Abstract
Purpose
Screw fixation (osteosynthesis) can be performed percutaneously by interventional radiologists. We report our experience in cancer patients.
Material/methods
We retrospectively reviewed all cases of percutaneous osteosynthesis (PO) of the pelvic ring and proximal femur performed in our hospital. PO were performed for fracture palliation or for osteolytic metastases consolidation. Screws were inserted under CT- or cone-beam CT- guidance and general anaesthesia. Patients were followed-up with pelvic-CT and medical consultation at 1 month, then every 3 months. For fractures, the goal was pain palliation and for osteolytic metastases, pathologic fracture prevention.
Results
Between February 2010 and August 2014, 64 cancer patients were treated with PO. Twenty-one patients had PO alone for 33 painful fractures (13 bone-insufficiency, 20 pathologic fractures). The pain was significantly improved at 1 month (VAS score = 20/100 vs. 80/100). In addition, 43 cancer patients were preventively consolidated using PO plus cementoplasty for 45 impending pathologic fractures (10 iliac crests, 35 proximal femurs). For the iliac crests, no fracture occurred (median-FU = 75 days). For the proximal femurs, 2 pathological fractures occurred (fracture rate = 5.7 %, median-FU = 205 days).
Conclusion
PO is a new tool in the therapeutic arsenal of interventional radiologists for bone pain management.
Key Points
• Screw fixation (osteosynthesis) can be performed percutaneously by interventional radiologists.
• CT- or CBCT-guidance results in high technical success rates for screw placement.
• This minimally invasive technique avoids extensive surgical exposure in bone cancer patients.
• Osteosynthesis provides pain relief for bone-insufficiency fractures and for pathologic fractures.
• Osteosynthesis plus cementoplasty provide prophylactic consolidation of impending pathological fractures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Metastatic bone disease is very common in cancer patients and can cause a pathologic fracture, giving rise to significant pain and loss of function. Prophylactic stabilization before a fracture occurs is an issue of utmost importance. In addition, fractures can occur in cancer patients because of bone insufficiency, which may be primary (osteoporosis) or secondary to treatments (steroids, radiation of pelvic malignancies, thermal ablation, etc.).
Percutaneous osteosynthesis (PO) is a new technique for interventional radiologists. It consists of inserting screws into bone structures through a minimal skin incision (less than 10 mm). Osteosynthesis was initially developed by orthopaedic surgeons to stabilize non-displaced bone fractures during open surgery [1–4]. The technique can now be performed percutaneously by interventional radiologists due to the development of cannulated screws that can be inserted coaxially over a stiff metallic wire needle, and thanks to the level of accuracy that is possible with computed tomography (CT) guidance or cone beam CT (CBCT) guidance [5–9].
PO is used both palliatively in patients suffering from fractures and as a prophylactic consolidation in patients with an impending pathologic fracture due to osteolytic metastases.
We report our experience of PO of the pelvic ring and of the proximal femur in cancer patients.
Material and methods
We retrospectively reviewed all the PO procedures performed in cancer patients for palliation of a fracture or for preventive consolidation of the pelvic ring or of the proximal femur. All patient files were discussed at a multidisciplinary pain meeting before the procedure and the institutional review boards approved this study.
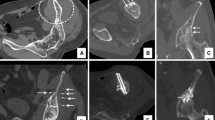
The procedures were entirely performed by interventional radiologists, either under CT guidance (LightSpeed, GE Medical Systems, Milwaukee, Wis) or in an Angio Suite equipped with CBCT guidance (Innova 4100IQ, GE Healthcare, Chalfont St Giles, UK). All the procedures were performed under general anaesthesia. The interventional radiologist first drilled a Kirschner wire across the fracture site/tumour under CT fluoroscopy guidance or under CBCT guidance using dedicated guidance software (TrackVision, GE Healthcare, Chalfont St Giles, UK). Then, a three-dimensional (3D) image of the pelvis was obtained via CT or CBCT to assess the proper direction of the Kirschner wire and to measure the appropriate length of the screw to be inserted. Ideally, the screw should be long enough to reach the distal sub-chrondral bone and must enter a strong cortical bone. The 8-mm cannulated self-drilling, tapping screw (Asnis III cannulated screws; Stryker, Montreux, Switzerland) was placed over the Kirschner wire and slid down to the cortical bone using a cannulated screw driver (Fig. 1). Once proper positioning of the screw was confirmed by a new 3D acquisition, the Kirschner wire was withdrawn and the skin entry point was sutured.
