Abstract
Purpose
Cystic echinococcosis (CE) in the spleen is a rare disease even in endemic regions. The aim of this study was to examine the efficacy of percutaneous treatment for splenic CE.
Materials and Methods
Twelve patients (four men, eight women) with splenic CE were included in this study. For percutaneous treatment, CE1 and CE3A splenic hydatid cysts were treated with either the PAIR (puncture, aspiration, injection, respiration) technique or the catheterization technique.
Results
Eight of the hydatid cysts were treated with the PAIR technique and four were treated with catheterization. The volume of all cysts decreased significantly during the follow-up period. No complication occurred in seven of 12 patients. Abscess developed in four patients. Two patients underwent splenectomy due to cavity infection developed after percutaneous treatment, while the spleen was preserved in 10 of 12 patients. Total hospital stay was between 1 and 18 days. Hospital stay was longer and the rate of infection was higher in the catheterization group. Follow-up period was 5–117 months (mean, 44.8 months), with no recurrence observed.
Conclusion
The advantages of the percutaneous treatment are its minimal invasive nature, short hospitalization duration, and its ability to preserve splenic tissue and function. As the catheterization technique is associated with higher abscess risk, we suggest that the PAIR procedure should be the first percutaneous treatment option for splenic CE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Echinococcal infection is caused by the larval form of the cestode Echinococcus, with E. granulosus accounting for 95 % of all cases [1]. The most commonly affected organ is the liver (70 %), followed by the lung (15–20 %) and spleen (0.9–8 %) [2–5]. Isolated splenic involvement is very uncommon [6, 7]. Splenic cystic echinococcosis (CE) is generally asymptomatic, and its diagnosis is generally established during imaging for other reasons [8–10]. Although most patients do not exhibit any symptoms, symptoms can present from complications such as left upper quadrant pain, rupture, or secondary infection [11, 12].
Serology has a limited role in the diagnosis of CE because of its inability to distinguish between active and inactive cysts, low sensitivity, and cross-reactivity with other helminths such as E. multilocularis and Taenia solium [13].
Treatment of viable splenic CE is indicated because of the risk of infection and rupture [6]. Traditionally, surgery was the only accepted treatment modality for splenic CE [1, 14, 15]. Several surgical techniques have been advocated, ranging from splenectomy to spleen-sparing surgical resection [14, 15]. Percutaneous treatment of splenic CE has also gained acceptance with modern advances in interventional radiology [2, 16].
The aim of the present study was to examine the efficacy of percutaneous treatment of splenic CE using the PAIR (puncture, aspiration, injection, respiration) or the catheterization techniques.
Materials and Methods
Twelve patients (four men, eight women) with splenic CE were included in the study. Age of the patients ranged between 5 and 57 years (mean age 26.3 years). All patients were examined with chest X-ray and abdominal ultrasonography (US), while five of 12 patients were examined with abdominal computed tomography (CT), prior to treatment. Two patients (2/12) had isolated splenic CE. Eight patients had coexisting liver CE, while two patients had coexisting liver and lung CE.
All cysts were classified according to the classification described by the World Health Organization [17]. Inclusion criteria were ultrasound and computed tomography evidence of viable hydatid cyst (CE1, CE2, CE3A, and CE3B). Two CE1 and two CE 3A patients were treated using the catheterization technique, while eight CE1 patients were treated by PAIR. Only patients with a confident diagnosis were included in the study. The diagnosis of splenic CE was proven by cytological examination of specimen acquired by aspiration and radiological findings during and after the percutaneous treatment, as previously described [18]. Patients with CE4 or CE5 cysts were excluded from the study and managed by the ‘wait and watch’ approach.
