Abstract
Aim
Adrenocortical cancer (ACC) is a rare disease with a poor outcome, and robust prognostic factors remain unclear. High neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) as markers of host inflammation have been found to be associated with decreased long-term outcomes in several tumour types, but have been scarcely analysed in ACC.
Methods
Patients who underwent resection of their ACC between 2000 and 2020 were identified; therapeutic, operative and outcome data were analysed. Pre-operative NLR and PLR were calculated by division of neutrophils and platelets by lymphocytes measured in peripheral blood.
Results
Fifty-seven patients (30F:27 M) with an overall median age of 53 years [range: 18–86] presented with tumours of median size 11.5 cm [range: 3.0–22.0], of whom 26 (46%) were hormonally active. Majority of patients underwent an open resection (n = 48; 84%); more than half (n = 30; 53%) underwent multi-organ excision. Median NLR was 4.63 and median PLR was 186.21; these values were used for median split analyses (low vs. high). There were no differences with regard to age, sex or tumour characteristics and peri-operative data between the two groups (all p > 0.05). Overall, median recurrence-free survival (RFS) was 26 months (3-year: 45%) on Kaplan–Meier analysis. On univariate analyses, a high NLR did not influence RFS [HR = 1.57 (95%-CI: 0.73–2.38); p = 0.25], but patients with a high PLR had an increased risk of developing recurrence [HR = 2.39 (95%-CI: 1.08–5.31); p = 0.03]. The median overall survival (OS) was 33 months (3 years: 79%) on Kaplan–Meier analysis. Both a high NLR [HR = 2.24 (95%-CI: 1.07–4.70); p = 0.03] and a high PLR [HR = 4.02 (95%-CI: 1.80–8.98); p = 0.001] were strongly associated with a shorter OS on unadjusted analyses.
Conclusion
Elevated pre-operative NLR and PLR are associated with shorter OS, while higher PLR was also associated with a shorter RFS for patients undergoing curative intent resection of ACC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adrenocortical cancer (ACC) is a rare tumour with an incidence of 1–2/million population/year. [1] Complete surgical resection is the backbone of treatment for localised disease, with reported 5-year survival rates after curative intent resection ranging from 40 to 51%. [2,3,4] Factors currently commonly used for survival estimates are clinical parameters, such as hormonal functionality of the tumour [5, 6] and age of the patient [7], or pathological variables, such as stage of the tumour [8], proliferation index of the tumour (e.g. the Weiss score) [9] and Ki67 immunostaining. [10] However, the cohort of patients with ACC as a whole is very heterogeneous and long-term outcomes may therefore differ even among patients within the same tumour stage, due to the largely still unknown impact of different clinical, pathological and molecular factors [11].
Traditional risk factors are currently unable to stratify patients satisfactorily to a certain prognostic group; thus, molecular and genetic biomarkers have been proposed as potential new predictive markers. [12,13,14] However, these have not yet been proved to be feasible in routine clinical practice as many of these techniques remain restricted to research laboratories.
In recent years, neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) have been reported to predict oncologic outcomes for various other types of carcinomas such as gastric, colorectal, lung, pancreas, ovarian, hepatocellular and oesophageal. [15,16,17,18,19,20] Conversely to molecular testing, these assays are inexpensive and readily available for all patients to be used as inflammatory- and immunologic-based investigations.
Inflammation is a known major driver for the development and progression among various types of cancer. The immune cells most commonly associated with progression of disease include neutrophils and platelets. [21] The hypothesis is that a higher NLR and PLR are associated with a worse oncological outcome. There are presently limited data on this association between NLR and PLR and oncological outcomes for patients who underwent surgery for ACC. [22, 23] The aim of the current analysis was to assess the prognostic impact of baseline NLR and PLR for patients who underwent resection of their ACC.
Methods
All patients (n = 57) who underwent a resection of their ACC between 2000 and 2020 at Oxford University Hospital Trust (Oxford, UK) and for whom a complete blood cell count with differential count within a week prior to the operation was available were included. All data were prospectively collected in a database and retrospectively analysed as part of an ongoing audit on outcomes after surgery for endocrine tumours.
