Abstract
Objective
Percutaneous osteosynthesis plus cementoplasty (POPC) is a minimally invasive technique that has never been reported before and that we have prospectively evaluated for patients with impending pathological fracture of the proximal femur.
Methods
We performed POPC in 12 patients (3 males, 9 females) with metastasis of the proximal femur with a high risk of fracture (Mirels’ score ≥8) between February 2010 and July 2011. Patients were not candidates for standard surgical stabilization. We analyzed the feasibility, duration, and complication of the procedure, the risk of fracture, the decrease in pain (Visual Analog Scale, VAS), and length of stay in hospital. Data were prospectively collected in all patients.
Results
The mean Mirels’ score was 9.8 ± 1.2 (range, 8–11). The technical success was 100%. POPC was performed under general anesthesia (n = 6) or conscious sedation (n = 6). The mean duration was 110 ± 43 (range, 60–180) minutes. All patients stood up and walked the second day after the procedure. The average length of stay in the hospital was 4 ± 1.6 (range, 2–7) days. We experienced two hematomas in two patients and no thromboembolic complication. For symptomatic patients (n = 8), VAS decreased from 6.5/10 (range, 2–9) before treatment to 1/10 (range, 0–3) 1 month after. No fracture occurred after a median follow-up of 145 (range, 12–608) days.
Conclusions
POPC for impending pathological fracture of the proximal femur seems to be a promising alternative for cancer patients who are not candidates for surgical stabilization. Further studies are required to confirm this preliminary experience.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteolytic metastasis can be responsible for pathological fracture. Impending pathological fracture of the head or trochanteric region of the femur should be treated before fracture occurs. Surgery is the standard of care to improve mechanical stability with protheses or osteosynthesis. Prophylactic surgical stabilization improves the quality of life of patients by decreasing the stress and the pain of a pathological fracture and decreases intraoperative and postoperative complications compared with surgery performed after pathological fracture has occurred [1–3]. However, prophylactic surgical stabilization is associated with surgical morbidity and mortality, especially in patients with metastatic disease [2, 3]. According to Mirels’ recommendation (Table 1), prophylactic fixation is highly indicated for a lesion with an overall score of 8 or greater [4, 5]. Other authors state that the best predictive criterion of fracture is the cortical involvement >30 mm [6].
Percutaneous cementoplasty has been used as an alternative for stabilization of impending pathologic fracture of proximal femur, but several reports in the literature have concluded that even if pain relief is very satisfactory after cementoplasty there is a risk of fracture due to insufficient consolidation of this weight-bearing bone [7–10]. Percutaneous osteosynthesis by cannulated screws is a well-established method for the treatment of nondisplaced femoral neck fractures, especially in elderly patients with comorbidities due to low operative invasiveness [11]. The purpose of this study was to evaluate the feasibility of a percutaneous stabilization using percutaneous osteosynthesis associated with percutaneous cementoplasty and to assess whether it allows the stabilization of impending pathological fracture of the proximal femur and prevents the occurrence of these fractures.
Material and Methods
Patients
We prospectively enrolled all consecutive patients who underwent percutaneous osteosynthesis plus cementoplasty (POPC) for impending pathological fracture of the proximal femur in our institution starting from our initial experience with this technique. The inclusion criteria were patients with metastasis of the proximal femur with a high risk of pathological fracture, defined by a Mirels’ score ≥8 (Fig. 1), who were not candidates for standard surgical stabilization because of poor performance status or refused surgery. Approval from the local institutional review board and informed consent were obtained from all patients before procedures.
Technique
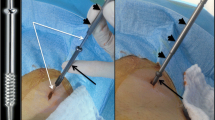
The procedures were performed by an interventional radiologist in an angio suite. Percutaneous osteosynthesis was performed with 8 mm cannulated screws (Trauma Asnis III, Stryker, Switzerland). An inverted triangle configuration of screw placement was considered to be optimal for stabilization. Thus, insertion of three guide pins parallel to the femoral neck axis was performed under fluoroscopic guidance combined with 3D acquisition from C-arm CT. The first guide pin was inserted along the inferior cortical of the femoral neck. The other two were placed against the upper cortical femoral neck—one posteriorly and the other anteriorly. The 3D acquisitions with a C-arm CT were performed to assess the good position of the three guide pins and to measure the appropriate length of each cannulated screws to be inserted. Three percutaneous incisions of less than 1 cm large were performed around the guide pin at the skin entry site. The cannulated screws were advanced over the guide pins under fluoroscopic guidance using a cannulated screwdriver. When screws were adequately placed, the guide pins were removed. Finally, cementoplasty was performed under fluoroscopic guidance (Fig. 2). To inject a maximal amount of polymethyl-methacrylate (CementoFixx, Optimed, Germany) as possible we performed simultaneous injections (at least two sites of injection) through 11-gauge beveled needles (Osteo-Site needle, Cook, Bjaeverskov, Denmark).