Palliation of fractures
For bone insufficiency or pathologic fractures, the goal of PO was to achieve fracture stabilization that would result in pain palliation. For this purpose we performed osteosynthesis without cement injection. The decision to perform PO for pelvis fractures was based on the visual analog scale (VAS) score, that must be at least 50/100, and on a pre-op CT. Typically, fractures that can be fixed using PO are located in the sacrum, the iliac crest, the acetabulum roof, the pubic ramus and the proximal femur (Fig. 2). Ideally, the fracture should be non-displaced because it is impossible to anatomically reduce fracture fragments percutaneously.
Technically, the screws should be inserted perpendicularly to the fracture and across the fracture. We did not perform cementoplasty for fracture stabilization because the mechanical property of the cement is not appropriate for the stabilization of locations submitted to torsion forces [10] and because there is a risk of cement leakage through the fracture line. Actually, this leakage can be relevant if it occurred in the adjacent joint or could result in stopping the injection prematurely.
In the case of sacral fractures [5, 6], two screws were advanced over the ilio-sacral joint. If the fracture was unilateral, the two screws were inserted ipsilaterally into the first and second sacral vertebral bodies, respectively. If the fracture was bilateral, the two screws were inserted into the first sacral vertebral body: one from the left side and one from the right side (Figs. 2 and 3).
For fractures located in the iliac crest [7] or in the acetabulum roof [8, 11], one screw was inserted perpendicular to the plane of the fracture line to be fixed and, therefore, depended on the site of the fracture (Fig. 2).
For a pubic ramus fracture, fixation consists of inserting a retrograde screw into the distal medial fragment of the superior ramus [1–3, 12] (Figs. 2 and 3).
For a femoral fracture, an inverted triangle configuration for screw placement was considered optimal for stabilization [4, 13, 14]. Thus, three screws were inserted parallel to the femoral neck axis. The first screw was inserted along the inferior cortex of the femoral neck. The other two were placed against the superior cortex of the femoral neck—one posteriorly and the other anteriorly (Fig. 2).
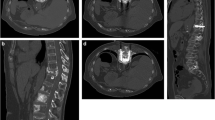
Consolidation of an impending pathologic fracture
For patients with osteolytic metastasis in the pelvis, the goals of the procedure were to prevent a pathologic fracture and to decrease the pain, if present. In order to do so, we performed PO plus cementoplasty. The decision to perform PO plus cementoplasty instead of cementoplasty alone was based on the fact that the strengthening properties of the cement are strong in the case of compression but weak for tensile or shear stresses [10, 15]. Technically, we inserted the screws across the osteolytic metastases first and then injected the cement into the osteolytic metastases thanks to a dedicated cementoplasty needle that is inserted in parallel through the same screw path. We started the injection close to the tips of the screws for good screw anchorage and continued the injection while removing the needle. We always tried to fill the entire osteolytic metastases. Typically, the impending osteolytic metastases that can be consolidated using PO plus cementoplasty was located in the proximal femur and in the iliac crest (Fig. 4).
For osteolytic metastases of the proximal femur, the decision to perform prophylactic consolidation was based on Mirel’s score [16]. According to Mirel’s recommendation (Table 1), there is a high risk of a pathologic fracture when the overall lesion score is 8 or greater. In patients who were not candidates for standard surgical stabilization (refusal, poor performance status or on-going chemotherapy) despite a Mirel score of 8 or greater, we performed osteosynthesis plus cementoplasty of the proximal femur. Technically, we inserted three screws in an inverted triangle configuration into the femoral neck (as previously described) and we then injected the cement (Opacity+, Technimed, ViC en Bigorre, France) through an 8-gauge bevelled needle (Transpedicular Introducer, Laurane, Westbrook, USA) into the osteolytic metastases and around the three screws (Figs. 4 and 6). The first twelve prophylactic consolidations of osteolytic metastases of the proximal femur have been previously reported [17]. This prior article dealt with development and feasibility of the technique whereas, in this manuscript, we report on the long term outcome in a larger population.
For osteolytic metastases in the iliac crest, the decision to perform prophylactic consolidation was based on the multidisciplinary meeting evaluation. Actually, there is no validated score to predict the risk of fracture of the iliac crest. In our current practice, we consider that there is a high risk of a pathologic fracture when the metastasis diameter exceeds 40 mm and if there is cortical disruption, especially in the greater sciatic notch. We inserted two screws through the long axis of the iliac crest using a posterior approach to treat these metastases. The path was from the posterior iliac crest to the upper edge of the acetabulum. We then used an 8-gauge bevelled needle (as above) to inject the cement (as above). This needle was inserted in parallel via the same screw path (Figs. 4 and 5).