Management decisions
At time of diagnosis, all patients were formally discussed in our weekly multidisciplinary meeting. This meeting was attended by endocrine surgeons, oncologists, radiologist, pathologists, nuclear physicians and endocrinologists. All patients underwent a full endocrine assessment, and all patients also had preoperative imaging studies done, in the form of a thoraco-abdominal Computed Tomography (CT) scan, while more recent patients also underwent a preoperative 18F-FDG positron emission tomography (PET) scan. All tumour staging was decided in concordance with the international guidelines published by the European Network for Study of Adrenal Tumours (ENSAT) [8].
Open radical adrenalectomy with en bloc resection of the tumour and ipsilateral kidney was the standard surgical approach in patients who had a preoperative diagnosis of ACC, with further decisions about multi-organ resection made on a case-by-case basis. Laparoscopic surgery was performed only when the presenting diagnosis of incidentaloma was made in patients with a tumour of < 6 cm and the diagnosis of ACC was proved only postoperatively.
To make decisions on postoperative oncological treatment and follow-up, all patients were again discussed in our multidisciplinary meeting. While adjuvant therapy with mitotane was considered for all patients with ENSAT-stage 1 or 2, patients with a tumour staged as ENSAT 3 or 4 were offered to start mitotane treatment within 4–8 weeks after their operation. These patients had their plasma levels regularly monitored (target level 14–20 mg/dL). Our follow-up protocol consisted of cross-sectional imaging by CT scan (with or without a 18F-FDG-PET scan), according to clinical protocols. Recurrence of disease was defined as either radiological evidence of local or distant disease on cross-sectional imaging or on functional studies.
Data collected
Standard demographic (age, sex), clinical (site and functionality of the tumour), biochemical (neutrophil count in 109/L, lymphocyte count in 109/L and platelet count in 109/L within a week prior to surgery) and operative data (type and extent of surgery) were collected. Moreover, histological variables (size of the tumour, ki-67 index, [10] resection margin and TNM status [24]) were noted. Short-term outcomes (length of stay and development of post-operative morbidity [classified according to minor (Dindo–Clavien grade < 3) vs. major (Dindo–Clavien grade ≥ 3) [25] as well as oncological outcomes (recurrence of disease and overall survival) were recorded].
Statistical analyses
Summary statistics were obtained and presented as percentages or median values. Upon comparing categorical data, the Chi-square test, or if deemed appropriate Fisher's exact test, was used, while the Mann–Whitney U-test was used to compare continuous data.
NLR was calculated by division of the absolute neutrophil and lymphocyte counts measured in peripheral blood before surgery. PLR was calculated by division of thrombocytes and lymphocytes accordingly. For descriptive statistics, patients were subdivided into two groups after performance of a median split, the low group below the median and the high group above.
Factors associated with overall and recurrence free survival were examined using cross-tabs and the nonparametric product limit method. Cox proportional hazards models were developed using relevant clinicopathologic variables to determine the association of each with survival. Relative risks were expressed as hazard ratios (HRs) with 95% CIs. Overall, a p-value of less than 0.05 was considered significant. All statistical analyses were performed using IBM SPSS Statistics for Macintosh, Version 23.0 (IBM Corp. IMB SPSS statistics, Armonk, NY).
Results
Patient characteristics
The demographic, clinical and peri-operative data of the 57 patients who were included in the current analysis are detailed in Table 1. The median age at time of diagnosis was 53 years [range: 18–86]. In almost half of patients, the tumour was hormonally active (n = 26; 46%), with 15 patients (58%) having a cortisol-producing tumour.
Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR)
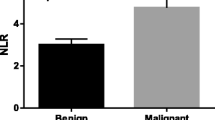
The median NLR for the whole cohort was 4.63, and the median PLR was 186.21. Table 2 details the demographic, clinical and operative characteristics of all patients stratified by patients NLR and PLR, grouped according to medial split. There are no differences with regard to age, sex or tumour characteristics and peri-operative data between the two groups (all p > 0.05).
Details of surgery and histopathology
The majority of patients underwent an open resection of their ACC (n = 48; 84%). More details on the surgical procedure are summarised in Table 1.
Unfortunately, the N-stage of most patients was unknown [i.e. Nx; n = 37 (65%)], while 12 patients had no signs of lymph node metastases [i.e. N0; n = 12 (21%)], and in eight patients, metastases in lymph nodes were confirmed [n = 8 (14%)].
