Abstract
Background
The neural plexus and lymph nodes around the superior mesenteric artery (LN#14), are the most frequent sites involved by pancreatic head cancer. However the influence of metastases to LN#14 on patients’ prognosis has rarely been evaluated.
Methods
The patients who underwent pancreatectomy for pancreatic head cancer between January 2010 and December 2018 were selected. The patients with nodal metastases were classified into an LN#14 + or LN#14−group according to LN#14 metastasis. Clinical and pathological characteristics and prognosis were compared between the two groups.
Results
In total, 99 patients underwent pancreatectomy. Ninety-four patients were positive for lymph node metastases and 14 and 80 were classified as LN#14 + and LN#14 − , respectively. Postoperative median overall survival (OS) of the LN#14 + and LN#14 − groups was 10.2 and 31.1 months, respectively (P < 0.001). Median OS of the LN#14 + group was worse than that of patients with ≥ 4 metastatic nodes in the LN#14 − group (n = 35, 24.7 months, P = 0.002). In multivariate analysis, LN#14 + (hazard ratio [HR] = 3.89, 95% confidence interval [CI], 1.64–8.86) was one of the independent predictors of worse OS.
Conclusion
It might be feasible to recognize LN#14 metastases as an important prognostic factor independently from other regional lymph node metastases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lymph node metastases are one of the most important prognostic predictors in patients with pancreatic cancer. Recently, the number of metastatic lymph nodes [1, 2] and metastatic lymph node ratio [3, 4], which can be more simply assessed than the sites of metastatic nodes, have been advocated as useful prognostic predictors. The current staging system of the Union for International Cancer Control (UICC) defines N1 and N2 as 1–3 and ≥ 4 metastatic regional lymph nodes, respectively [5]. However, only a few studies have evaluated the prognostic impact of the regions of nodal metastases [6,7,8,9].
Pancreatic cancer is likely to invade along nerve plexuses. In the surgical resection of pancreatic head cancer, usually by pancreaticoduodenectomy (PD), the plexus around the superior mesenteric artery (SMA) is the most frequent site of tumor exposure and results in R1 resection [10]. The importance of achieving an adequate resection margin by appropriate dissection of the nerve plexus around the SMA has been emphasized [11], whereas the influence of nodal metastases around the SMA on prognosis has rarely been evaluated. A previous study showed that there were several independent lymphatic pathways from the pancreatic head: one toward the nodes around the celiac trunk and another toward the SMA [12]. Other studies showed that all patients with para-aortic lymph node metastases had accompanying lymph node metastases around the SMA [13, 14]. These findings suggest that lymph node metastases around the SMA could be a preliminary step toward para-aortic nodal metastases.
The aim of the present study was to investigate the impact of lymph node metastases around the SMA on the prognosis of patients who underwent pancreatectomy for pancreatic head cancer.
Materials and methods
Patient selection and data collection
This study was conducted with the approval of the Institutional Review Board of the National Defense Medical College, Tokorozawa, Japan (No. 4115).
An institutional chart review was performed to select the patients who underwent pancreatectomy for pancreatic ductal adenocarcinoma in the pancreatic head between January 2010 and December 2018. The patients who underwent R2 resection were excluded. Resectability status was evaluated according to the National Comprehensive Cancer Network guidelines [15]. Tumor stages were recorded according to the 8th edition of the UICC staging system [5]. In addition to the number of harvested and metastatic lymph nodes, the sites of metastatic lymph nodes were recorded according to the definition of the Japanese Pancreas Society [16]. By this definition, each group of lymph nodes is numbered as follows: anterior surface of the pancreatic head, LN#17; posterior surface of the pancreatic head, LN#13; along the common hepatic artery, LN#8; along the hepatoduodenal ligament, LN#12; and along the SMA, LN#14. To evaluate the impact of metastases to LN#14, the patients with and without LN#14 metastases were classified as LN#14 + and LN#14 − , respectively.
