SOFIA/SOFIA PLUS [MicroVention Inc., Tustin, CA, USA]) was mounted over the 3MAX and a 0.014″ microguide wire. The 3MAX was then positioned just upstream from the clot. The microguide wire was removed and the 3MAX was connected to the aspiration system to engage the clot. The 3MAX was then pulled back in the intermediate catheter under constant aspiration, and a control DSA was performed after each aspiration (Fig. 1). A median of 2 (IQR: 1–5) aspiration attempts was performed. If recanalization could not be achieved with ADAPT, the so-called “Solumbra” technique was attempted at the operator’s discretion by deploying a stent retriever (Solitaire Flow Restoration device [ev3-Covidien, Irvine, CA, USA] and/or pREset [Phenox GmbH, Bochum, Germany]) through a Velocity 2.6 F delivery microcatheter (Penumbra).
A 67-year-old man with sudden onset of coma (National Institute of Health Stroke Scale [NIHSS] 28). a Axial susceptibility-weighted magnetic resonance images showing signal void inside the distal basilar artery assessing the presence of the clot which was confirmed by the MR angiography and during perprocedural selective left vertebral artery DSA (Digital Subtraction Angiography) (b, black arrow). c DSA through the ACE64 (black arrow head): clot fragmentation caused by the initial road map injection for catheter navigation is demonstrated: bilateral posterior cerebral artery (PCA) occlusions (P3, black asterisks) and bilateral superior cerebellar artery (SCA) occlusions (First segment on the left side and second segment on the right side [dotted arrows]) are seen. d Road map in anteroposterior (AP) projection. After two failed thromboaspiration attempts with the 3MAX, recanalization of the left PCA was obtained with a stent retriever (4/20 mm Solitaire Flow Restoration; black asterisk) (Thrombolysis In Cerebral Infarction [TICI] 3 recanalization). e Road map in AP projection: direct thromboaspiration through the 3MAX is successfully performed on the right PCA occlusion (white asterisk). f Selective DSA through a Velocity 2.6 F delivery microcatheter (large arrow) (Penumbra) placed into the left SCA after a failed 3MAX navigation attempt, showing occlusion of the left SCA (black arrowhead). TICI 3 was obtained after the second stent-retrieving attempt with a Solitaire. g Control DSA in AP projection: TICI 3 recanalization of both PCAs and left SCA. Partial spontaneous recanalization of the right SCA during the procedure is also seen (dotted arrow). h Axial diffusion weighted images at day 1 after MT: multiple punctuate infarcts as well as an infarct in the right SCA territory are seen (lateral branches; white arrowhead)
Evaluation Criteria
In each case, the feasibility of using the 3MAX (i. e., ability to reach the occlusion site in the target vessel) was assessed. Efficacy of thromboaspiration through the 3MAX was evaluated using the TICI score [11]. Intracerebral hemorrhages were graded according to the SITS-MOST classification [12]. Major procedure-related complications (procedure-related death, vessel perforation, emboli in a new territory [ENT]) including 3MAX-related complications as well as minor complications (vasospasm after thromboaspiration on the target vessel, minor puncture site complication) were also recorded. For each patient, delays from symptoms’ onset to arterial puncture, symptoms’ onset to successful reperfusion, reperfusion time (i. e., time from arterial puncture to recanalization) and procedure lasting were also evaluated.
Imaging and Clinical Follow-up
Postoperatively, all patients had dual-energy CT scan to depict early hemorrhagic complications and differentiate them from postprocedural contrast media extravasation [13]. All living patients had a control brain MRI within the 48 h after MT to evaluate the extent of the ischemic lesions, depict potential complications, and rule out reocclusion of the target vessel. Patients under general anesthesia were extubated immediately after the procedure if their clinical status allowed it. Neurological impairment was assessed using the NIHSS at admission, at day 1, and at discharge after exclusion of the deceased patients. Disability was evaluated with the mRS performed at discharge and at 3 months, when available. A good functional outcome was defined as a mRS score ≤2.
Statistical Analysis
Data analysis was performed using EPI Info 7.1.5.2 software (Centers for Disease Control and Prevention [CDC] Atlanta, GA, USA). Results are presented as means ± standard deviations and ranges or medians with their interquartile range (IQR). Comparison of means was performed using a Student t test or Wilcoxon test, depending on the data distribution. Results were considered statistically significant when P values <0.05.