Short-term outcomes
The median length of stay was 7 days [range: 1–67]. Two patients (4%) died during their hospital admission after treatment for severe malignant Cushing syndrome. One patient died on post-operative day 36 after undergoing an open bilateral adrenalectomy and splenectomy with lymph node dissection. This patient developed intra-abdominal collections and subsequent sepsis and succumbed to multi-organ failure. Another patient died 45 days after undergoing an open left-sided adrenalectomy plus nephrectomy plus splenectomy and extraction of the tumour from the inferior vena cava through bypass surgery. They suffered a neurological deficit attributed to prolonged bypass use and died of airway complications after tracheostomy. Further details on post-operative morbidity are detailed in Table 1.
When looking at the NLR, there was no association found between a high ratio and the development of post-operative morbidity (p = 0.29), while among those with a high PLR the incidence of complications bordered on being significantly higher (p = 0.05). There was no increased morbidity when looking at sex or age, the hormonal status of the tumour or the location of the tumour (all p > 0.05).
Long-term outcomes and predictors of survival
At time of last follow-up, 28 (49%) patients had developed recurrent disease after a median recurrence-free survival (RFS) of 26 months, with a 1-year RFS of 70% and a 3-year RFS of 45%. While six patients (21%) developed only local recurrence of their disease, 19 patients (68%) developed recurrent disease at one or more distant locations (e.g. lung or liver) and two patients (7%) developed both local and distant recurrence of disease. A total of 12 patients (43%) underwent repeat resection of their recurrent ACC.
Upon exploring factors associated with an increased risk of recurrence of disease (Table 3), a high NLR did not seem to influence the risk of recurrent disease (HR = 1.57 [95%-CI: 0.73–2.38]; p = 0.25; Fig. 1a). Conversely, patients with a high PLR before surgery had an increased risk of developing recurrence of their disease, with patients with a higher than median PLR being at a more than two-fold increased risk [HR = 2.39 (95%-CI: 1.08–5.31); p = 0.03; Fig. 1b]. Other factors found to be associated with an increased risk of developing recurrent disease on univariate analyses were T-stage of 3 or 4 [HR = 2.72 (95%-CI: 1.23–5.99); p = 0.01] and the presence of capsular invasion on histological examination [HR = 2.39 (95%-CI: 1.09–5.22); p = 0.03]. Due to the small number of included patients, controlling for competing factors by performance of a multivariate analysis was not deemed feasible. Examining the subgroup of patients without metastatic disease, there was no difference in RFS when stratifying patients by NLR (p = 0.28) or PLR (p = 0.06).
The median overall survival (OS) for all patients was 33 months, with a 1-year OS of 79% and a 3-year OS of 49%. Table 3 displays the factors associated with OS for the whole cohort of patients. Specifically, patients within the high NLR group had a more than twofold increased risk of an early death [HR = 2.24 (95%-CI: 1.07–4.70); p = 0.03; Fig. 2a]. Moreover, when looking at the potency of the PLR as a prognostic factor, for patients with a higher than median PLR, the risk of an early death was more than four times higher [HR = 4.02 (95%-CI: 1.80–8.98); p = 0.001; Fig. 2b]. Other factors deemed to be associated with a shortened overall survival on univariate analyses were age at time of diagnosis [HR = 1.03 (95%-CI: 1.01–1.05); p = 0.006], the presence of local invasion or invasion into adjacent organs (i.e. T-stage of 3 or 4) [HR = 3.35 (95%-CI: 1.50–7.51); p = 0.003] or of positive lymph nodes (i.e. N1-status) [HR = 4.10 (95%-CI: 1.05–15.95); p = 0.04], signs of capsular invasion on histological examination [HR = 2.46 (95%-CI: 1.18–5.12); p = 0.02] or a positive resection margin (i.e. R1 or R2) [HR = 2.47 (95%-CI: 1.20–5.09); p = 0.02]. Multivariate analysis to exclude confounding was not deemed possible due to the limited sample size. For patients who did not have metastatic disease present at the time of surgery, their OS was shorter for patients with higher NLR (1-year OS of 74% and a 3-year OS of 33%) compared with low NLR (1-year OS of 90% and a 3-year OS of 74%; p = 0.024). Similarly, the OS was found to be shorter for those patients with a high PLR (1-year OS of 67% and 3-year OS of 25%) compared with low PLR (1-year OS of 96% and a 3-year OS of 72%; p < 0.001).
