Abstract
Background
Incisional hernias have an impact on patients’ quality of life and on health care finances. Because of high recurrence rates despite mesh repair, the prevention of incisional hernias with prophylactic mesh reinforcement is currently a topic of interest. But only 15% of surgeons are implementing it, mainly because of fear for mesh complications and disbelief in the benefits. The goal of this systematic review is to evaluate the effectiveness and safety of prophylactic mesh in adult patients after midline laparotomy.
Methods
An extensive literature search was performed in PubMed, Embase and CENTRAL until 9/5/2020 for RCTs and cohort studies regarding mesh reinforcement versus primary suture closure of a midline laparotomy. The quality of the articles was analyzed using the Scottish Intercollegiate Guidelines Network checklists. Revman 5 was used to perform a meta-analysis.
Results
Twenty-three articles were found with a total of 1633 patients in the mesh reinforcement group and 1533 in the primary suture group. An odds ratio for incisional hernia incidence of 0.37 (95% CI = [0.30, 0.46], p < 0.01) with RCTs and of 0.15 (95% CI = [0.09,0.25], p < 0.01) in cohort studies was calculated. Seroma rate shows a significant odds ratio of 2.18 (95% CI = [1.45, 3.29], p < 0.01) in favor of primary suture. No increase was found regarding other complications.
Conclusion
The evidence for the use of prophylactic mesh reinforcement is overwhelming with a significant reduction in incisional hernia rate, but implementation in daily clinical practice remains limited. Instead of putting patients at risk for incisional hernia formation and subsequent complications, surgeons should question their arguments why not to use mesh reinforcement, specifically in high-risk patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abdominal wall hernias have a negative impact on patient’s quality of life. They might cause pain, obstruction, incarceration (6–15%), strangulation (2%) as well as aesthetic complaints [1,2,3,4]. Furthermore, they have financial consequences for both patient and society. The average additional medical expenditure for patients that do develop incisional hernias (IH) versus patients that don’t, is between $21,211 and $28,870 [5].
Incisional hernias occur in 2–50% of the patients that underwent open midline laparotomy and even in 70% in high-risk patients. Obesity and connective tissue disorders are the most important risk factors, but more are identified, like COPD, chronic steroid use and infection [6,7,8,9]. Recurrence rates of 25–63% after primary suture (PS) repair and 11–32% for mesh repair still apply [10, 11]. Because of these high recurrence rates, the prevention of incisional hernias with prophylactic mesh reinforcement (PMR) might have a great impact. Although about 89% of surgeons are familiar with the current literature, the most frequent reason why surgeons are reluctant to use prophylactic mesh, is fear for mesh infection and complications. [12]. Infection may lead to chronic wound problems, subsequent mesh removal and lowers the success rate of a later hernia repair [11]. Also a slight increase in operation time is considered with a mean of 15 min [3, 13]. Other reasons why they are rather skeptical regarding potential benefits of PMR are unfamiliarity with the surgical technique and financial loss [12].
After discussion with the patient, the best location of the mesh might be questioned too. Both sublay and onlay mesh position are widely used in abdominal wall reconstruction. The onlay position is easier to perform, but needs creation of larger skin flaps. The sublay position is more technically demanding, but is physiological, shows low recurrence and decreased SSI rates in hernia repair [14].
Because of this ongoing debate about the pros and cons of mesh reinforcement, as well as the difficult implementation in daily practice by general surgeons, this review tries to summarize the current evidence on prophylactic mesh placement after midline laparotomy.
Material and methods
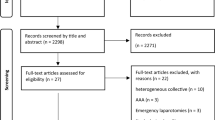
An extensive literature search was performed in PubMed, Embase and Cochrane Central Register of Controlled Trials (CENTRAL) until 9/5/2020 for RCT’s and cohort studies (Fig. 1 [15]). Following MeSH-terms were used: Surgical Mesh, Hernia, Abdominal OR Hernia, Ventral OR Hernia, Umbilical (prevention and control), Midline laparotomy, Obesity and Aortic Aneurysm, Abdominal. Other relevant articles were also selected from review citations. This was performed by 2 independent reviewers (D.M., B.F.). In a first-level screening, only studies about prophylactic use of meshes in laparotomy in humans were screened for. Studies concerning parastomal, inguinal and hernia repair were excluded. In a second-level screening, the quality of the articles was analyzed using the checklists of the Scottish Intercollegiate Guidelines Network (SIGN) [16,17,18]. Low quality studies were excluded. Data were extracted in an extraction sheet, similar to Tables 1 and 2. The primary outcome is the effect on the incidence of incisional hernias. The secondary outcomes are complications as seroma, infection and chronic pain.