Results
Patients’ demographics and results are summarized in Table 1.
Overall Results
In one case (2.6%) of a 1.3 mm superior cerebellar artery (SCA) occlusion, the 3MAX could not be navigated. ADAPT alone with the 3MAX allowed successful (TICI 2b/3) reperfusion in 59.5% of the cases. In 10 cases (26.3%), the complementary “Solumbra” technique was used which allowed successful recanalization in 7 cases, thus, achieving an overall reperfusion rate of 76.3%.
The median NIHSS score improved from 14 (IQR: 9–19) at admission to 9 (IQR: 5–18) at 24 h to 6 (IQR: 3–12) at discharge. mRS score was available for 23 patients (71.9%) at discharge and for 22 patients at 3 months (68.8%). A good functional outcome (mRS ≤2) was obtained in 19% of the patients at discharge and 45.5% at 3 months.
Average delay between symptoms’ onset and arterial puncture was 235.5 (±113.8) min, average reperfusion time was 67.7 (±33.4) min and procedures lasted a mean of 85.5 (±38.0) min.
Five patients (15.6%) died during follow-up: one at day 17 and one at day 67 from unrelated causes, two from remote (contralateral) parenchymal hemorrhages (PHrp2) subsequently to the therapeutic management (MT and IVT for both patients), and one from a multivisceral failure. Six (18.8%) major procedure-related complications occurred including three (9.4%) 3MAX-related (2 ENTs and 1 vascular perforation). It is noteworthy that the ENTs were easily removed using ADAPT and were not responsible for any clinical sequelae. The other major procedure-related complications were two vascular perforations (one microguide wire-induced lenticulostriate perforation without any clinical consequences and one after stent retrieval) and one ipsilateral central retinal artery occlusion. In 6 patients, intracerebral hemorrhages were depicted: 3 (9.4%) SICH (2 PHrp2 and 1 PH2), 2 HI1, 1 PH1. Three of them also had asymptomatic subarachnoid hemorrhages. Significant spasm (defined as >50% of the target vessel’s lumen) was seen in 7/38 (18.4%) arteries after ADAPT with the 3MAX. Three of them spontaneously regressed before the end of the procedure.
Anterior Versus Posterior Circulation Occlusions
Seven of the 37 occlusions (18.9%) affected the posterior circulation. The median baseline NIHSS was lower in posterior distal occlusions (7 [IQR: 5–28] vs 15 [IQR: 12–24]; p = 0.47). The rate of successful reperfusion after ADAPT alone was not significantly higher in the posterior occlusion group (85.7% vs 53.3%; p > 0.5) or after rescue stent retriever thrombectomy (100% vs 75%; p > 0.5). Posterior occlusions were associated with a significantly better clinical outcome at 3 months (100% vs 44.4%; p = 0.029) even though no statistical difference in NIHSS at discharge was found (5 [IQR: 4–11] vs 3 [IQR: 0–4] in the posterior group; p > 0.5).
MT for Iatrogenic Thromboembolic Events
Four iatrogenic thromboembolic events were included in the analysis. Successful reperfusion by 3MAX ADAPT alone was obtained in 3 of the 4 cases (80%) and for the last patient, additional stent retriever passages did not achieve successful reperfusion. Good clinical outcome at 3 months was achieved in 50% of cases. No embolic or hemorrhagic complication was recorded.
In the noniatrogenic AIS group, successful reperfusion was achieved in 56.3% of cases with the 3MAX alone and in 75% of cases after complementary stent retriever thrombectomy. A good functional outcome could be obtained in 44% of cases. The results in terms of reperfusion rate and clinical outcome were not significantly different between the noniatrogenic and iatrogenic groups.
Discussion
In the presented series, the self-reported rate of successful reperfusion after ADAPT alone with the 3MAX was 59.5% and complementary stent-retrieving techniques allowed to achieve an overall recanalization rate of 76.3% but three (9.4%) 3MAX-related major complications were recorded. Hence, a good functional outcome was obtained in only 45.5% of patients at 3 months.