Percutaneous Treatment Technique
Before the Procedure
To reduce the risk of the abdominal dissemination caused by leakage of the cyst fluid, patients were given albendazole (10 mg/kg/day) at 1 week before and during the period of 4 weeks after the procedure [18, 19]. After the patients fasted overnight, they received intravenous sedation with midazolam and fentanyl, and were monitored by an anesthesiology team during the procedures for anaphylactic shock or allergic reaction. The interventional procedure was performed by combined ultrasonographic and fluoroscopic guidance. The desired tract of the needle from the selected puncture site to the cyst was passed through the normal splenic tissue to reduce the potential risk for leakage.
The Procedure
For the PAIR technique (P: puncture of the cyst, A: aspiration of the cyst content, I: Injection of hypertonic saline solution or alcohol, R: respiration of all fluid) [20], the first puncture was performed under US guidance using an 18–19 G needle after the safe entry path from the entry site to the cyst was decided. As soon as the targeted cyst was penetrated, 20 % of fluid content of the cyst was aspirated. We injected contrast media (10–20 mL) into the cavity under fluoroscopic guidance before almost all fluid content of the cyst was aspirated and hypertonic saline solution (15–30 %) was injected into the punctured cyst. All the fluid in the cavity was aspirated after approximately 10 min. and absolute alcohol (95 % alcohol, approximately 30–50 % of the aspirated cavity volume) was instilled. After 5–10 min, all the cystic content including alcohol was re-aspirated before the needle was removed.
The second technique involved the ‘catheterization technique with hypertonic saline and alcohol’, originally proposed by Akhan et al. after an experimental study in sheep [21]. In this technique, the cyst was punctured under US guidance with a Seldinger needle, and 20 % of fluid content of the cyst was aspirated. We injected contrast media (10–20 mL) into the cavity under fluoroscopic guidance to confirm that there is no leakage. Almost all fluid content of the cyst was aspirated before we injected hypertonic saline (15–30 %) for approximately 6–10 min until detachment of the endocyst. We then advanced a 0.035-inch Amplatz guide wire under fluoroscopy guidance before the placement of a small pig tail catheter (6–8 F pig tail) using a modified Seldinger technique. After irrigation of the cavity with hypertonic saline, the catheter was fixed to the skin with a single suture and left for gravity drainage. When the daily drainage of the cavity was less than 10 mL, absolute alcohol (95 % alcohol, approximately 30–50 % of the aspirated cavity volume) was instilled. After 5–10 min, all the cystic content including alcohol was re-aspirated via the catheter before it was removed. If the daily drainage was more than 10 mL, the catheter was kept in place until the daily drainage stopped, and sclerosis by 95 % alcohol was obtained under fluoroscopic guidance before withdrawal of the catheter.
As a rule, the PAIR technique was applied for cysts smaller than 250 mL, while the catheterization technique was performed for cysts larger than 250 mL. Only one cyst (660 mL) larger than 250 mL was treated by PAIR instead of catheterization owing to the preference of the interventional radiology team who performed the procedure.
Patient Follow-up and Complications
During the follow-up, abdominal US was performed at the end of first month in all patients. US was then performed once every 3 months during the first year after the procedure, twice a year during the second year, and once yearly for following years. CT examination was performed during the follow-up if indicated. On follow-up US examinations, the size, volume, content, and wall changes of the treated CE were evaluated. The healing criteria included considerable reduction in the size and volume of the cyst, irregularity and thickening of the cyst wall, decrease in the fluid component of the cavity, and solidification of the cyst in time by disappearance of fluid component [21]. This solid remnant was defined as a pseudotumor appearance on US. These changes in the treated CE occured gradually after the procedure.
Complications were grouped as minor or major according to the ‘SIR Classification System for Complications by Outcome’. We defined a major complication as one that required an additional invasive procedure, prolonged hospital stay, or resulted in significant morbidity or mortality [22].
Results
Twelve patients (four men, eight women) with splenic CE were treated percutaneously. Patient data are summarized in Table 1. CE treated by percutaneous treatment were ten CE1 and two CE3A cysts. Eight of the CE were treated with the PAIR technique, while four were treated with the catheterization technique. Total hospital stay was between 1 and 18 days (mean 3.9, median 1). The hospital stay was between 1 and 4 days (mean 1.4) for the PAIR technique and between 1 and 18 days (mean 9) for the catheterization technique.