PRISMA for studies concerning IH prevention after laparotomy [15]
The PMA group was selected as intervention group and the PS group as the control group. Patient demographic similarity was reported in the studies. A fixed-effect model was used to pool data. The outcomes were dichotomous, and odds ratios were calculated with the Mantel–Haenszel method with a 95% confidence interval. Subgroup analysis was performed with studies that reported infection rate, seroma rate and chronic pain assessment. Heterogeneity was assessed with Chi2 and I2. p < 0.05, and I2 > 50% heterogeneity was seen as significant heterogeneity. This was performed using Review Manager 5 (The Cochrane Collaboration, Copenhagen). The research is being reported in line with the guidelines of Moher et al. [15] and Probst et al. [19].
Results
In total, 23 articles were found regarding PMR: 17 studies are RCTs, and 6 are cohort studies. Two articles report on long-term results of previously published data by the same authors. Fifteen studies have high quality, and 8 have acceptable quality according to SIGN-checklist [16,17,18]. The studies include a total of 1633 patients in the PMR group and 1533 in the PS group. The characteristics of the included studies can be found in Table 1, while the results are summarized in Table 2.
The design of most studies is comparable for both PMR and PS closing techniques after midline laparotomy. All but one [20] used slowly- or non-absorbable running sutures. Ten authors mentioned recommending a suture length-to-wound length ratio of 4:1 but this was never measured [21]. Ten authors reported closing with a 1 cm distance between stiches and 1 cm distance to the fascial border. Others mentioned standard fascia closure without specifying the technique. Note that currently smaller bites of 0.5 cm are recommended, the so-called small bites, small steps technique [21, 22]. Nine out of the 23 authors used sublay, 11 used onlay, 1 both sublay and onlay, 1 inlay and 1 intraperitoneal mesh placement. Four studies used biological mesh, while all others used a synthetic polypropylene mesh. The most important differences between studies concern both methodology and duration of follow-up. Subgroup analysis of different techniques could not be properly performed because of lack of adequate data.
The meta-analysis including all RCTs shows a difference in incisional hernia formation of 13.6% for the PMR group versus 28.1% for the PS group with a significant odds ratio (OR) of 0.37 (95% CI = [0.30, 0.46] (Fig. 2). The risk ratio of having an incisional hernia when implementing PMR in comparison of PS is 0.46, (95% CI = [0.38, 0.55]). (Table 3) There was a significant statistical heterogeneity of 64% between the studies. The cohort studies also show a significant odds ratio of 0.15 (95% CI = [0.09,0.25]) (Fig. 3) without heterogeneity.
Fourteen RCTs and five cohort studies published data on infection, both superficial, deep and mesh infection. There was no difference in overall infection in RCTs (OR = 1.00, 95% CI = [0.74, 1.35]) (Fig. 4) and cohort studies (OR = 1.19, 95% CI = [0.76, 1.86]). (Fig. 5) Twelve RCTs reported data on seroma and showed significantly more seroma formation in the PMR group than in the PS group (OR = 2.18, 95% CI = [1.45, 3.29]). (Fig. 6) The cohort studies could not be analyzed for this complication due to insufficient data. Only 5 studies reported the treatment of seromas [7, 9, 23,24,25]. Out of 75 seromas reported, only 1 was reoperated because of suspicion of infection. All others were treated non-surgically, with or without percutaneous drainage. Only 6 RCTs investigated chronic pain, with a significant increase in the PMR group with an OR of 1.68 (95% CI = [1.02, 2.76]), without heterogeneity (Fig. 7).
Discussion
Post-operative incisional hernias are an important health care problem and can result in high morbidity and even mortality. Risk factors like obesity and AAA can raise the risk to 70% after laparotomy. However, IHs appear to generate little interest: at the end of an operation ‘closing time’ is sometimes viewed as ‘coffee time’ or is done by less experienced and trained surgical residents [26]. Various solutions have been advocated, such as closure using a small bite technique and prophylactic mesh reinforcement (PMR) [27]. Awareness as well as debate regarding the use of prophylactic mesh have now gained more attention, but implementation is still very low [12]. Prevention of IH formation may however benefit QoL as well as reduce health care costs. In this systematic review, we analyzed the currently available literature, evaluating specific possible arguments for surgeons not to implement mesh prophylaxis after midline laparotomy.