ADAPT has gained acceptance as a safe and effective alternative to stent retrievers in LVO [14, 15]. The THERAPY trial [16] that sought to compare thromboaspiration to IVT alone was halted due to emergent proof of the added value of MT over IVT alone, and did not achieve its primary endpoint. Thus, there is a lack of solid evidence for ADAPT even though complementary data suggested that ADAPT is not inferior to primary stent retriever thrombectomy [17]. The 2017 ASTER randomized trial directly compared ADAPT to stent retrievers in LVO and found no significant difference in reperfusion rates and safety using either thrombectomy technique [18].
Distal Intracranial Occlusions
For distal occlusions of the MCA, Saqqur et al. [19] reported a 44.2% rate of complete reperfusion after IVT alone. Dorn et al. [20] compared stentriever-based MT in M2 vs M1 occlusions and reported a higher reperfusion rate (93.3% versus 76.0%; p = 0.186) with fewer periprocedural complications (none vs 3) in M2 occlusions.
The literature provides only retrospective series focused on distal occlusions (Table 2) mainly treated with stent retrievers and displays heterogeneous reperfusion rates (from 70 to 100%) but low complication rates [9, 10, 20,21,22,23,24,25]. Navia et al. [9] provided a 6 case series of distal occlusions treated with ADAPT and found a 100% TICI 2b/3 reperfusion rate with a 83% rate of good clinical outcome, no complication or need to use stent retrievers. Due to the very low number of patients included, direct comparison is delicate. Also in this publication, the strokes’ etiologies were not detailed and maybe clots from different nature or different underlying condition may explain discrepancies with our results.
The choice between ADAPT and stent retriever thrombectomy as the frontline technique is not yet elucidated and the answer is probably not univocal [18]. Our study shows that the 3MAX can navigate efficiently in most situations and reach very distal occlusions, up to A3, M3, or P3 segments (Fig. 2). Arguably, as a faster, safer, and more cost-effective method [8], ADAPT with the 3MAX is acceptable as a frontline technique for distal occlusions. Kim et al. [24] compared forced arterial suction (n = 25 patients) to stent retriever thrombectomy (n = 16) as the frontline technique in M2 occlusions and found a tendency toward a better reperfusion rate (64% vs 81.2%; p = 0.305) with stent retrievers. No statistically significant differences in complication and good functional outcome rates were depicted. The authors also identified that a M2 occlusion located immediately after a severe angulation was associated with an increased rate of failure with ADAPT. In our series a perforation occurred in this exact location, supporting the fact that adequate assessment of the target vessel is crucial when choosing between ADAPT and stent retriever. Vargas et al. [10] proposed a series of 35 patients treated with ADAPT for distal occlusion which was very similar to our study. They reported a TICI 2b/3 rate of 77.1% after ADAPT alone with a conversion rate of 20% to achieve an overall reperfusion rate of 97.1% and reached good clinical outcome in 59.4% of patients at 3 months. Due to the limited number of patients in both our studies, direct comparison is hazardous; however, additional devices permitted to rescue a substantial amount of remaining occlusions. The 3MAX seemed more efficient in very distal occlusions due to the increasing of aspiration force as the vessel’s diameter gets closer to the 3MAX. The 3MAX might also be helpful in iatrogenic distal occlusions or in ENTs to achieve successful reperfusion with a good level a safety, which remains essential in this context. Very acute clots may be more able to pass into small diameter catheters, making them easier to be removed by aspiration. Avoiding deploying a stent retriever that seems more invasive in small vessels may also be an advantage of the 3MAX catheter. Nevertheless, the self-reported reperfusion results showed that ADAPT alone with the 3MAX was able to recanalize most of distal occlusions even in the posterior circulation but was insufficient as the sole reperfusion device. Stent retrievers were still needed and rescued 7 of the 15 (46.7%) remaining occlusions. Moreover, in one case of a proximal SCA (Fig. 1.) occlusion, the target SCA could not be catheterized due to vessel’s angulation and small diameter. In the latter case, a Velocity microcatheter could reach the target occlusion, allowing successful reperfusion of the artery by deploying a Solitaire. For very challenging intracranial catheterization, stent retrievers might be preferred, not for their superiority to reperfuse but simply because the tractability of the delivery microcatheter is more suitable.