Discussion
Adrenocortical carcinoma (ACC) is one of the most aggressive endocrine tumours. Due to its low incidence and possibly to the concurrent lack of centralised treatment for this patient group, robust risk factors to predict a worse long-term outcome have not yet been identified. [26] While the incidence of ACC seems to be rising [27, 28] and traditionally used variables have proved to be unable to stratify patients towards reliable survival groups, there is a need for more reliable prognostic markers. With molecular testing currently not readily available to be used in clinical settings, we explored the prognostic role of pre-operative NLR and PLR as potential cheap and widely available markers. Only two studies have addressed this question before in ACC. The first reported on 84 patients who underwent surgery for ACC at several institutions; 5-year RFS was lower when NLR and PLR were elevated and NLR was associated with decreased diseases-specific survival (HR 2.21) as well as and RFS (HR 1.99). [22] Others confirmed that the higher NLR group (NLR > 5) showed a significantly poorer overall survival than the lower NLR group. [23] We aimed to validate the findings from these previous two reports in a relatively large, single-centre cohort of patients undergoing curative intent surgery for ACC in order to increase the overall interest in the significance of using NLR and PLR as prognostic markers for this group of patients and to perhaps promote future prospective studies into its clinical implementation.
We report on a fairly typical cohort of patients undergoing curative intent surgery for their ACC, [26] including 57 patients with a median age of 53 years and a male-to-female ratio of almost 1:1.
About half of patients developed post-operative morbidity, while two patients died during their admission (4%). Peri-operative complications following surgery for ACC are relatively common, probably largely due to the extent of the surgery undertaken. [29, 30] While in our cohort, a higher NLR or PLR were not significantly increasing the incidence of morbidity, other groups have reported on this association in other types of diseases and noted that higher ratios of either of both increased the risk of developing systemic inflammatory response syndrome (SIRS) or sepsis. [31, 32] Although we could not demonstrate this in the current study, this might be an important finding, as Margonis et al. [30] reported that occurrence of postoperative complications after resection of ACC is an independent risk factor for a decreased long-term outcome. Therefore, the prevention of post-operative complications might be an important factor from an oncologic perspective and being able to stratify patients into a high-risk group before their surgery could therefore be beneficial in the longer term.
Overall median RFS was 26 months, with a 1-year RFS of 70% and a 3-year RFS of 45%, and a total of 12 patients (43%) underwent repeat resection of their recurrent disease. These statistics are similar to those reported by other groups who also described the feasibility of repeat surgery in select patients. [33,34,35] The median OS for all patients was 33 months, with a 1-year OS of 79% and a 3-year OS of 49% as corroborated by survival analyses in other cohorts. [8, 36,37,38] While a higher NLR did not seem to significantly influence the risk of recurrent disease, patients with a high PLR before surgery had a more than two-fold increased risk of developing recurrence of their disease. For OS, this association seemed to be even more profound, as the risk of an early death was increased more than twofold for patients within the high NLR and more than four times higher for those in the high PLR group. Similarly, an increasing number of studies in the literature have revealed that NLR and PLR indeed act as significant prognostic factors for both disease recurrence and overall survival in a variety of cancer types [15,16,17,18,19,20, 39, 40].
Although the exact molecular pathways through which the NLR and PLR are associated with poorer outcomes remain unelucidated, several hypotheses have been, mainly based on imbalances in the immune response to the tumour cells. [39, 40] Circulating cytokines and chemokines released by the malignant cells of solid tumours trigger a systemic inflammatory response, resulting in systematic alterations, such as an increase in neutrophils and platelets and a decrease in lymphocytes. [41] The subsequent occurrence of neutrophilia inhibits the cytolytic activity of certain immune cells, such as lymphocytes, activated T-cells and natural killer cells. [42] Moreover, neutrophils have shown to enhance angiogenesis and to promote primary tumour progression. [43] Additionally, platelets not only aid in the growth of primary tumour cells via angiogenesis, but also assist the tumour cells in evading the host immune system by protecting them from tumour lysis mediated by natural killer cells. [44,45,46] On the other hand, for patients with a higher NLR or PLR, their lymphocyte count is relatively low. Lymphocytes play an important role in the cell-mediated anti-tumour immune response. Several studies on different types of cancer state that lymphopenia is a predictive factor for a shorter RFS and OS, [47, 48] with others suggesting an improved outcome for those with an increased lymphocyte infiltration in tumours [49].