Although 80% of the surgeons around the world use specific suturing techniques for hernia prevention, only 15% reported using prophylactic mesh. 11% of the surgeons are not familiar with the literature while 12% admit not to have the surgical knowledge for applying mesh insertion, neither onlay nor sublay positioning. Raising awareness and provide surgical videos are necessary as this should not be the reason not to apply a superior technique [12].
During the survey by Fisher and colleagues, 23% of the surgeons are not convinced of the efficacy [12]. But PMR significantly reduces IH formation, as an odds ratio (OR) for IH incidence of 0.37 (95% CI = [0.30, 0.46] with RCTs and of 0.15 (95% CI = [0.09, 0.25]) in cohort studies was calculated. Encouraging results for intraperitoneal mesh reinforcement showed a 17% incisional hernia rate versus 39% in the primary closure group after 2 years’ follow-up (P < 0.001) [28, 29], while the PRIMA trial randomized 480 high-risk patients to 3 treatment arms: primary suture, onlay, and sublay [30]. At 2 years’ follow-up, there was 33/107 (30%) IHs in the suture-only group, 25/188 (13%) in the onlay mesh-reinforcement group and 34/185 (18%) in the sublay-reinforcement group (onlay vs primary suture P = 0.0016; sublay vs primary suture P = 0.05).
In high-risk patients, like obese patients and patients with AAA, even a bigger decrease can be expected. According to Jairam et al. [7] and Argudo et al. [31], a BMI higher than 27 kg/m2 or 29 kg/m2, respectively, seems a good indication for PMR. Although the clinically heterogeneity is limited and a graphical evaluation of the forest plot shows that all studies favor PMR, there is a statistical heterogeneity between RCTs (I2 = 62%). The heterogeneity originates from four studies specifically Sarr et al. [13], Caro-Tarrago et al. [24], Muysoms et al. [25], Pans et al. [20], but no specific reasons could be identified.
The European Hernia Society did not yet recommend PMR in their guidelines [32]. But since then many publications suggest the use of mesh to prevent IH after abdominal surgery. Three mesh locations have been studied to reinforce fascial closure of midline wounds. [33] Available evidence indicates that all 3 seem effective in reducing IH formation. A RCT by Jairam et al [8]. reported better IH prevention with onlay placement in comparison with sublay. Also the simplicity of the onlay procedure is an advantage. Data concerning intraperitoneal and inlay mesh reinforcement are scarce.
46.9% of the surgeons are concerned about mesh infection and other mesh-related complication. This seems actually to be the main reason not to implement prophylactic mesh use in their routine practice [12]. Looking at the outcome of this systematic review, the risk of SSI is equal with versus without PMR. If an infection occurs, a mesh removal is not always necessary. Two articles reported the necessity of mesh removal in 1.6% and 6.7%, while the other articles reported no mesh removals. Garcia-Urena et al. [34]. included both elective and emergency colorectal operations without hemodynamic instability of the patient during the operation. A total of 107 patients were included, with clinical and radiological follow-up for 24 months. There was no significant difference in surgical site infection between the suture-only group (33.3%) and the suture-plus-mesh group (18.9%).
Onlay and sublay mesh reinforcement show an increased risk of seroma formation, though this is not usually a significant clinical problem. A doubling of seroma rate to 10.4% is found when using mesh. Jairam et al. [8] reported a significant increase of seroma when the onlay approach is used in comparison with the sublay approach.
PMR also presented a slightly increased risk of chronic wound pain compared with primary suture [35]. An OR of 1.68 was found in this analysis, which was borderline significant. The risk increased from 7.0 to 10.7%. However, it has to be mentioned that Sarr et al. [13] was accountable for 69% of the weight in this analysis, showing chronic pain in 32 out of 185 patients after PMR using a bioprosthesis. Only two studies reporting chronic pain, used a sublay technique. These two studies show an OR of 2.93 (95% CI = [0.46, 18.67]) [25, 36]. The role of mesh fixation considering chronic pain remains unclear. Data on mesh fixation in PMR are scarce: only 2 retrospective studies show a safe implementation and possible reduction of chronic pain with fibrin sealant [37, 38].