Follow-up and data analysis
All patients were followed up with a pelvic CT and a medical consultation with an interventional radiologist at 1 month and then every 3 months with a medical oncologist. For painful fractures, the primary endpoints were pain palliation and no fracture displacement. For impending pathologic fractures, the primary endpoints were pain palliation (if present), and no pathologic fracture during the follow-up. To analyze pain palliation, we used the VAS score to compare pain before the procedure and 1 month after. To analyze the occurrence of fracture displacement despite screw fixation and to report the occurrence of a fracture despite preventive consolidation with osteosynthesis plus cementoplasty, we analyzed all the imaging exams performed after the procedure. We also report on the duration of the procedure and of the hospital stay. The duration of the procedure comprised the time between the initial 3D acquisition and suture of the entry point(s). We report the length of the screws inserted according to the location, the amount of cement injected and the rate of osteolytic metastasis of the proximal femur associated with cortical disruption. Actually, some authors state that the best prognostic factor for a pathologic fracture of the proximal femur is not Mirel’s score, but the existence of cortical disruption measuring 30 mm or more [15, 18]. Finally, we report on procedure-related complications, the rate of screw misplacement (not crossing the fracture, entering the joint surface, etc.) and cement leakage. Figure 6
Results
Painful fractures
From June 2010 to August 2014, 21 cancer patients (3 males and 18 females, mean age 58.6 ± 8.8 years old [range 28.8 to 75.5 y-o] were treated with PO for 33 fractures in 24 procedures. Patients had pelvic primary cancer (rectum n = 3, uterine cervix n = 3, prostate n = 2, ovarian n = 1), breast cancer (n = 5), lung cancer (n = 2) or a variety of other primary cancers (n = 5). The fractures were bone-insufficiency fractures in 13 cases and pathologic fractures in 20 cases. They were located in the sacrum (n = 16, including 5 bilateral), the iliac crest or acetabulum roof (n = 9), the pubic ramus (n = 7) and the proximal femur (n = 1). The mean duration of the procedure was 70 ± 15 minutes [range 30 to 140 minutes] and the mean hospital stay was 2 days [range 1 to 6 days] (Table 2). The average length of the screws inserted was: 85 mm [range 50 to 120 mm] for a sacral fracture, 95 mm [range 65 to 130 mm] for an iliac crest or acetabulum roof fracture, 80 mm [range 60 to 110 mm] for a pubic ramus fracture and 90 mm [range 85 to 95 mm] for a proximal femur fracture. The pain was significantly improved at 1 month (VAS score = 20/100 vs. 80/100). No difference was found between the improvement in osteoporotic (VAS score = 15/100 vs. 75/100) and pathologic fractures (VAS score = 25/100 vs. 80/100). No fracture displacement occurred at CT after a median follow-up of 189 days [range 31 to 1472 days].
Consolidation of impending pathologic fractures
From February 2010 to August 2014, 43 cancer patients (18 males and 25 females, mean age 61.1 ± 8.7 years old [range 28.4 to 83.7 y-o] were preventively treated with PO plus cementoplasty for 45 impending pathologic fractures in 43 procedures. All patients had bone metastases, mainly from breast (n = 12) and lung cancers (n = 9) but also from thyroid (n = 2), kidney (n = 2) and variety of other primary cancers (n = 18). The impending pathologic fractures were located in the iliac crest (n = 10) and the proximal femur (n = 35) (Table 3).
For the iliac crest (n = 10), the mean maximum diameter of the osteolytic metastases was 7 cm [range 5 to 9 cm] and 80 % (n = 8) had caused cortical disruption. Two screws were inserted for each treatment, each screw measuring an average length of 120 mm [range 105 to 130 mm]. The mean amount of cement injected was 12 ml [range 4 to 20 ml]. The mean duration of the procedure was 90 minutes [range 60 to 150 minutes] and the mean hospital stay was 1.3 day [range 1 to 2 days]. For painful impending pathologic fractures of the iliac crest (n = 8), osteosynthesis plus cementoplasty resulted in a significant decrease in the VAS score from 80/100 before osteosynthesis to 26/100 1 month after osteosynthesis. No fracture occurred over a mean follow-up of 75 days [range 30 to 383 days].