Conversely, some authors recently suggested that its impact on oncological outcomes is merely due to the relationship between the NLR or PLR and adverse certain tumour characteristics. [50, 51] While we could not fully exclude confounding by other variables as we were limited by our sample size to perform any adjusted analyses, we did not find any differences in patient and tumour variables between the low and high NLR or PLR groups, indicating NLR and PLR to act as surrogates for other characteristics.
The proliferation marker ki-67 index has been shown to be an independent prognostic factor for survival among patients undergoing resection for ACC. [10] This finding could be reproduced in our current analysis. The ki-67 index was, however, not consistently reported for patients included and was therefore only available in 24 patients (42%). Moreover, only the subgroups of an index of < 10% and ≥ 10% could thus be formed. This limited availability of the ki-67 results is most probably due to the ongoing reluctance of several pathologists to provide an exact value for this variable. This is presumably based on the known variability among the current practices for ki-67 scoring assessments, as interobserver variations set particular limitations around clinically relevant cut-off values. [52] The statistical power of our analysis involving this parameter could therefore be interpreted as non-robust and hence thus unable to demonstrate a significant correlation of the ki-67 index with survival in our cohort.
The present study has several limitations associated with its retrospective nature such as that we had to rely on the accuracy and completeness of the recordkeeping. Moreover, although our study has one of the largest numbers of patients from a single institution, the included number of patients is still relatively low due to the rarity of the disease. While this, on one hand, only stresses the highly selected nature of the cohort of patients with ACC who are considered for resection, the small sample size has statistical disadvantages. Specifically, we were unable to properly control for competing factor and exclude confounding, as multivariate analyses were not deemed appropriate due to the relatively small number of patients in each group or unavailability of necessary data.
While both NLR and PLR are variables available at the beginning of the decision-making process, they could potentially be used to stratify patients into certain risk groups and influence treatment and follow-up protocols. However, this potential feasibility of incorporating NLR and PLR in the decision-making process has not been assessed in the current study, but this could be the scope of a further prospective study. It is, nonetheless, likely that other parameters which are currently not widely available or in use yet (e.g. molecular testing and gene profiling) could prove to be much stronger predictors of long-term outcomes for patients undergoing curative intent surgical resection of their ACC and that these parameters should therefore be used to guide decision-making on the intensity of treatment and/or follow-up.
In summary, for patients undergoing curative intent surgical resection of their ACC both a higher pre-operative NLR and PLR strongly correlated with a diminished overall survival, while a higher PLR also predicted the recurrence of disease. This proposes NLR and PLR as prognostic markers which are inexpensive and readily available and could easily add additional prognostic information for patients undergoing surgery for ACC. This hypothesis should be validated in a multicentre study.