Additional mesh costs and increased operating time might be another argument not to implement PMR in daily clinical practice. However, Fischer et al. [39] performed a cost-effectiveness analysis of PMR in high-risk patients with 719 included patients. A dominant incremental cost-effectiveness ratio (ICER) of $42,444/QALY was found. In a Monte Carlo sensitivity analysis, a proportion of 11.5% showed that PMR was dominant to primary suturing and a proportion of 36.2% showed that PMR lays under the $50,000/QALY threshold. This threshold might increase to $91,318 in Belgium, following the guidelines of the World Health Organization [40]. Argudo et al. [31] chose to implement mesh reinforcement in patients with a HERNIAscore higher than 7 (HERNIAscore = 4 × 1 (= laparotomy) + 3 × 0 (= no hand-assisted laparoscopy) + 1 × COPD + 1 × BMI > 25). The primary outcome was mean cost. They saw a significant reduction in total cost (10,057€ vs. 10,921€, p < 0.001) using an algorithm for patient selection, especially in obesity (10,210€ vs 13,588€, p < 001), but not in low risk patients (9,226€ vs. 10,279€, p = 0.323). So PMR might be cost-efficient and can improve the quality of life, mainly in high-risk patients. 6.4% of the surgeons reported that mesh augmentation takes too long to perform [12]. Only 3 studies reported a slightly increased operation time of 10–20 min [9, 13, 25]. Despite the closing time is coffee time dogma, this might certainly not be an excuse for increased IH rates.
Fear for long-term sequellae of mesh implantation seems not valid either. Glauser et al. reported their experience using an intraperitoneal onlay mesh after more than 5 years of follow-up. Between the second and fifth year, there were no reported complications associated with the mesh [41].
Results of previous systematic reviews are similar. Jairam et al. [42] published their meta-analysis and trial sequential analysis including all studies until 1 January 2017. A significant reduction in incisional hernia rate was observed, specifically in high-risk patients. PMR was found to be safe, with no increase in SSI. Others also found a significant decrease in the incidence of IH [43,44,45,46,47], in some associated with a positive effect on QoL [43]. Sugrue et al. [48] summarized the available evidence in more than 2700 patients showing that besides an optimal laparotomy closure technique, preventive mesh placement should be considered in higher risk patients and if not, surgeons need to question why. Our review also has several limitations. No separate bias analyses were performed on the studies. In the included studies, there are differences in follow-up method and duration. A significant heterogeneity was found in the RCTs. The quality of the studies also varies, but low quality studies were excluded.
PMR can efficiently and safely prevent IH, especially in high-risk patients with a BMI over 29 kg/m2 and with connective tissue disorders. This will increase QoL and is likely to be cost-efficient. Only an increase in seroma rate can be expected, while chronic pain seems slightly increased after mesh reinforcement. SSI and other complications are not increased using PMR. For now, a polypropylene, lightweight, large-pore mesh, in the onlay position is the best recommendation. It’s important that both surgical techniques, new indications and long-term effects are further analyzed. The evidence for the use of PMR is overwhelming, but implementation in daily clinical practice remains limited. Instead of putting their patients at risk for incisional hernia formation and subsequent complications, surgeons should question their arguments why not to use PMR, specifically in high-risk patients.