For proximal femur metastases (n = 35), the mean Mirel score was 10.1 [range 8 to 12].
Twenty-one osteolytic metastases (60 %) were associated with cortical disruption, including 15 with a 30-mm rupture. Three screws were inserted for each treatment, each measuring an average length of 105 mm [range 85 to 130 mm]. The mean amount of cement injected was 6 ml [range 3 to 10 ml]. The mean duration of the procedure was 110 minutes [range 60 to 180 minutes] and the mean hospital stay was 3.1 days [range 1 to 8 days]. For painful impending pathologic fractures of the proximal femur (n = 26), osteosynthesis plus cementoplasty resulted in a significant decrease in the VAS score (10 vs. 70) at 1 month. After a mean follow-up of 205 days [range 24 to 1633 days], two pathological fractures occurred and both required open surgery for stabilization (fracture rate = 5.7 %). The first fracture occurred 3 weeks after the procedure. In this patient, the risk of fracture was very high: the Mirel score was 12 and cortical disruption was 50 mm long. In addition, the three screws entered a smooth–surfaced cortical bone. In the second patient, the fracture occurred 7 months after the procedure after fall injury. At this point in time, 22 patients have died (mean follow-up of 126 days) without any femoral fracture.
Complications
Four haematomas occurred at the puncture site in four patients and a red blood cell transfusion was required in two patients. Pain associated with haematomas resolved in less than 10 days. A haematoma was responsible for a prolonged hospital stay for 2 days in one patient. No infection or procedure-related thrombo-embolic complications occurred during the follow-up. No screw misplacement was depicted at 1 month on CT but 9 (20 %) cement leakages occurred (in soft tissue only) without any symptoms.
Discussion
Pelvic fractures, particularly hip fractures, are a major source of morbidity and mortality in cancer patients. The fractures are secondary to decreased bone strength due to either osteolytic metastasis or osteoporosis which can be promoted by treatments (steroids, radiation of pelvic malignancies, thermal ablation, etc.). In a retrospective analysis, Schmeler et al. [19] reported that pelvic fractures were detected in approximately 10 % of women after definitive radiotherapy (RT) for cervical cancer. They also demonstrated that the median time from the completion of RT to the detection of fractures on imaging studies was 14.1 months and that fractures were more frequently associated with a lower body mass index (BMI). Similarly, Uezono et al. [20] reported that the 2- and 5-year cumulative incidence of overall pelvic insufficiency fractures were 32 % and 63 %, respectively, after definitive RT for uterine cancer. They also reported that the median interval between the first day of RT and the detection of the fracture was 14 months and that the distribution of the fractures was as follows: the lumbar spinal vertebrae (28 %), the sacrum (32 %), the pubic ramus (26 %), iliac crest (6 %), and femoral head (4 %). This distribution is consistent with the irradiated field that is currently used to deliver RT for uterine cervical cancer and would be different after RT delivered to other locations in the pelvis.
In most cases the fracture is transiently painful and pain resolves after a short rest period. However, in some patients, the pain persists because the fracture has not healed. Typically, the pain improves during rest periods and significantly worsens upon movement. In these cases, fracture fixation is required. Surgery is the standard of care for fracture stabilization, especially if an anatomic reduction is required. However several authors have described that PO is a very effective alternative for stabilizing non-displaced pelvic fractures directly while avoiding the complications and extensive exposure of open surgery [3, 12]. Moreover, due to the accuracy provided by CT and C-arm guidance, the rate of screw malpositioning is extremely low [5, 6, 21, 22]. In this study, we performed stabilization of the fracture line using osteosynthesis without cementoplasty. However, we believe that a small amount of cement could be injected around the tip of the screw in order to avoid any backward dislodgement, especially in bone-insufficiency patients.
A pathologic fracture is a significant risk for patients afflicted with osteolytic metastases. However, little is known about the natural behaviour of impending pathologic fractures without preventive consolidation, especially in the case of osteolytic metastases located in the iliac crest. In our clinical practice, we consider that the risk is high enough to justify preventive consolidation when the diameter of the metastasis exceeds 4 cm, especially if cortical disruption is associated. However, to our knowledge, no data exist in the literature to support our criteria. More data have been published concerning the risk of fracture due to osteolytic metastases located in the proximal femur. According to Mirel’s recommendation (Table 1), prophylactic fixation is highly indicated when the overall lesion score is 8 or greater [16]. This is why we use this inclusion criterion. The estimated risk of fracture for a Mirel score of 8 is 15 % and is over 33 % for a Mirel score of 9 or higher. Other authors state that the risk of fracture is high (between 63 % and 86 %) [15, 18] when the osteolytic metastasis is associated with 30-mm-wide or more cortical disruption.