A 50-year-old patient with acute onset aphasia and partial motor deficit (National Institute of Health Stroke Scale 6) due to a left M2 occlusion who underwent intravenous thrombolysis and mechanical thrombectomy (MT) at 3 h from symptoms’ onset. a Diffusion weighted imaging (DWI); axial slice showing small insular and opercular acute ischemic stroke (white arrows). b Arterial spin labelling (ASL) perfusion sequence displaying a large hypoperfusion (white asterisk) in the occluded territory assessing the DWI-perfusion mismatch. Note the linear hyperperfusion corresponding to a transit arterial artifact, related to slowdown in a cortical branch (white arrow). c Left internal carotid artery selective DSA (Digital Subtraction Angiography) in left anterior oblique (LAO) projection: inferior division M2 branch occlusion (black arrow) with arterial defect in the corresponding territory (white dotted arrow) are seen. d Control DSA after two thromboaspiration attempts: Thrombolysis In Cerebral Infarction score 2b recanalization 26 minutes after groin puncture. Note the significant spasm at the occlusion’s level (arrowhead). e Control MRI (Magnetic Resonance Imaging) 24 h after MT, DWI; axial slice: no extension of ischemia is seen. f ASL perfusion sequence at day 1 showing complete reperfusion of the posterior MCA territory defect. Note the faint hyperperfusion of the previously hypoperfused territory, also known as “luxury perfusion”
Complications
MT for distal occlusions is controversial as it is known to be technically challenging and associated with a higher complication rate which is confirmed by the presented results. We experienced a perprocedural 3MAX-related rupture at the M1–M2 genu, which was managed by glue occlusion. Ultimately, the patient presented a multivisceral failure at day 9 (mRS 6). Contrast media extravasation and pseudoaneurysm formation after aspiration thrombectomy have already been described with distal aspiration catheters such as the 4MAX [26]. One must always consider that these catheters can be harmful even on large intracranial arteries especially at junction points or in tortuous segments. In comparison, the series from Vargas et al. [10] comprised 80% isolated M2 occlusions, one M3 and one A3 occlusion; they reported two major procedure-related complications. In our series, we aimed to reperfuse even very distal occlusions up to A3 (one case), M3 (six cases) and P3 (two cases) which inevitably exposes to a greater risk of complications.
ENT may be encountered with all types of MT devices. However, in the literature, the ENT rate seems lower with aspiration devices (from 0–6%) [27, 28] than with stentrievers (from 0–13.3%) [29, 30]. ENTs were observed in two cases in our series, which could be easily recanalized with the 3MAX without any clinical consequences.
Even though average NIHSS score was similar to other series, the rate of mRS 0–2 at 3 months was low. This can be explained by a higher rate of major complications and the inclusion of patients in poor general condition (ruptured intracranial aneurysms, advanced cardiovascular diseases or recovered cardiac arrest before MT).
Procedure Times
Average reperfusion time was 67.7 (±33.4) min and was rather long in comparison to the study of Vargas et al. [10] which reported a mean time to recanalization of 35.5 (±26.4) min with distal ADAPT. It is a direct consequence of an inferior reperfusion rate after ADAPT alone and a superior rate of perprocedural complications. Moreover, five patients had multiple occlusions and five had tandem occlusions that considerably increased the procedure times.
Limitations
The value of this study is limited by the retrospective and monocentric fashion of data collection and analysis as well as the small number of patients included. We also purposely included patients with iatrogenic thromboembolic events to display a more representative population who may benefit from distal recanalization. However, the nature of the clots encountered in thromboembolic events occurring during embolization is probably different from the one observed in patients with non-iatrogenic AIS. The lack of core-lab evaluation, the absence of control group, and the fact that mRS at 3 months was available for only 62.5% of the patients does not allow an optimal assessment of clinical outcome. Furthermore, mRS is probably an inaccurate tool to evaluate the outcome of patients with distal occlusions, especially in the ACAs and vertebrobasilar territories where the clinical consequences (e.g., behavioral disorders, anopia, dyspraxia) are not adequately assessed by this scale.
Conclusion
The 3MAX reperfusion catheter is a well-navigable catheter, making it acceptable as a frontline technique in distal MT, especially in case of periprocedural thromboembolic event. The reperfusion rate with the ADAPT technique using a 3MAX catheter alone appears lower than the ones reported with stent retrievers. One must also be aware of the risk of vascular injury, especially in tortuous and angulated segments. Randomized trials are needed to efficiently compare ADAPT to stent retrievers in distal occlusions.