References
Millikan KW (2003) Incisional hernia repair. Surg Clin North Am 83:1223–1234
van’t Riet M, Steyerberg EW, Nellensteyn J, Bonjer HJ, Jeekel J (2002) Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg 89:1350–1356
Bhangu A, Fitzgerald JE, Singh P, Battersby N, Marriott P, Pinkney T (2013) Systematic review and meta-analysis of prophylactic mesh placement for prevention of incisional hernia following midline laparotomy. Hernia 17:445–455
Flum DR, Horvath K, Koepsell T (2003) Have outcomes of incisional hernia repair improved with time? A population-based analysis. Ann Surg 237:129–135
Alli VV, Zhang J, Telem DA (2018) Impact of incisional hernia development following abdominal operations on total healthcare cost. Surg Endosc 32:2381–2386
Nieuwenhuizen J, Eker HH, Timmermans L, Hop WC, Kleinrensink GJ, Jeekel J et al (2013) A double blind randomized controlled trial comparing primary suture closure with mesh augmented closure to reduce incisional hernia incidence. BMC Surg 13:48
Jairam AP, Timmermans L, Eker HH, Pierik R, van Klaveren D, Steyerberg EW et al (2017) Prevention of incisional hernia with prophylactic onlay and sublay mesh reinforcement versus primary suture only in midline laparotomies (PRIMA): 2-year follow-up of a multicentre, double-blind, randomised controlled trial. Lancet 390:567–576
Timmermans L, de Goede B, Eker HH, van Kempen BJ, Jeekel J, Lange JF (2013) Meta-analysis of primary mesh augmentation as prophylactic measure to prevent incisional hernia. Dig Surg 30:401–409
Bali C, Papakostas J, Georgiou G, Kouvelos G, Avgos S, Arnaoutoglou E et al (2015) A comparative study of sutured versus bovine pericardium mesh abdominal closure after open abdominal aortic aneurysm repair. Hernia 19:267–271
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583 (discussion 583-575)
Caglia P, Tracia A, Borzi L, Amodeo L, Tracia L, Veroux M et al (2014) Incisional hernia in the elderly: risk factors and clinical considerations. Int J Surg 12(Suppl 2):S164–S169
Fischer JP, Harris HW, Lopez-Cano M, Hope WW (2019) Hernia prevention: practice patterns and surgeons’ attitudes about abdominal wall closure and the use of prophylactic mesh. Hernia: J Hernias Abdom Wall Surg 23:329–334
Sarr MG, Hutcher NE, Snyder S, Hodde J, Carmody B (2014) A prospective, randomized, multicenter trial of surgisis gold, a biologic prosthetic, as a sublay reinforcement of the fascial closure after open bariatric surgery. Surgery 156:902–908
Holihan JL, Nguyen DH, Nguyen MT, Mo J, Kao LS, Liang MK (2016) Mesh location in open ventral hernia repair: a systematic review and network meta-analysis. World J Surg 40:89–99. https://doi.org/10.1007/s00268-015-3252-9
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Methodology Checklist 2: Controlled Trials. [document on the Internet]. 2015 [updated 2015 Sept 7]. Available from: http://www.sign.ac.uk/methodology/checklists.html
Methodology Checklist 3: Cohort studies. [document on the Internet]. Scottish Intercollegiate Guidelines Network; 2015 [updated 2015 Sept 7]. Available from: http://www.sign.ac.uk/methodology/checklists.html
Methodology Checklist 6: Economic Evaluations. [document on the Internet]. 2015 [updated 2015 Sept 7]. Available from: http://www.sign.ac.uk/methodology/checklists.html
Probst P, Zaschke S, Heger P, Harnoss JC, Hüttner FJ, Mihaljevic AL et al (2019) Evidence-based recommendations for blinding in surgical trials. Langenbeck’s Arch Surg 404:273–284
Pans A, Elen P, Dewe W, Desaive C (1998) Long-term results of polyglactin mesh for the prevention of incisional hernias in obese patients. World J Surg 22:479–482. https://doi.org/10.1007/s002689900420 (discussion 482-473)
Muysoms FE, Antoniou SA, Bury K, Campanelli G, Conze J, Cuccurullo D et al (2015) European hernia society guidelines on the closure of abdominal wall incisions. Hernia: J Hernias Abdom Wall Surg 19:1–24
Deerenberg EB, Harlaar JJ, Steyerberg EW, Lont HE, van Doorn HC, Heisterkamp J et al (2015) Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. The Lancet 386:1254–1260