Preoperative chemotherapy
The patients with resectable disease underwent upfront surgery except for a few patients who were enrolled in a clinical study to evaluate the effect of neoadjuvant chemotherapy (Prep-02/JSAP05) [17]. The patients with borderline resectable and unresectable disease received preoperative chemotherapy, but a few patients underwent upfront surgery according to the attending physicians’ decision.
Surgical procedure
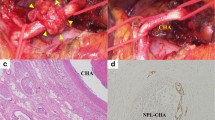
Preoperatively, PD was indicated in all patients. After laparotomy para-aortic lymph node sampling was performed only when metastases was suspected by preoperative imaging or by intraoperative findings. Pathological examination of frozen sections of the pancreatic stump was routinely performed. If tumor invasion was positive, additional pancreatic resection was performed, resulting in total pancreatectomy (TP) in a few patients with extensive tumor spread. All patients underwent regional lymph node dissection, including LN#8, LN#12, LN#13, LN#14 and LN#17. We routinely dissect LN#14 only in the right side of the SMA preserving the nerve plexus around it (PLsma) [16] unless the tumor invasion was suspected by preoperative imaging assessment or by intraoperative findings.
Pathologic evaluation of surgical specimens
Basically we performed lymph node dissection in en bloc manner. The dissected lymph nodes in the specimen were separated according to each lymph node station. We also used schematic drawing of the resected specimen to inform the pathologist of the sites of nodes dissected. Based on these information, the pathologists investigated the lymph node metastases.
Postoperative follow-up
Postoperative adjuvant chemotherapy with S-1 or gemcitabine was performed as long as it was tolerable to the patients’ condition. Each patient was followed up every 3–6 months with blood examinations, including carbohydrate antigen 19–9 level and contrast-enhanced computed tomography. For survival analyses, the last follow-up date was July 31, 2020.
Statistical analysis
Continuous data were expressed as median and range and compared by Wilcoxon’s rank-sum test. Categorized variables were compared using the chi-square test or Fisher’s exact test. Recurrence-free survival (RFS) and overall survival (OS) were estimated using the Kaplan–Meier method, and differences in survival curves were compared using the log-rank test. Univariate analyses of OS were performed by log-rank test, and multivariate analyses were performed using a Cox proportional-hazards model. P ≤ 0.050 was considered statistically significant. All the statistical analyses were performed using JMP software version 9.0.0 (SAS Institute Inc., Cary, NC, USA).
Results
Patient characteristics
During the study period, 145 patients underwent pancreatectomy for pancreatic ductal adenocarcinoma. Among them 43 patients with pancreatic body or tail adenocarcinoma and other three patients who had distant metastasis were excluded. The remaining 99 patients were selected for this study. The median age was 70 years (range 48–92 years) and 49 patients (49%) were male. Resectability status was resectable, borderline resectable, and unresectable in 73 (74%), 15 (15%), and 11 (11%) patients, respectively. Preoperative chemotherapy was performed in 23 patients (23%), eight in resecteble, eight in borderline resectable and seven in unresectable disease, respectively. The primary regimen according to the resectability status is summarized in Table 1. Ninety-two patients (93%) underwent PD and the remaining seven patients (7%) underwent TP as a result of additional pancreatic resection. Portal/superior mesenteric vein and/or hepatic/superior mesenteric artery reconstruction was required in 25 (34%), 11 (73%) and 11 (100%) patients with resectable, borderline resectable and unresectable disease, respectively. R0 resection was achieved in 74 patients (75%). Postoperative adjuvant chemotherapy was performed in 71 patients (72%). The primary regimen was S-1 in 60 (85%) patients, gemcitabine in 10 (14%), and gemcitabine plus S-1 in one (1%).