Same patient as Fig. 1. A Guide pin (white arrow head) has been inserted under fluoroscopic guidance through a minimal skin incision (black dashed circle). A cannulated screw (black arrow) is ready to be inserted over the guide pin using a cannulated screwdriver. B, C Three cannulated screws have been inserted over the three guide pins, which are still in place (white arrow heads), under fluoroscopic guidance in an inverted triangle configuration. Then, two 11-gauge beveled needles (white dashed arrows) were used for cement injection (black dashed arrows)
POPC was performed under general anesthesia or conscious sedation plus local anesthesia and continuous femoral nerve block. The choice between general anesthesia and conscious sedation depended on the general performance status of the patient. Conscious sedation was preferred for the patient with poor performance status. It was associated with local anesthesia and a continuous femoral nerve block.
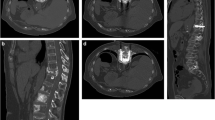
All patients were followed with medical consultation and X-ray examination of the femur at 1 month and then every 3 months until death occurred (Fig. 3).
Same patient as Fig. 1. X-ray examination at 12 months. AP view (A, C) and profile (B) of the proximal femur show no modification of the bones, screw, or cement in a patient with a VAS score of 2/10
Data Analysis
The primary end point was the risk of fracture of the proximal femur. We analyzed the feasibility of this new procedure, its duration, and complications. We also analyzed the Mirels’ score, the cortical involvement metastasis, the pain (using Visual Analog Scale (VAS)) before, during (in case of conscious sedation), and 1 month after the procedure, and the length of stay in hospital.
The duration of the procedure includes the time between the beginning of osteosynthesis and the end of cementoplasty.
Results
Twelve consecutive patients (3 males, 9 females) with a median age of 55 ± 14 (range, 28–77) years were prospectively included between February 2010 and July 2011 (Table 2). The primary tumors were breast (n = 6), neuroendocrine tumor (n = 2), lung (n = 1), hepatocarcinoma (n = 1), thyroid (n = 1), and melanoma (n = 1). The mean Mirels’ score was 9.8 ± 1.2 (range, 8–11). Nine patients had an osteolytic metastasis located in the trochanteric region and three in the femoral neck. Five patients had no cortical involvement and seven patients had cortical involvement, including six with a cortical involvement >30 (mean, 51) mm. These metastases were asymptomatic in four patients and painful in eight. In five patients, the treatment of the femoral metastasis was associated with treatment of other bone metastases during the same procedure: cementoplasty of acetabulum (n = 1), vertebroplasty (n = 1), cryotherapy of two iliac metastases plus triple vertebroplasty (n = 1), cementoplasty of the contralateral femoral shaft (n = 1), and cryotherapy plus cementoplasty of two pelvic bone metastases (n = 1).
The POPC was technically feasible in all patients. The mean duration for osteosynthesis plus cementoplasty was 110 ± 43 (range, 60–180) minutes. Six patients underwent general anesthesia. Six patients underwent conscious sedation with a maximum VAS of 2.6/10 (range, 0–5) during the procedure. All patients were allowed to stand up the second day after the procedure, and the average length of stay in the hospital was 4 ± 1.6 (range, 2–7) days.
No fracture occurred during a median follow-up of 145 (range, 12–608) days.
We report no death during treatment or during the hospital stay and 33% (4/12) within 3 months after the treatment. At the present time, six patients have died from cancer after a median follow-up of 60 (range, 12–175) days, and six patients are still alive after a median follow-up of 406 (range, 59–608) days.
We experienced two hematomas in two patients at the puncture site at 3 and 15 days, which required two red blood cells units transfusion each. In the first case, the hematoma occurred during the hospitalization and the length of stay in the hospital has been prolonged for 2 days. In the second case, the transfusion was performed ambulatory. We did not experience any infection or thromboembolic complications during the follow-up.
For symptomatic patients (n = 8), the maximal pain decreased from 6.5/10 ± 2.2 (range, 2–9) before treatment to 1/10 ± 1.1 (range, 0–3) 1 month after.