Bevis PM, Windhaber RA, Lear PA, Poskitt KR, Earnshaw JJ, Mitchell DC (2010) Randomized clinical trial of mesh versus sutured wound closure after open abdominal aortic aneurysm surgery. Br J Surg 97:1497–1502
Caro-Tarrago A, Olona C, Millan M, Olona M, Espina B, Jorba R (2019) Long-term results of a prospective randomized trial of midline laparotomy closure with onlay mesh. Hernia: J Hernias Abdom Surg 23:335–340
Muysoms FE, Detry O, Vierendeels T, Huyghe M, Miserez M, Ruppert M et al (2016) Prevention of incisional hernias by prophylactic mesh-augmented reinforcement of midline laparotomies for abdominal aortic aneurysm treatment: a randomized controlled trial. Ann Surg 263:638–645
de Beaux AC (2019) Abdominal wall closure. Br J Surg 106:163–164
Curro G, Centorrino T, Low V, Sarra G, Navarra G (2012) Long-term outcome with the prophylactic use of polypropylene mesh in morbidly obese patients undergoing biliopancreatic diversion. Obes Surg 22:279–282
Brosi P, Glauser PM, Speich B, Kaser SA, Maurer CA (2018) Prophylactic intraperitoneal onlay mesh reinforcement reduces the risk of incisional hernia, two-year results of a randomized clinical trial. World J Surg 42:1687–1694. https://doi.org/10.1007/s00268-017-4363-2
Jairam AP, Timmermans L, Eker HH, Pierik R, van Klaveren D, Steyerberg EW et al (2017) Prevention of incisional hernia with prophylactic onlay and sublay mesh reinforcement versus primary suture only in midline laparotomies (PRIMA): 2-year follow-up of a multicentre, double-blind, randomised controlled trial. Lancet 390(10094):567–576
Kohler A, Lavanchy JL, Lenoir U, Kurmann A, Candinas D, Beldi G (2018) Effectiveness of prophylactic intraperitoneal mesh implantation for prevention of incisional hernia in patients undergoing open abdominal surgery: a randomized clinical trial. JAMA Surg 154(2):109
Argudo N, Pera M, Lopez-Cano M, Hernandez L, Sancho JJ, Grande L et al (2018) Selective mesh augmentation to prevent incisional hernias in open colorectal surgery is safe and cost-effective. Front Surg 5:8
Muysoms FE, Antoniou SA, Bury K, Campanelli G, Conze J, Cuccurullo D et al (2015) European hernia society guidelines on the closure of abdominal wall incisions. Hernia 19:1–24
Lanni MA, Tecce MG, Shubinets V, Mirzabeigi MN, Fischer JP (2018) The state of prophylactic mesh augmentation. Am Surg 84:99–108
Garcia-Urena MA, Lopez-Monclus J, Hernando LA, Montes DM, Valle de Lersundi AR, Pavon CC et al (2015) Randomized controlled trial of the use of a large-pore polypropylene mesh to prevent incisional hernia in colorectal surgery. Ann Surg 261:876–881
Gutierrez de la Pena C, Medina Achirica C, Dominguez-Adame E, Medina Diez J (2003) Primary closure of laparotomies with high risk of incisional hernia using prosthetic material: analysis of usefulness. Hernia: J Hernias Abdom Wall Surg 7:134–136
El-Khadrawy OH, Moussa G, Mansour O, Hashish MS (2009) Prophylactic prosthetic reinforcement of midline abdominal incisions in high-risk patients. Hernia 13:267–274
Weltz AS, Sibia US, Zahiri HR, Schoeneborn A, Park A, Belyansky I (2017) Operative outcomes after open abdominal wall reconstruction with retromuscular mesh fixation using fibrin glue versus transfascial sutures. Am Surg 83:937–942
Rhemtulla IA, Tecce MG, Broach RB, Messa CAt, Mauch JT, Fischer JP (2019) Retromuscular mesh repair using fibrin glue: early outcomes and cost-effectiveness of an evolving technique. Plast Reconstr Surg Glob Open 7:e2184
Fischer JP, Basta MN, Wink JD, Krishnan NM, Kovach SJ (2015) Cost-utility analysis of the use of prophylactic mesh augmentation compared with primary fascial suture repair in patients at high risk for incisional hernia. Surgery 158:700–711
Organisation WH. Table: Threshold values for intervention cost-effectiveness by Region2005 24/10/2016 24/10/2016]
Glauser PM, Brosi P, Speich B, Kaser SA, Heigl A, Rosenberg R et al (2019) Prophylactic intraperitoneal onlay mesh following midline laparotomy-long-term results of a randomized controlled trial. World J Surg 43:1669–1675. https://doi.org/10.1007/s00268-019-04964-6
Jairam AP, López-Cano M, García Alamino J, Pereira JA, Timmermans L, Jeekel J et al (2020) Prevention of incisional hernia after midline laparotomy with prophylactic mesh reinforcement: a meta-analysis and trial sequential analysis. BJS Open 4(3):357–368