Metastatic lymph nodes
The median number of dissected lymph nodes was 33 (range, 12–91). Pathological lymph node metastases were observed in 94 patients (95%), and 49 and 45 patients were classified as N1 and N2, respectively. Figure 1 shows the number of patients with metastases to each site of regional lymph nodes. LN#13 metastases were most frequent, followed by LN#17, LN#14, LN#8 and LN#12. In 94 patients with node metastases, the median number of dissected nodes and metastatic nodes was 33 (range 12–91) and three (range 1–18), respectively. The median metastatic lymph node ratio was 0.10 (range 0.02–0.57). All patients with LN#8, LN#12 or LN#14 metastases had accompanying metastases to LN#13 and/or LN#17, except in one patient with LN#12 metastases and another with direct invasion of the primary tumor to LN#14. One of eight patients (13%) with LN#12 metastases and three of 14 (21%) with LN#14 metastases had accompanying LN#8 metastases, whereas no patient had metastases to both LN#12 and LN#14 (Fig. 2).
Number of patients with metastases to each site of regional lymph nodes. Abbreviations: CeA Celiac trunk; SpA Splenic artery; CHA Common hepatic artery; PHA Proper hepatic artery; GDA Gastroduodenal artery; SMA Superior mesenteric artery; PV Portal vein; SMV Superior mesenteric vein; CBD Common bile duct
Univariate and multivariate analyses of predictors of worse OS
Table 2 shows the univariate and multivariate analyses of the predictors of worse OS in 94 patients with node metastases. Postoperative median follow-up period was 52 months. Sixty-four patients (68%) died during the study periods. According to the univariate analysis, LN#14 metastases (median OS, LN#14 + vs. LN#14 − , 10.2 vs. 31.1 months, P < 0.001), tumor differentiation, R status, T status, N status, and metastatic lymph node ratio were significant. Regarding the sites of lymph node metastases, only LN#14 was a significant predictor. The multivariate analysis revealed that tumor differentiation grade of “not well” (hazard ratio [HR] = 2.39; 95% confidence interval [CI], 1.21–5.33; P = 0.011), R1 resection (HR = 2.77; 95% CI, 1.44–5.17; P = 0.003), and LN#14 metastases (HR = 3.89; 95% CI, 1.64–8.86; P = 0.002) were independent predictors. N status (N2 vs. N1) and metastatic lymph node ratio > 0.2 did not remain as independent predictors.
Figure 3 shows the RFS and OS of patients with LN#14 + , LN#14 − and N1 (LN#14 − /N1), and LN#14 − and N2 (LN#14 − /N2). Both RFS and OS were comparable between the LN#14 − /N1 and LN#14 − /N2 groups (median RFS, 16.1 vs. 11.0 months, P = 0.084; median OS, 34.3 vs. 24.7 months; P = 0.123). RFS and OS of the LN#14 + group were significantly worse than those of the LN#14 − /N2 group (median RFS, 8.8 vs. 11.0 months; P = 0.025; median OS, 10.2 vs. 24.7 months; P = 0.002).
Factors associated with LN#14 metastases
Table 3 shows the comparison of clinical and pathological factors between patients in the LN#14 + and LN#14 − groups. Tumor size was larger in the LN#14 + group than in the LN#14 − group, with a statistically marginal difference (P = 0.073). The difference in the proportion of patients with N2 status was also marginal (P = 0.056). Pathological invasion to the portal venous system was more frequently observed in the LN#14 + group (P = 0.006), while the proportion of patients with PLsma invasion was comparable (P = 0.938). R1 resection rate was significantly higher in the LN#14 + group (P = 0.038).
Eleven and 60 patients in the LN#14 + and LN#14 − groups, respectively, showed tumor recurrence. Peritoneal dissemination and liver metastases were the most frequent initial recurrence sites in the LN#14 + and LN#14 − group, respectively. Four patients in the LN#14 − group showed both peritoneal dissemination and liver metastases. The frequency of peritoneal dissemination was significantly higher in the LN#14 + group (n = 5) than LN#14 − group (n = 9) (P = 0.020) (Fig. 4).