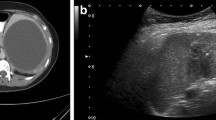
The follow-up period was 5–117 months (mean 44.8), with no recurrence observed during follow-up. The volume of the cysts decreased significantly during the follow-up period (Fig. 1). Cyst volumes were between 3.8 and 1100 mL (mean 326 mL) at admission and between 0 and 108 mL (mean 27.4 mL) after percutaneous treatment. The mean percent volume reduction of the CE in spleen-preserved patients was 77.3 %. After treatment, the mean residual volume of the catheterization group (17.5 mL) was less than the PAIR group (35.6 mL). Further, the mean percent volume reduction for catheterization technique was 95 % while it was 69 % for the PAIR technique.
Seven of the cysts exhibited a tumor-like lesion (pseudotumor appearance) during the follow-up, while the remaining two cysts had minimal fluid component within the cavity without any sign of viability. One cyst totally disappeared after percutaneous treatment. Two patients underwent splenectomy because of splenic abscesses. Before surgery, these patients were vaccinated against pneumococcus.
No mortality, anaphylactic reaction, or bleeding were encountered during or after the percutaneous treatment in our study. No complication occurred in seven of 12 patients. The only minor complication was self-limiting fever that occurred once in one patient. The major complication was infection in the cavity diagnosed in four patients, requiring percutaneous treatment or surgery. The abscesses were diagnosed 1–18 months after percutaneous procedure. Abscesses developed predominantly in the catheterization group (three of four patients). Only one abscess developed in the PAIR group. Two patients with abscesses were treated percutaneously and one patient with splenectomy. The fourth patient with abscess was treated percutaneously at 1 month after the PAIR procedure. However, as the abscess reappeared 5 months later after percutaneous drainage, it was then treated by splenectomy (Fig. 2).
Discussion
Because of the risk of rupture and secondary infection, there is an indication for splenic CE to be treated. Splenectomy is associated with a high morbidity rate of 21 %, overall mortality up to 7 %, and a long duration of hospitalization (3–47 days) [1, 5, 23–25]. In a recent study, 26 patients with splenic CE were treated with splenectomy, with a recurrence rate of 3.8 % [23]. Complications of splenectomy include hemorrhage, gastric injury, or pancreatic fistulae caused by careless or inadequate surgery [6]. Thromboembolic complications occur predominantly in patients with myeloproliferative diseases. Overwhelming post-splenectomy infections that usually involve an encapsulated organism (usually pneumococcus and Haemophilus influenza) can also occur, especially in children younger than 4 years of age who undergo splenectomy. Splenectomy is associated with sepsis-related deaths in 1.9 % of adults and 4 % of children [23]. Partial cystectomy and omentopexy were suggested as the procedure of choice for the surgical treatment of splenic CE [16, 26]. Laparoscopic or robotic surgical treatment of splenic CE was also reported [1, 15, 27]. Atmatzidis et al. demonstrated that the recurrence rate, complication rate, and hospital rate after total splenectomy were similar to spleen-preserving surgery [5]. Further, no differences in mean hospital stay and no recurrence was observed following spleen-preserving surgery or splenectomy [28–30]. In a series of 21 patients, Ran et al. reported a residual cavity infection in a patient who underwent spleen-preserving surgery. Arıkanoglu et al. also reported a hemorrhage and subsequent intraabdominal abscess in one patient with spleen-preserving surgery in a study of 11 patients with splenic CE [30]. Spleen-preserving surgery may be justified in children to avoid septic complications.