References
Fassnacht M, Allolio B (2009) Clinical management of adrenocortical carcinoma. Best Pract Res Clin Endocrinol Metab 23(2):273–289
Fassnacht M, Libe R, Kroiss M, Allolio B (2011) Adrenocortical carcinoma: a clinician’s update. Nat Rev Endocrinol 7(6):323–335
Ayala-Ramirez M, Jasim S, Feng L, Ejaz S, Deniz F, Busaidy N et al (2013) Adrenocortical carcinoma: clinical outcomes and prognosis of 330 patients at a tertiary care center. Eur J Endocrinol 169(6):891–899
Puglisi S, Calabrese A, Basile V, Pia A, Reimondo G, Perotti P et al (2020) New perspectives for mitotane treatment of adrenocortical carcinoma. Best Pract Res Clin Endocrinol Metab 34(3):101415
Abiven G, Coste J, Groussin L, Anract P, Tissier F, Legmann P et al (2006) Clinical and biological features in the prognosis of adrenocortical cancer: poor outcome of cortisol-secreting tumors in a series of 202 consecutive patients. J Clin Endocrinol Metab 91(7):2650–2655
Berruti A, Fassnacht M, Haak H, Else T, Baudin E, Sperone P et al (2014) Prognostic role of overt hypercortisolism in completely operated patients with adrenocortical cancer. Eur Urol 65(4):832–838
Libe R, Borget I, Ronchi CL, Zaggia B, Kroiss M, Kerkhofs T et al (2015) Prognostic factors in stage III–IV adrenocortical carcinomas (ACC): an European Network for the Study of Adrenal Tumor (ENSAT) study. Ann Oncol 26(10):2119–2125
Fassnacht M, Johanssen S, Quinkler M, Bucsky P, Willenberg HS, Beuschlein F et al (2009) Limited prognostic value of the 2004 international union against cancer staging classification for adrenocortical carcinoma: proposal for a revised TNM classification. Cancer 115(2):243–250
Weiss LM, Medeiros LJ, Vickery AL Jr (1989) Pathologic features of prognostic significance in adrenocortical carcinoma. Am J Surg Pathol 13(3):202–206
Beuschlein F, Weigel J, Saeger W, Kroiss M, Wild V, Daffara F et al (2015) Major prognostic role of Ki67 in localized adrenocortical carcinoma after complete resection. J Clin Endocrinol Metab 100(3):841–849
Terzolo M, Daffara F, Ardito A, Zaggia B, Basile V, Ferrari L et al (2014) Management of adrenal cancer: a 2013 update. J Endocrinol Invest 37(3):207–217
Li X, Gao Y, Xu Z, Zhang Z, Zheng Y, Qi F (2020) Identification of prognostic genes in adrenocortical carcinoma microenvironment based on bioinformatic methods. Cancer Med 9(3):1161–1172
Assie G, Jouinot A, Fassnacht M, Libe R, Garinet S, Jacob L et al (2019) Value of molecular classification for prognostic assessment of adrenocortical carcinoma. JAMA Oncol 5(10):1440–1447
Crona J, Beuschlein F (2019) Adrenocortical carcinoma—towards genomics guided clinical care. Nat Rev Endocrinol 15(9):548–560
Feng JF, Huang Y, Chen QX (2014) Preoperative platelet lymphocyte ratio (PLR) is superior to neutrophil lymphocyte ratio (NLR) as a predictive factor in patients with esophageal squamous cell carcinoma. World J Surg Oncol 12:58
Templeton AJ, Ace O, McNamara MG, Al-Mubarak M, Vera-Badillo FE, Hermanns T et al (2014) Prognostic role of platelet to lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev 23(7):1204–1212
Chen H, He J (2014) Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after radical resection of esophageal squamous cell carcinoma. Zhonghua Zhong Liu Za Zhi 36(4):294–297
Smith RA, Ghaneh P, Sutton R, Raraty M, Campbell F, Neoptolemos JP (2008) Prognosis of resected ampullary adenocarcinoma by preoperative serum CA19-9 levels and platelet-lymphocyte ratio. J Gastrointest Surg 12(8):1422–1428
Stotz M, Gerger A, Eisner F, Szkandera J, Loibner H, Ress AL et al (2013) Increased neutrophil-lymphocyte ratio is a poor prognostic factor in patients with primary operable and inoperable pancreatic cancer. Br J Cancer 109(2):416–421
Yodying H, Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Yamada M et al (2016) Prognostic significance of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in oncologic outcomes of esophageal cancer: a systematic review and meta-analysis. Ann Surg Oncol 23(2):646–654
Diakos CI, Charles KA, McMillan DC, Clarke SJ (2014) Cancer-related inflammation and treatment effectiveness. Lancet Oncol 15(11):e493-503