Discussion
The present study showed the impact of LN#14 metastases on the postoperative prognosis of the patients with pancreatic head cancer. Since the proportion of PV system invasion and R1 resection was higher in the LN#14 + group and it might have influenced their prognosis, LN#14 metastasis itself was one of the independent poor prognostic predictors. And it was notable that only LN#14 metastases were associated with significantly poor prognosis among lymph node positive patients. Several previous studies showed the prognostic impact of LN#8 metastases, with controversial results. Cordera et al. and LaFemina et al. showed that LN#8 metastases were a negative prognostic factor in patients who underwent PD for pancreatic head cancer [6, 8]. In contrast, Philips et al. and Paiella et al. showed no difference in the OS between patients with and without LN#8 metastases [7, 9]. Most previous studies evaluated the impact of LN#8 metastases on prognosis because LN#8 was routinely and easily dissected during PD. To the best of our knowledge, the present study was the first to show the influence of LN#14 metastases on the prognosis of patients with pancreatic head cancer. Furthermore, our multivariate analysis showed that LN#14 metastases rather than other regional node metastases including LN#8, N2 status, and metastatic lymph node ratio > 0.2 were independent prognostic predictors. Both RFS and OS of the patients with LN#14 + were significantly worse than those in patients with LN#14 − /N2. Recent studies showed that the number of metastatic nodes or metastatic lymph nodes ratio more precisely reflected prognosis than the sites of metastatic nodes [18]. However, the present results suggested that the region of metastatic lymph nodes, or at least LN#14 metastases, should also be regarded as an important prognostic factor. One drawback of evaluation by metastatic node number or ratio is that it depends on the number of nodes harvested. If the number of harvested nodes is insufficient, the number of metastatic lymph nodes could potentially be underestimated, and in contrast, the metastatic lymph node ratio might be overestimated.
Several randomized controlled studies have shown no clinical benefit of extended lymphadenectomy and nerve plexus dissection, including complete dissection of LN#14, for patients with pancreatic cancer [19,20,21,22]. Nevertheless, both UICC and the Japanese Pancreas Society staging include LN#14 as regional lymph nodes [5, 16]. Previous studies showed a higher incidence of LN#14 metastases (2%–43%) compared with LN#8 (8%–17%) or LN#12 (2%–19%) metastases in patients with pancreatic head cancer [9, 21, 23]. In these studies, the association of nodal metastases in each region with the incidence of para-aortic lymph node metastases was referred to, but their influence on patients’ prognosis was not evaluated. The present study similarly showed higher incidence of LN#14 metastases than other regional lymph node metastases, including LN#8 or LN#12, and showed the relationship of the incidence of metastases among each group of regional lymph nodes, and evaluated their impact on postoperative prognosis. It was notable that there was no patient with simultaneous metastases to LN#14 and LN#12. Although there was no patient with para-aortic lymph node metastases in our series, the results confirm the previous suggestion that the lymphatic pathway toward the SMA, but not the celiac trunk, is more likely to lead to further distant metastases outside the regional lymph nodes, including the para-aortic nodes [13, 14]. The higher incidence of peritoneal dissemination in the LN#14 + group may also reflect this theory.
Currently the adjuvant chemotherapy following the surgical resection of pancreatic cancer is strongly recommended in the National Comprehensive Network guideline [15] as well as the Japanese guideline [24]. While it was still controversial about recommended regimen, we chose S-1 as the first treatment regimen according to the JASPAC 01 trial [25]. We do not change the treatment regimen according to the recurrence risk factors. In the present study we showed LN#14 metastases was one of the poor prognostic factors other than other lymph node station metastases. Although it was still debated whether the choice of adjuvant chemotherapy regimen should change according to the recurrence risk factors, the present study might suggest that more strong chemotherapy regimen would be feasible in the patients with LN#14 metastases.
The International Study Group on Pancreatic Surgery guidelines propose dissection of only the right side of the SMA as standard lymphadenectomy [26]. The current UICC classification also defines the lymph nodes along the right lateral wall of the SMA as the regional nodes [5]. Most patients in our series underwent LN#14 dissection only along the right side of the SMA. Therefore, we could not evaluate the benefit of complete dissection of LN#14 around the SMA. A recent study by Okada, et al. showed the negative impact of LN#14 metastases in the left side of SMA on the postoperative prognosis in the patients with pancreatic head cancer [27]. However, the left side of SMA is usually out of routine lymph node dissection in pancreaticoduodenectomy. Most of the positive LN#14 in our series were located on the right side of SMA, therefore, our study was different from Okada’s study in suggesting that metastases of LN#14 should be discriminated from metastases to other regional lymph nodes. On the other hand, it would be still controversial whether LN#14 metastases should be considered as contraindication of further surgical resection or as a criterion to choose more stronger adjuvant chemotherapy regimens.