Abbreviations
- AcomA:
-
Anterior Communicating Artery
- ACA:
-
Anterior Cerebral Artery
- ADAPT:
-
A Direct Aspiration First-Pass Thrombectomy
- AIS:
-
Acute Ischemic Stroke
- DSA:
-
Digital Subtraction Angiography
- ENT:
-
Embolus to New Territory
- IVT:
-
Intravenous Thrombolysis
- LVO:
-
Large Vessel Occlusion
- MCA:
-
Middle Cerebral Artery
- mRS:
-
Modified Rankin Scale
- MRI:
-
Magnetic Resonance Imaging
- MT:
-
Mechanical Thrombectomy
- NIHSS:
-
National Institute of Health Stroke Scale
- PCA:
-
Posterior Cerebral Artery
- r-TPA:
-
Recombinant Tissue Plasminogen Activator
- SCA:
-
Superior Cerebellar Artery
- SICH:
-
Symptomatic Intracranial Hemorrhage
- TICI:
-
Thrombolysis in Cerebral Infarction
References
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, van Walderveen MA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, Kappelle LJ, Lo RH, van Dijk EJ, de Vries J, de Kort PL, van Rooij WJ, van den Berg JS, van Hasselt BA, Aerden LA, Dallinga RJ, Visser MC, Bot JC, Vroomen PC, Eshghi O, Schreuder TH, Heijboer RJ, Keizer K, Tielbeek AV, den Hertog HM, Gerrits DG, van den Berg-Vos RM, Karas GB, Steyerberg EW, Flach HZ, Marquering HA, Sprengers ME, Jenniskens SF, Beenen LF, van den Berg R, Koudstaal PJ, van Zwam WH, Roos YB, van der Lugt A, van Oostenbrugge RJ, Majoie CB, Dippel DW; MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20.
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W, Jansen O, Jovin TG, Mattle HP, Nogueira RG, Siddiqui AH, Yavagal DR, Baxter BW, Devlin TG, Lopes DK, Reddy VK, du Mesnil de Rochemont R, Singer OC, Jahan R; SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t‑PA vs. t‑PA alone in stroke. N Engl J Med. 2015;372:2285–95.
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD; ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–30.
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, San Román L, Serena J, Abilleira S, Ribó M, Millán M, Urra X, Cardona P, López-Cancio E, Tomasello A, Castaño C, Blasco J, Aja L, Dorado L, Quesada H, Rubiera M, Hernandez-Pérez M, Goyal M, Demchuk AM, von Kummer R, Gallofré M, Dávalos A; REVASCAT Trial Investigators. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296–306.
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M, Ang T, Scroop R, Barber PA, McGuinness B, Wijeratne T, Phan TG, Chong W, Chandra RV, Bladin CF, Badve M, Rice H, de Villiers L, Ma H, Desmond PM, Donnan GA, Davis SM; EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–18.
Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, Johnston KC, Johnston SC, Khalessi AA, Kidwell CS, Meschia JF, Ovbiagele B, Yavagal DR; American Heart Association Stroke Council. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015;46:3020–35.
Vargas J, Spiotta A, Fargen K, Turner R, Chaudry I, Turk A. Long term experience using the ADAPT technique for the treatment of acute ischemic stroke. J Neurointerv Surg. 2017;9:437-41.
Turk AS 3rd, Campbell JM, Spiotta A, Vargas J, Turner RD, Chaudry MI, Battenhouse H, Holmstedt CA, Jauch E. An investigation of the cost and benefit of mechanical thrombectomy for endovascular treatment of acute ischemic stroke. J Neurointerv Surg. 2014;6:77–80.
Navia P, Larrea JA, Pardo E, Arce A, Martínez-Zabaleta M, Díez-González N, Murias E, Arráez-Aybar LA, Massó J. Initial experience using the 3MAX cerebral reperfusion catheter in the endovascular treatment of acute ischemic stroke of distal arteries. J Neurointerv Surg. 2016;8:787–90.
Vargas J, Spiotta AM, Fargen K, Turner RD, Chaudry I, Turk A. Experience with a direct aspiration first pass technique (ADAPT) for thrombectomy in distal cerebral artery occlusions causing acute ischemic stroke. World Neurosurg. 2017;99:31–6.