Discussion
The decision to perform an orthopedic treatment for impending fracture of the proximal femur is difficult in cancer patients, because the indication must take into account the risk of fracture, the general condition of the patient, and the prognostic of the cancer disease, namely life expectancy. Concerning the risk of fracture little is known about the natural behavior of impending pathological fracture of the proximal femur without surgical fixation According to Mirels’ recommendation (Table 1), prophylactic fixation is highly indicated for a lesion with an overall score of 8 or greater [4, 5]. Other authors state that the best predictive criterion of fracture is cortical involvement >30 mm [6]. A pragmatic approach is currently to fix all patients with expected high-risk lesions. However, this could lead to surgical “overtreatment” in patients who only have a limited life expectancy and results in postoperative morbidity and mortality, which can be considerable in this population. A retrospective study of prophylactic surgery for stabilization of femoral metastatic lesions in 201 patients reported a length of stay in the hospital of 19.3 days; 8% of surgical or medical complications occurred during hospitalization and 3% of deep vein thrombosis within 3 months after surgery [3]. Death during surgery was 1, 9% during the hospital stay, and 13.9% within 3 months. POPC make it a good alternative for patients who are not candidates for standard surgical stabilization even if it is very likely that the mechanical consolidation obtained with this technique is less important than orthopedic protheses or osteosynthetic devices. Indeed, the level of consolidation obtained in our series seems sufficient in patients with advanced cancer disease or poor general condition, because we did not experience any fracture despites a population at risk with a Mirels’ score >8 and/or cortical involvement superior to 30 mm in 6 of 12 patients.
POPC is highly feasible and has several advantages. The first advantage is that it can be performed under conscious sedation with very low pain level. This is very interesting in all patients but even more in patients with poor general condition. The second clear advantage is the minimal invasiveness, with only three skin entry points <1 cm, avoiding damage to the muscles around the femur and decreasing the pain and the disability after the procedure. This minimal invasiveness probably also decreases the risk of infection and blood loss especially in case of hypervascular metastases. The third advantage is the short bed rest required (mean = 2 days) associated with a short hospital stay (mean = 4 days), which would decrease the risk of thromboembolic complications compared with conventional surgery. The fourth advantage is that this treatment could be associated with thermal ablation during the same procedure or with external radiotherapy. At least, additional cementoplasties or percutaneous ablations can be performed during the same procedure for patients with distant bone metastases.
There are some limitations in our study, including the small number of patients. However, to our knowledge, it is the first report of this technique in the literature. Another limitation is the relatively short follow-up, because several patients died of cancer progression. In some way, death without fracture is the goal of this palliative treatment. Finally, there is no comparison with other therapeutic options, such as cementoplasty alone or no treatment.
Conclusions
Percutaneous stabilization of impending pathological fracture of the proximal femur using POPC is highly feasible by an interventional radiologist. It seems to be a promising alternative for patients who are not candidates for surgical stabilization because of poor performance status. It is a minimally invasive technique that can be performed under conscious sedation, with very low complication rates and short hospital stay. Further studies are required to confirm this preliminary experience, including larger series and comparison with other nonsurgical available treatments.
References
Ward WG, Holsenbeck S, Dorey FJ et al (2003) Metastatic disease of the femur: surgical treatment. Clin Orthop Relat Res (415 Suppl): S230–S244
Popken F, Schmidt J, Oegur H et al (2002) Treatment outcome after surgical management of osseous breast carcinoma metastases. Preventive stabilization vs. management after pathological fracture. Unfallchirurg 105(4):338–343
Ristevski B, Jenkinson RJ, Stephen DJ et al (2009) Mortality and complications following stabilization of femoral metastatic lesions: a population-based study of regional variation and outcome. Can J Surg 52(4):302–308
Mirels H (1989) Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res (249):256–264
Jawad MU, Scully SP (2010) In brief: classifications in brief: Mirels’ classification: metastatic disease in long bones and impending pathologic fracture. Clin Orthop Relat Res 468(10):2825–2827
Van der Linden YM, Dijkstra PD, Kroon HM et al (2004) Comparative analysis of risk factors for pathological fracture with femoral metastases. J Bone Joint Surg Br 86(4):566–573
Anselmetti GC, Manca A, Ortega C et al (2008) Treatment of extraspinal painful bone metastases with percutaneous cementoplasty: a prospective study of 50 patients. Cardiovasc Interv Radiol 31(6):1165–1173
Dayer R, Peter R (2008) Percutaneous cementoplasty complicating the treatment of a pathologic subtrochanteric fracture: a case report. Injury 39(7):801–804
Chang SW, Murphy KP (2005) Percutaneous CT-guided cementoplasty for stabilization of a femoral neck lesion. J Vasc Interv Radiol 16(6):889–890
Basile A, Giuliano G, Scuderi V et al (2008) Cementoplasty in the management of painful extraspinal bone metastases: our experience. Radiol Med 113(7):1018–1028
Schep NW, Heintjes RJ, Martens EP et al (2004) Retrospective analysis of factors influencing the operative result after percutaneous osteosynthesis of intracapsular femoral neck fractures. Injury 35(10):1003–1009
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Deschamps, F., Farouil, G., Hakime, A. et al. Percutaneous Stabilization of Impending Pathological Fracture of the Proximal Femur. Cardiovasc Intervent Radiol 35, 1428–1432 (2012). https://doi.org/10.1007/s00270-011-0330-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-011-0330-8