In our series, LN#14 metastases were not correlated with PLsma invasion, which is commonly presented as a prognostic predictor. Makino et al. reported that PLsma invasion was strongly associated with tumor location [28]. The extrapancreatic nerve invasion is a common infiltration pattern of pancreatic cancer. Thus, it would be expected that tumors located near the SMA frequently show PLsma invasion. However, the sites of lymph node metastases depend on the lymphatic pathway as well as tumor location [13]. Our comparable incidence of LN#14 metastases in patients with tumors in the uncinate process and in other areas of the pancreatic head suggests that the pathway of lymph node metastases and direct nerve plexus invasion should be discriminated. Both the LN#14 metastases and PLsma invasion were important for prediction of patients’ prognosis.
The present study had several limitations. First, this was a retrospective study, and it was natural that there was a difference in patients’ background and pathological profiles between the LN#14 + and LN#14 − groups. Pathological portal vein invasion and R1 resection were more frequent in the LN#14 + group. However, this might reflect the more advanced stage of pancreatic cancer with LN#14 metastases, and it should be noted that LN#14 + was an independent prognostic predictor in multivariate analysis. Second, the number of patients and the incidence of each regional lymph node metastases were small. Therefore, the impact of metastases, especially to LN#8 or LN#12, might have been underestimated. Third, we included patients who received chemotherapy before surgery, and the influence of chemotherapy on the lymph node metastases was not considered. In addition, the chemotherapy regimen was not unified and old regimens such as gemcitabine and/or S-1 were included. These factors might have affected the incidence of node metastases or prognosis.
Conclusion
In conclusion, the present study suggested that metastases to LN#14 in particular were associated with worse prognosis than metastases to other regional lymph nodes.
References
Murakami Y, Uemura K, Sudo T et al (2010) Number of metastatic lymph nodes, but not lymph node ratio, is an independent prognostic factor after resection of pancreatic carcinoma. J Am Coll Surg 211:196–204
Strobel O, Hinz U, Gluth A et al (2015) Pancreatic adenocarcinoma: number of positive nodes allows to distinguish several N categories. Ann Surg 261:961–969
Slidell MB, Chang DC, Cameron JL et al (2008) Impact of total lymph node count and lymph node ratio on staging and survival after pancreatectomy for pancreatic adenocarcinoma: a large, population-based analysis. Ann Surg Oncol 15:165–174
Zhan HX, Xu JW, Wang L et al (2015) Lymph node ratio is an independent prognostic factor for patients after resection of pancreatic cancer. World J Surg Oncol 13:105
Brierley J D, Gospodarowicz M K,Wittekind C. (2017) In: International Union Against Cancer (UICC). TNM Classification of Malignant Tumors, Wiley, New York.
Cordera F, Arciero CA, Li T et al (2007) Significance of common hepatic artery lymph node metastases during pancreaticoduodenectomy for pancreatic head adenocarcinoma. Ann Surg Oncol 14:2330–2336
Philips P, Dunki-Jacobs E, Agle SC et al (2014) The role of hepatic artery lymph node in pancreatic adenocarcinoma: prognostic factor or a selection criterion for surgery. HPB (Oxford) 16:1051–1055
LaFemina J, Chou JF, Gonen M et al (2013) Hepatic arterial nodal metastases in pancreatic cancer: is this the node of importance? J Gastrointest Surg 17:1092–1097
Paiella S, Malleo G, Maggino L et al (2015) Pancreatectomy with para-aortic lymph node dissection for pancreatic head adenocarcinoma: pattern of nodal metastasis spread and analysis of prognostic factors. J Gastrointest Surg 19:1610–1620
Raut CP, Tseng JF, Sun CC et al (2007) Impact of resection status on pattern of failure and survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. Ann Surg 246:52–60
Inoue Y, Saiura A, Yoshioka R et al (2015) Pancreatoduodenectomy with systematic mesopancreas dissection using a supracolic anterior artery-first approach. Ann Surg 262:1092–1101
Deki H, Sato T (1988) An anatomic study of the peripancreatic lymphatics. Surg Radiol Anat 10:121–135
Kayahara M, Nagakawa T, Kobayashi H et al (1992) Lymphatic flow in carcinoma of the head of the pancreas. Cancer 70:2061–2066
Nagakawa T, Kobayashi H, Ueno K et al (1994) Clinical study of lymphatic flow to the paraaortic lymph nodes in carcinoma of the head of the pancreas. Cancer 73:1155–1162
; Available from: National Comprehensive Cancer Network. NCCN practice guidelines for pancreatic cancer, version 2. Available at http://www.nccn.org/professionals/physician_gls/default.aspx.