Percutaneous treatment of splenic CE was widely accepted after studies reporting the success of percutaneous treatment of liver CE [18, 21]. However, there are a limited number of studies on percutaneous treatment of splenic CE. Ormeci et al. presented a therapeutic approach for the treatment of splenic CE in nine patients [2]. Over a median follow-up period of 39 months, one patient exhibited urticaria and low-grade fever just after the procedure, and one patient received splenectomy at 8 months after percutaneous treatment because of persistent left upper quadrant pain. The authors suggest that percutaneous treatment of splenic CE is a safe and reliable method that does not interfere with splenic function. Zerem et al. presented a series of eight patients with splenic CE treated with a modified PAIR procedure (injection of 95 % alcohol, 1 % polidocanol, and 1 % albendazole) [16]. The mean hospital stay was 2.5 days, and the mean volume reduction was 77.8 %. The follow-up period was between 7 and 24 months. No major complications were detected. Immediately following the procedure, one patient exhibited urticaria, one patient exhibited transient hypotension, and two patients had fever. The authors suggest that modified PAIR can be performed safely with successful results in patients with splenic CE.
A number of early and late complications should be considered when using percutaneous treatment of splenic CE. Early complications include hemorrhage, pneumothorax, pleural effusion, and colonic injury during and following splenic puncture, anaphylaxis, and hypersensitivity reactions such as urticaria and fever. Data concerning the risk of splenic puncture are primarily based upon other interventional procedures such as splenic biopsies. Söderström reported no complications in a study of over 1000 blind splenic fine needle aspirations [31]. Similarly, the majority of previous studies have reported a low complication rate after both fine-needle aspiration and small-bore cutting-edge needle biopsy of the spleen, with a reported incidence of hemorrhage after splenic biopsy between 0 and 10.3 % [32–36]. In the present study, there was no evidence of hemorrhage, pneumothorax, pleural effusion, colonic injury, or anaphylactic reaction during and following cyst puncture. The exact frequency of anaphylaxis is not known, although the risk of anaphylactic reactions in percutaneous treatment is similar to surgical procedures in patients with liver CE. When the number of liver CE treated percutaneously is taken into consideration, the mortality rate due to anaphylactic shock is approximately 0.1 % [37].
Late complications of surgical and percutaneous treatment include infection in the cavity, recurrence, and dissemination [38, 39]. Although the reported recurrence rate for percutaneous treatment of liver CE is between 0 and 4 %, no recurrence was observed in our study [39]. Further, we observed no mortality. The major complication in the present study was cavity infection requiring percutaneous treatment or surgery, with abscess developing in four of our patients (three after catheterization technique, one after PAIR) as a late complication. In the PAIR group, abscess developed in only one patient after treatment of the largest hydatid cyst (660 mL). As abscesses were most common in the catheterization group in our series, we suggest that the catheterization technique should be avoided for percutaneous treatment of splenic CE if technically possible.
Conclusion
The most important consideration in the treatment of splenic CE is the preservation of splenic tissue and function, particularly in children. Splenic preservation using spleen-saving surgery or percutaneous treatment should be attempted if possible. Percutaneous treatment of splenic CE is associated with a low morbidity rate and a short hospital stay, without mortality and recurrence, apart from its ability to preserve splenic function. Therefore, we suggest that the percutaneous approach should be the first treatment option for splenic CE if the cyst is either CE1 or CE3A. Further, PAIR should be the first percutaneous technique in patients with splenic CE. Nevertheless, future randomized prospective studies are required to fully determine the efficacy and safety of this approach.
References
Safioleas M, Misiakos E, Manti C. Surgical treatment for splenic hydatidosis. World J Surg. 1997;21:374–8.
Ormeci N, Soykan I, Palabiyikoğlu M, Idilman R, Erdem H, Bektaş A, et al. A new therapeutic approach for treatment of hydatid cysts of the spleen. Dig Dis Sci. 2002;47:2037–44.
Franquet T, Montes M, Lecumberri FJ, Esparza J, Bescos JM. Hydatid disease of the spleen: imaging findings in 9 patients. AJR. 1990;154:525–8.
Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS. Hydatid disease: radiologic and pathologic features and complications. RadioGraphics. 2000;20:795–817.
Atmatzidis K, Papaziogas B, Mirelis C, Pavlidis T, Papaziogas T. Splenectomy versus spleen-preserving surgery for splenic echinococcosis. Dig Surg. 2003;20:527–31.
Durgun V, Kapan S, Kapan M, Karabiçak I, Aydogan F, Goksoy E. Primary splenic hydatidosis. Dig Surg. 2003;20:38–41.
Prousalidis J, Tzardinoglou K, Sgouradis L, Katsohis C, Aletras H. Uncommon sites of hydatid disease. World J Surg. 1998;22:17–22.
Urrutia M, Mergo PJ, Ros LH, Torres GM, Ros PR. Cystic masses of the spleen: radiologic-pathologic correlation. RadioGraphics. 1996;16:107–29.
von Sinner WN, Stnidbeck H. Hydatid disease of the spleen: ultrasonography, CT and MR imaging. Acta Radiol. 1992;33:459–61.
Robertson F, Leander P, Ekberg O. Radiology of the spleen. Eur Radiol. 2001;11:80–95.
Lewall DB. Hydatid disease: biology, pathology, imaging and classification. Clin Radiol. 1998;53:863–74.
Dahniya MH, Hanna RM, Ashebu S, Muhtaseb SA, el-Beltagi A, Badr S, et al. The imaging appearance of HD at some unusual sites. Br J Radiol. 2001;74:283–9.
Tamarozzi F, Sako Y, Ito A, Piccoli L, Grisolìa A, Itoh S, et al. Recombinant AgB8/1 ELISA test vs. commercially available IgG ELISA test in the diagnosis of cystic echinococcosis. Parasite Immunol. 2013;35:433–40.
Khoury G, Abiad F, Geagea T, Nabout G, Jabbour S. Laparoscopic treatment of hydatid cysts of the liver and spleen. Surg Endosc. 2000;14:243–5.
Manouras AJ, Nikolaou CC, Katergiannakis VA, Apostolidis NS, Golematis BC. Spleen-sparing surgical treatment for echinococcosis of the spleen. Br J Surg. 1997;84:1162.
Zerem E, Nuhanovic A, Caluk J. Modified PAIR technique for treatment of hydatid cysts in the spleen. Bosn J Basic Med Sci. 2005;5:74–8.
WHO Informal Working Group. International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop. 2003;85:253–61.
Akhan O, Ozmen MN, Dinçer A, Sayek I, Göçmen A. Liver hydatid disease: long-term results of percutaneous treatment. Radiology. 1996;198:259–64.
Akhan O, Yildiz AE, Akinci D, Yildiz BD, Ciftci T, et al. Is the adjuvant albendazole treatment really needed with PAIR in the management of liver hydatid cysts? A prospective, randomized trial with short-term follow-up results. Cardiovasc Interv Radiol. 2014;37:1568–74.
Ben Amor N, Gargouri M, Gharbi HA, Ghorbel A, Golvan YJ, Hammou-Jeddi H, et al. Traitment du kyste hydatique du foie du mouton par ponction sous e´chographie. Tunis Med. 1986;64:325–31.
Akhan O, Dincer A, Gököz A, Sayek I, Havlioglu S, Abbasoglu O, et al. Percutaneous treatment of abdominal hydatid cysts with hypertonic saline and alcohol: an experimental study in sheep. Investig Radiol. 1993;28:121–7.
Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of interventional radiology clinical practice guidelines. J Vasc Interv Radiol. 2003;14:S199–202.
Dar MA, Shah OJ, Wani NA, Khan FA, Shah P. Surgical management of splenic hydatidosis. Surg Today. 2002;32:224–9.
Uriarte C, Pomares N, Martin M, Conde A, Alonso N, Bueno MG. Splenic hydatidosis. Am J Trop Med Hyg. 1991;44:420–3.