Wang XC, Zhang D, Yang ZX, Gan JX, Yin LN (2017) Mesh reinforcement for the prevention of incisional hernia formation: a systematic review and meta-analysis of randomized controlled trials. J Surg Res 209:17–29
Muysoms FE, Dietz UA (2017) Prophylactic meshes in the abdominal wall. Chirurg 88:34–41
Borab ZM, Shakir S, Lanni MA, Tecce MG, MacDonald J, Hope WW et al (2017) Does prophylactic mesh placement in elective, midline laparotomy reduce the incidence of incisional hernia? A systematic review and meta-analysis. Surgery 161:1149–1163
Payne R, Aldwinckle J, Ward S (2017) Meta-analysis of randomised trials comparing the use of prophylactic mesh to standard midline closure in the reduction of incisional herniae. Hernia 21:843–853
Harris HW, Hope WH, Adrales G, Andersen DK, Deerenberg EB, Diener H et al (2018) Contemporary concepts in hernia prevention: Selected proceedings from the 2017 International Symposium on Prevention of Incisional Hernias. Surgery 164:319-326
Sugrue M, Johnston A, Zeeshan S, Loughlin P, Bucholc M, Watson A (2019) The role of prophylactic mesh placement to prevent incisional hernia in laparotomy. Is it time to change practice? Anaesthesiol Intens Ther 51:323–329
Abo-Ryia MH, El-Khadrawy OH, Abd-Allah HS (2013) Prophylactic preperitoneal mesh placement in open bariatric surgery: a guard against incisional hernia development. Obes Surg 23:1571–1574
Caro-Tarrago A, Olona Casas C, Jimenez Salido A, Duque Guilera E, Moreno Fernandez F, Vicente Guillen V (2014) Prevention of incisional hernia in midline laparotomy with an onlay mesh: a randomized clinical trial. World J Surg 38:2223–2230. https://doi.org/10.1007/s00268-014-2510-6
El-Khadrawy OH, Moussa G, Mansour O, Hashish MS (2009) Prophylactic prosthetic reinforcement of midline abdominal incisions in high-risk patients. Hernia: J Hernias Abdom Wall Surg 13:267–274
Pizza F, D’Antonio D, Arcopinto M, Dell’Isola C, Marvaso A (2020) Safety and efficacy of prophylactic resorbable biosynthetic mesh following midline laparotomy in clean/contemned field: preliminary results of a randomized double blind prospective trial. Hernia 24:85–92
Strzelczyk JM, Szymanski D, Nowicki ME, Wilczynski W, Gaszynski T, Czupryniak L (2006) Randomized clinical trial of postoperative hernia prophylaxis in open bariatric surgery. Br J Surg 93:1347–1350
Argudo N, Pereira JA, Sancho JJ, Membrilla E, Pons MJ, Grande L (2014) Prophylactic synthetic mesh can be safely used to close emergency laparotomies, even in peritonitis. Surgery 156:1238–1244
Kurmann A, Barnetta C, Candinas D, Beldi G (2013) Implantation of prophylactic nonabsorbable intraperitoneal mesh in patients with peritonitis is safe and feasible. World J Surg 37:1656–1660. https://doi.org/10.1007/s00268-013-2019-4
Llaguna OH, Avgerinos DV, Nagda P, Elfant D, Leitman IM, Goodman E (2011) Does prophylactic biologic mesh placement protect against the development of incisional hernia in high-risk patients? World J Surg 35:1651–1655. https://doi.org/10.1007/s00268-011-1131-6
Von Ahrens D, Hwang R, Kato T, Emend J, Gnesemer A, Samstein B (2019) Absorbable mesh placement to prevent incisional hernias after donor hepatectomy. Am J Transplant 19:876
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MD: conception and design, and/or acquisition of data, and/or analysis and interpretation of data, draft, revising; MA: analysis and interpretation of data, draft, revising, Luis Abreu de carvalho, analysis and interpretation of data, draft, revising; AV: analysis and interpretation of data, draft, revising; FB: conception and design, and/or acquisition of data, and/or analysis and interpretation of data, draft, revising.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Depuydt, M., Allaeys, M., de Carvalho, L.A. et al. Prophylactic Mesh After Midline Laparotomy: Evidence is out There, but why do Surgeons Hesitate?. World J Surg 45, 1349–1361 (2021). https://doi.org/10.1007/s00268-020-05898-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05898-0