Zaidat OO1, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, Marks MP, Prabhakaran S, Kallmes DF, Fitzsimmons BF, Mocco J, Wardlaw JM, Barnwell SL, Jovin TG, Linfante I, Siddiqui AH, Alexander MJ, Hirsch JA, Wintermark M, Albers G, Woo HH, Heck DV, Lev M, Aviv R, Hacke W, Warach S, Broderick J, Derdeyn CP, Furlan A, Nogueira RG, Yavagal DR, Goyal M, Demchuk AM, Bendszus M, Liebeskind DS; Cerebral Angiographic Revascularization Grading (CARG) Collaborators; STIR Revascularization working group; STIR Thrombolysis in Cerebral Infarction (TICI) Task Force. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013;44:2650–63.
Wahlgren N, Ahmed N, Dávalos A, Ford GA, Grond M, Hacke W, Hennerici MG, Kaste M, Kuelkens S, Larrue V, Lees KR, Roine RO, Soinne L, Toni D, Vanhooren G; SITS-MOST investigators. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet. 2007;369:275–82.
Tijssen MP, Hofman PA, Stadler AA, van Zwam W, de Graaf R, van Oostenbrugge RJ, Klotz E, Wildberger JE, Postma AA. The role of dual energy CT in differentiating between brain haemorrhage and contrast medium after mechanical revascularisation in acute ischaemic stroke. Eur Radiol. 2014;24:834–40.
Hussain SI, Zaidat OO, Fitzsimmons BF-M. The Penumbra system for mechanical thrombectomy in endovascular acute ischemic stroke therapy. Neurology. 2012;79:S135–S41.
Romano DG, Cioni S, Vinci SL, Pero G, Comelli C, Comai A, Peschillo S, Mardighian D, Castellan L, Resta F, Piano MG, Comelli S, Barletta L, Puliti A, Leonini S, Bracco S. Thromboaspiration technique as first approach for endovascular treatment of acute ischemic stroke: initial experience at nine Italian stroke centers. J Neurointerv Surg. 2017;9:6–10.
Mocco J, Zaidat OO, von Kummer R, Yoo AJ, Gupta R, Lopes D, Frei D, Shownkeen H, Budzik R, Ajani ZA, Grossman A, Altschul D, McDougall C, Blake L, Fitzsimmons BF, Yavagal D, Terry J, Farkas J, Lee SK, Baxter B, Wiesmann M, Knauth M, Heck D, Hussain S, Chiu D, Alexander MJ, Malisch T, Kirmani J, Miskolczi L, Khatri P; THERAPY Trial Investigators*. Aspiration thrombectomy after intravenous alteplase versus intravenous alteplase alone. Stroke. 2016;47:2331–8.
Stapleton CJ, Torok CM, Patel AB. 110 Noninferiority of a direct aspiration first-pass technique vs stent retriever thrombectomy in emergent large-vessel Intracranial occlusions. Neurosurgery. 2016;63(Suppl 1):146–7.
Lapergue B, Labreuche J, Piotin M. Aster trial. Contact aspiration vs stent retriever front line for rencanalization in acute cerebral infarction. LB2. International Stroke Conference, Houston, 22.–24. Feb 2017. 2017.
Saqqur M, Uchino K, Demchuk AM, Molina CA, Garami Z, Calleja S, Akhtar N, Orouk FO, Salam A, Shuaib A, Alexandrov AV; CLOTBUST Investigators. Site of arterial occlusion identified by transcranial Doppler predicts the response to intravenous thrombolysis for stroke. Stroke. 2007;38:948–54.
Dorn F, Lockau H, Stetefeld H, Kabbasch C, Kraus B, Dohmen C, Henning T, Mpotsaris A, Liebig T. Mechanical thrombectomy of M2-occlusion. Stroke. 2015;24:1465–70.
Pfaff J, Herweh C, Pham M, Schieber S, Ringleb PA, Bendszus M, Möhlenbruch M. Mechanical thrombectomy of distal occlusions in the anterior cerebral artery: recanalization rates, periprocedural complications, and clinical outcome. AJNR Am J Neuroradiol. 2016;37:673–8.