Eris C, Akbulut S, Yildiz MK, Abuoglu H, Odabasi M, Ozkan E, et al. Surgical approach to splenic hydatid cyst: single center experience. Int Surg. 2013;98:346–53.
Ozdogan M, Baykal A, Keskek M, Yorgancy K, Hamaloglu E, Sayek I. Hydatid cyst of the spleen: treatment options. Int Surg. 2001;86:122–6.
Vasilescu C, Tudor S, Popa M, Tiron A, Lupescu I. Robotic partial splenectomy for hydatid cyst of the spleen. Langenbecks Arch Surg. 2010;395:1169–74.
Meimarakis G, Grigolia G, Loehe F, Jauch KW, Schauer RJ. Surgical management of splenic echinococcal disease. Eur J Med Res. 2009;14:165–70.
Ran B, ShaoY Yimiti Y, Aji T, Shayiding P, Jiang T, et al. Spleen preserving surgery is effective for the treatment of spleen cystic echinococcosis. Int J Infect Dis. 2014;29:181–3.
Arikanoglu Z, Taskesen F, Gumus H, Onder A, Aliosmanoglu I, Gul M, et al. Selecting a surgical modality to treat a splenic hydatid cyst: total splenectomy or spleen-saving surgery? J Gastrointest Surg. 2012;16:1189–93.
Söderström N. How to use cytodiagnostic spleen puncture. Acta Med Scand. 1976;199:1–5.
Lucey BC, Boland GW, Maher MM, Gervais DA, Mueller PR. Percutaneous nonvascular splenic intervention: a 10-year review. Am J Roentgenol. 2002;179:1591–6.
Muraca S, Chait PG, Connolly BL, Baskin KM, Temple MJ. US-guided core biopsy of the spleen inchildren. Radiology. 2001;218:200–6.
Lieberman S, Libson E, Maly B, Lebensart P, Ben-Yehuda D, Bloom AI. Imaging guided percutaneous splenic biopsy using a 20- or 22-gauge cutting-edge core biopsy needle for the diagnosis of malignant lymphoma. Am J Roentgenol. 2003;181:1025–47.
Liang P, Gao Y, Wang Y, Yu X, Yu D, Dong B. Us-guided percutaneous needle biopsy of the spleen using 18-gauge versus 21-gauge needles. J Clin Ultrasound. 2007;35:477–82.
Tam A, Krishnamurthy S, Pillsbury EP, Ensor JE, Gupta S, Murthy R, et al. Percutaneous image-guided splenic biopsy in the oncology patient: an audit of 156 consecutive cases. J Vasc Interv Radiol. 2008;19:80–7.
Smego RA Jr, Bhatti S, Khaliq AA, Beg MA. Percutaneous aspiration-injection-reaspiration drainage plus albendazole or mebendazole for hepatic cystic echinococcosis: a meta-analysis. Clin Infect Dis. 2003;37:1073–83.
Akhan O, Ozmen MN. Percutaneous treatment of liver hydatid cysts. EJR. 1999;32:76–85.
Franquet T, Cozcolluela R, Montes M, Sanchez J. Abscessed splenic hydatid cyst: sonographic and CT findings. Clin Imaging. 1991;15:118–20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Okan Akhan declares no conflict of interest. Selçuk Akkaya declares no conflict of interest. Merve Gülbiz Dağoğlu declares no conflict of interest. Burcu Akpınar declares no conflict of interest. Aysun Erbahçeci declares no conflict of interest. Türkmen Çiftçi declares no conflict of interest. Mert Köroğlu declares no conflict of interest. Devrim Akıncı declares no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Akhan, O., Akkaya, S., Dağoğlu, M.G. et al. Percutaneous Treatment of Splenic Cystic Echinococcosis: Results of 12 Cases. Cardiovasc Intervent Radiol 39, 441–446 (2016). https://doi.org/10.1007/s00270-015-1265-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-015-1265-2