Society J P. In: Classification of Pancreatic Carcinoma, Kanehara & Co. Ltd, Tokyo.
Motoi F, Kosuge T, Ueno H et al (2019) Randomized phase II/III trial of neoadjuvant chemotherapy with gemcitabine and S-1 versus upfront surgery for resectable pancreatic cancer (Prep-02/JSAP05). Jpn J Clin Oncol 49:190–194
Yamada S, Fujii T, Hirakawa A et al (2016) Lymph node ratio as parameter of regional lymph node involvement in pancreatic cancer. Langenbecks Arch Surg 401:1143–1152
Pedrazzoli S, DiCarlo V, Dionigi R et al (1998) Standard versus extended lymphadenectomy associated with pancreatoduodenectomy in the surgical treatment of adenocarcinoma of the head of the pancreas: a multicenter, prospective, randomized study. Lymphadenectomy Study Group Ann Surg 228:508–517
Farnell MB, Pearson RK, Sarr MG et al (2005) A prospective randomized trial comparing standard pancreatoduodenectomy with pancreatoduodenectomy with extended lymphadenectomy in resectable pancreatic head adenocarcinoma. Surgery. 138:618–628 (discussion 628-630)
Nimura Y, Nagino M, Takao S et al (2012) Standard versus extended lymphadenectomy in radical pancreatoduodenectomy for ductal adenocarcinoma of the head of the pancreas: long-term results of a Japanese multicenter randomized controlled trial. J Hepatobiliary Pancreat Sci 19:230–241
Jang JY, Kang MJ, Heo JS et al (2014) A prospective randomized controlled study comparing outcomes of standard resection and extended resection, including dissection of the nerve plexus and various lymph nodes, in patients with pancreatic head cancer. Ann Surg 259:656–664
Sakai M, Nakao A, Kaneko T et al (2005) Para-aortic lymph node metastasis in carcinoma of the head of the pancreas. Surgery 137:606–611
Society J P (2019) In: Clinical Practice Guidelines for Pancreatic Cancer 2019. Kanehara & Co., Ltd, Tokyo
Uesaka K, Boku N, Fukutomi A et al (2016) Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet 388:248–257
Tol JA, Gouma DJ, Bassi C et al (2014) Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the international study group on pancreatic surgery (ISGPS). Surgery 156:591–600
Okada K, Murakami Y, Kondo N et al (2019) Prognostic significance of lymph node metastasis and micrometastasis along the left side of superior mesenteric artery in pancreatic head cancer. J Gastrointest Surg 23:2100–2109
Makino I, Kitagawa H, Ohta T et al (2008) Nerve plexus invasion in pancreatic cancer: spread patterns on histopathologic and embryological analyses. Pancreas 37:358–365
Acknowledgements
We thank Cathel Kerr, BSc, PhD, from Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miyata, Y., Yonamine, N., Fujinuma, I. et al. Impact of Lymph Node Metastases Around the Superior Mesenteric Artery on Postoperative Outcomes of Pancreatic Head Cancer. World J Surg 45, 3668–3676 (2021). https://doi.org/10.1007/s00268-021-06276-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06276-0