Kurre W, Aguilar-Pérez M, Martinez-Moreno R, Schmid E, Bäzner H, Henkes H. Stent retriever thrombectomy of small caliber Intracranial vessels using pREset LITE: safety and efficacy. Clin Neuroradiol. 2016 Jan 21. [Epub ahead of print]
Coutinho JM, Liebeskind DS, Slater LA, Nogueira RG, Baxter BW, Levy EI, Siddiqui AH, Goyal M, Zaidat OO, Davalos A, Bonafé A, Jahan R, Gralla J, Saver JL, Pereira VM. Mechanical thrombectomy for isolated M2 occlusions: a post hoc analysis of the STAR, SWIFT, and SWIFT PRIME studies. AJNR Am J Neuroradiol. 2016;37:667–72.
Kim YW, Son S, Kang DH, Hwang YH, Kim YS. Endovascular thrombectomy for M2 occlusions: comparison between forced arterial suction thrombectomy and stent retriever thrombectomy. J Neurointerv Surg. 2016 Jul 5. [Epub ahead of print]
Park JS, Kwak HS. Manual aspiration thrombectomy using penumbra catheter in patients with acute M2 occlusion : a single-center analysis. J Korean Neurosurg Soc. 2016;59:352–6.
Jeong EO, Kwon HJ, Choi SW, Koh HS. Pseudoaneurysm formation after repetitive suction thrombectomy using a penumbra suction catheter. J Cerebrovasc Endovasc Neurosurg. 2016;18:296–301.
Investigators TPPST. The penumbra pivotal stroke trial safety and effectiveness of a new generation of mechanical devices for clot removal in Intracranial large vessel occlusive disease. Stroke. 2009;40:2761–8.
Kowoll A, Weber A, Mpotsaris A, Behme D, Weber W. Direct aspiration first pass technique for the treatment of acute ischemic stroke: initial experience at a European stroke center. J Neurointerv Surg. 2016;8:230–4.
Stampfl S, Kabbasch C, Müller M, Mpotsaris A, Brockmann M, Liebig T, Wiesmann M, Bendszus M, Möhlenbruch MA. Initial experience with a new distal intermediate and aspiration catheter in the treatment of acute ischemic stroke: clinical safety and efficacy. J Neurointerv Surg. 2016;8(7):714–8.
Gascou G, Lobotesis K, Machi P, Maldonado I, Vendrell JF, Riquelme C, Eker O, Mercier G, Mourand I, Arquizan C, Bonafé A, Costalat V. Stent retrievers in acute Ischemic stroke: complications and failures during the perioperative period. AJNR Am J Neuroradiol. 2014;35:734–40.
Acknowledgements
The authors of this manuscript would like to thank Ms. Christine Pires for her kind help with the collection of clinical data.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
N. Sourour is proctor for the Pipeline Embolization Device and for the Medina Embolization Device (Medtronic). F. Clarençon is consultant for Medtronic, Balt (paid lectures) and for Codman Neurovascular (Study Core lab). K. Premat, B. Bartolini, F. Baronnet-Chauvet, E. Shotar, V. Degos, P. Muresan, F. Di Maria, J. Gabrieli, C. Rosso, S. Pistocchi, J. Chiras, S. Alamowitch and Y. Samson declare that they have no competing interests.
Ethical standards
Neither approval of the institutional review board nor patient informed consent are required by the ethics committee of our institution for retrospective analyses of patients’ records and imaging data.
Additional information
Contributorship
All authors made a substantial, direct, and intellectual contribution to the work. Kévin Premat: Data collection, manuscript redaction, statistical analysis. Bruno Bartolini: Data collection, critical review of the manuscript. Flore Baronnet-Chauvet: Data collection. Eimad Shotar: Data collection, critical review of the manuscript. Vincent Degos: Critical review of the manuscript. Paul Muresan: Data collection. Federico Di Maria: Data collection. Joseph Gabrieli: Manuscript editing. Charlotte Rosso: Critical review of the manuscript. Silvia Pistocchi: Critical review of the manuscript. Jacques Chiras: Study supervision. Nader Sourour: Manuscript editing. Sonia Alamowitch: Critical review of the manuscript. Yves Samson: Critical review of the manuscript. Frédéric Clarençon: Study supervisor, critical review of the manuscript.
Rights and permissions
About this article
Cite this article
Premat, K., Bartolini, B., Baronnet-Chauvet, F. et al. Single-Center Experience Using the 3MAX Reperfusion Catheter for the Treatment of Acute Ischemic Stroke with Distal Arterial Occlusions. Clin Neuroradiol 28, 553–562 (2018). https://doi.org/10.1007/s00062-017-0594-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-017-0594-8