It is noteworthy that all the patients were discussed at a multidisciplinary team meeting. Open surgery remains the gold standard for prophylactic consolidation of impending pathologic fractures, especially of the proximal femur. However, deciding whether or not to perform open surgery in cancer patients is difficult because the indication must take into account the general status of the patient, the prognosis of their cancer disease and ongoing chemotherapy. Consequently, many patients are not candidates for surgery. Furthermore, the risk incurred by surgery is sometimes too high compared to the estimated risk of a fracture or to the intensity of the pain. In these cases, less invasive procedures are warranted. Cementoplasty was the first option. The injection of cement into the osteoporotic fracture or into the osteolytic metastasis has demonstrated a huge benefit for pain palliation [23–25]. However, cementoplasty has two major drawbacks. The first one is that cement leakage could occur in soft tissue or in the adjacent joint. This is particularly true when cement is injected into a fracture or into an osteolytic metastasis with cortical disruption. In contrast, the insertion of a screw is completely predictable and controllable. In addition, the screw can be easily unscrewed if the position is not correct at 3D imaging during the procedure [26]. The second drawback of cementoplasty is that the strengthening properties of the cement are strong in cases of compression but weak for tensile or shear stresses [10, 15]. This explains why cementoplasty is only appropriate for the consolidation of osteolytic metastases located in the vertebral body and in the acetabulum. To our knowledge, no data in the literature support a benefit gained with cementoplasty for prophylactic consolidation of impending pathologic fractures located elsewhere. Nevertheless, we strongly believe that cementoplasty remains a good way to consolidate many osteolytic metastases, especially when there is no cortical rupture. Actually, the decision to perform cementoplasty alone or in association with PO is not established yet and prognostic scores of a fracture’s risks are warranted.
In conclusion, PO provides pain palliation for pathologic and bone-insufficiency fractures, as well as prophylactic consolidation of impending pathologic fractures due to osteolytic metastases. The technique should be included in the therapeutic arsenal as a minimally invasive procedure avoiding extensive surgical exposure and providing consolidation that significantly decreases the risk of fracture, with high technical success rates and a low complication rate.
References
Winkelhagen A, van den Bekerom MPJ, Bolhuis HW, Hogervorst M (2012) Preliminary results of cannulated screw fixation for isolated pubic ramus fractures. Strat Traum Limb Recon 7:87–91
Mosheiff R, Liebergall M (2002) Maneuvering the retrograde medullary screw in pubic ramus fractures. J Orthop Trauma 16:594–596
Routt ML Jr, Simonian PT, Grujic L (1995) The retrograde medullary superior pubic ramus screw for the treatment of anterior pelvic ring disruptions: a new technique. J Orthop Trauma 9:35–44
Asnis SE, Wanek-Sgaglione L (1994) Intracapsular fractures of the femoral neck. Results of cannulated screw fixation. J Bone Joint Surg Am 76:1793–1803
Reuther G, Rohner U, Will T, Dehne I, Petereit U. CT-guided screw fixation of vertical sacral fractures in local anaesthesia using a standard CT. Fortschr Röntgenstr. doi:10.1055/s-0034-1366605
Strobl FF, Haeussler SM, Paprottka PM, Hoffmann RT, Pieske O, Reiser MF et al (2014) Technical and clinical outcome of percutaneous CT fluoroscopy-guided screw placement in unstable injuries of the posterior pelvic ring. Skelet Radiol 43:1093–1100
Tsoumakidou G, Borensztein M, Zini C, Garnon J, Gangi A. Postablation insufficiency fracture of the iliac crest: management by percutaneous screw fixation. Cardiovasc Intervent Radiol. doi:10.1007/s00270-013-0781-1
Amoretti N, Huwart L, Hauger O et al (2013) Percutaneous Screw Fixation of Acetabular Roof Fractures by Radiologists Under CT and Fluoroscopy Guidance. AJR 200:447–450
Amoretti N, Hovorka I, Marcy PY, Hauger O, Amoretti ME, Lesbats V et al (2009) Computed axial tomography-guided fixation of sacroiliac joint disruption: safety, outcomes, and results at 3-year follow-up. Cardiovasc Intervent Radiol 32:1227–1234
Deschamps F, de Baere T (2012) Cementoplasty of bone metastases. Diagn Interv Imaging 93:685–689
Gay SB, Sistrom C, Wang GJ et al (1992) Percutaneous screw fixation of acetabular fractures with CT guidance: preliminary results of a new technique. AJR 158:819–822
Winkelhagen J, van den Bekerom MPJ, Bolhuis HW, Hogervorst M (2012) Preliminary results of cannulated screw fixation for isolated pubic ramus fractures. Strat Traum Limb Recon 7:87–91
Selvan VT, Oakley MJ, Rangan A et al (2004) Optimum configuration of cannulated hip screws for the fixation of intra- capsular hip fractures: a biomechanical study. Injury 35:136–141
Yih-Shiunn L, Chien-Rae H, Wen-Yun L (2007) Surgical treatment of undisplaced femoral neck fractures in the elderly. Int Orthop (SICOT) 31:677–682
Deschamps F, Farouil G, Hakime A, Barah A, Guiu B, Teriitehau C et al (2012) Cementoplasty of metastases of the proximal femur: is it a safe palliative option? J Vasc Interv Radiol 23:1311–1316
Mirels H (1989) Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res 249:256–264
Deschamps F, Farouil G, Hakime A, Teriitehau C, Barah A, de Baere T (2011) Percutaneous stabilization of impending pathological fracture of the proximal femur. Cardiovasc Intervent Radiol 35:1428–1432
Van der Linden YM, Dijkstra PD, Kroon HM et al (2004) Comparative analysis of risk factors for pathological fracture with femoral metastases. J Bone Joint Surg (Br) 4:566–573
Schmeler KM, Jhingran A, Iyer RB, Sun CC, Eifel PJ, Soliman PT et al (2010) Pelvic Fractures After Radiotherapy for Cervical Cancer. Cancer 116:625–630
Uezono H, Tsujino K, Moriki K, Nagano F, Ota Y, Sasaki R et al (2013) Pelvic insufficiency fracture after definitive radiotherapy for uterine cervical cancer: retrospective analysis of risk factors. J Radiat Res 54:1102–1110
Zwingmann J, Hauschild O, Bode G, Sudkamp NP, Schmal H (2013) Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: a systematic review and meta‐analysis. Arch Orthop Trauma Surg 133:1257–1265
Coste C, Asloum Y, Marcheix PS, Dijoux P, Charissoux JL, Mabit C (2013) Percutaneous iliosacral screw fixation in unstable pelvic ring lesions: The interest of O-ARM CT-guided navigation. Orthop Traumatol Surg Res 99S:S273–S278
Frey ME, DePalma MJ, Cifu DX, Bhagia SM, Daitch JS (2007) Efficacy and safety of percutaneous sacroplasty for painful osteoporotic sacral insufficiency fractures: a prospective, multicenter trial. Spine 32:1635–1640
Beall DP, D’Souza SL, Costello RF et al (2007) Percutaneous augmentation of the superior pubic ramus with polymethyl methacrylate: treatment of acute traumatic and chronic insufficiency fractures. Skelet Radiol 36:979–983
Marcy PY, Palussière J, Descamps B, Magné N, Bondiau PY, Ciais C et al (2000) Percutaneous cementoplasty for pelvic bone metastasis. Support Care Cancer 8:500–503
Fischer S, Vogl TJ, Marzi I, Zangos S, Wichmann JL, Scholtz JE et al (2015) Percutaneous cannulated screw fixation of sacral fractures and sacroiliac joint disruptions with CT-controlled guidewires performed by interventionalists: single center experience in treating posterior pelvic instability. Eur J Radiol 84:290–294
Acknowledgments
The authors thank Lorna Saint-Ange for editing this manuscript.
The scientific guarantor of this publication is Pr Thierry de Baere. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional review board approval was obtained. Written informed consent was waived by the institutional review board. The first 12 patients of this series have been previously reported in a published paper: "Percutaneous Stabilization of Impending Pathological Fracture of the Proximal Femur. Deschamps F, Farouil G, Hakime A, Teriitehau C, Barah A, de Baere T. Cardiovasc Intervent Radiol. 2011 Dec 28"
Methodology: retrospective, observational/performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Deschamps, F., de Baere, T., Hakime, A. et al. Percutaneous osteosynthesis in the pelvis in cancer patients. Eur Radiol 26, 1631–1639 (2016). https://doi.org/10.1007/s00330-015-3971-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3971-1