Bagante F, Tran TB, Postlewait LM, Maithel SK, Wang TS, Evans DB et al (2015) Neutrophil-lymphocyte and platelet-lymphocyte ratio as predictors of disease specific survival after resection of adrenocortical carcinoma. J Surg Oncol 112(2):164–172
Mochizuki T, Kawahara T, Takamoto D, Makiyama K, Hattori Y, Teranishi JI et al (2017) The neutrophil-to-lymphocyte ratio (NLR) predicts adrenocortical carcinoma and is correlated with the prognosis. BMC Urol 17(1):49
AJCC cancer staging manual, eighth edition staging. Available from: https://cancerstaging.org/references-tools/deskreferences/Documents/AJCC%20Cancer%20Staging%20Form%20Supplement.pdf
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Mihai R (2015) Diagnosis, treatment and outcome of adrenocortical cancer. Br J Surg 102(4):291–306
Gaujoux S, Weinandt M, Bonnet S, Reslinger V, Bertherat J, Dousset B (2017) Surgical treatment of adrenal carcinoma. J Visc Surg 154(5):335–343
Dickson PV, Kim L, Yen TWF, Yang A, Grubbs EG, Patel D et al (2018) Evaluation, staging, and surgical management for adrenocortical carcinoma: an update from the SSO endocrine and head and neck disease site working group. Ann Surg Oncol 25(12):3460–3468
Eichhorn-Wharry LI, Talpos GB, Rubinfeld I (2012) Laparoscopic versus open adrenalectomy: another look at outcome using the Clavien classification system. Surgery 152(6):1090–1095
Margonis GA, Amini N, Kim Y, Tran TB, Postlewait LM, Maithel SK et al (2016) Incidence of perioperative complications following resection of adrenocortical carcinoma and its association with long-term survival. World J Surg 40(3):706–714. https://doi.org/10.1007/s00268-015-3307-y
Cetinkaya M, Buldu I, Kurt O, Inan R (2017) Platelet-to-lymphocyte Ratio: a new factor for predicting systemic inflammatory response syndrome after percutaneous nephrolithotomy. Urol J 14(5):4089–4093
Sen V, Bozkurt IH, Aydogdu O, Yonguc T, Yarimoglu S, Sen P et al (2016) Significance of preoperative neutrophil-lymphocyte count ratio on predicting postoperative sepsis after percutaneous nephrolithotomy. Kaohsiung J Med Sci 32(10):507–513
Glenn JA, Else T, Hughes DT, Cohen MS, Jolly S, Giordano TJ et al (2019) Longitudinal patterns of recurrence in patients with adrenocortical carcinoma. Surgery 165(1):186–195
Simon G, Pattou F, Mirallie E, Lifante JC, Nomine C, Arnault V et al (2017) Surgery for recurrent adrenocortical carcinoma: a multicenter retrospective study. Surgery 161(1):249–256
Dy BM, Wise KB, Richards ML, Young WF Jr, Grant CS, Bible KC et al (2013) Operative intervention for recurrent adrenocortical cancer. Surgery 154(6):1292–1299 (discussion 9)
Saade N, Sadler C, Goldfarb M (2015) Impact of regional lymph node dissection on disease specific survival in adrenal cortical carcinoma. Horm Metab Res 47(11):820–825
Vanbrabant T, Fassnacht M, Assie G, Dekkers OM (2018) Influence of hormonal functional status on survival in adrenocortical carcinoma: systematic review and meta-analysis. Eur J Endocrinol 179(6):429–436
Else T, Kim AC, Sabolch A, Raymond VM, Kandathil A, Caoili EM et al (2014) Adrenocortical carcinoma. Endocr Rev 35(2):282–326
Zheng J, Cai J, Li H, Zeng K, He L, Fu H et al (2017) Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as prognostic predictors for hepatocellular carcinoma patients with various treatments: a meta-analysis and systematic review. Cell Physiol Biochem 44(3):967–981
Jiang K, Lei J, Chen W, Gong Y, Luo H, Li Z et al (2016) Association of the preoperative neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios with lymph node metastasis and recurrence in patients with medullary thyroid carcinoma. Medicine (Baltimore) 95(40):e5079
Salazar-Onfray F, Lopez MN, Mendoza-Naranjo A (2007) Paradoxical effects of cytokines in tumor immune surveillance and tumor immune escape. Cytokine Growth Factor Rev 18(1–2):171–182
Kuang DM, Zhao Q, Wu Y, Peng C, Wang J, Xu Z et al (2011) Peritumoral neutrophils link inflammatory response to disease progression by fostering angiogenesis in hepatocellular carcinoma. J Hepatol 54(5):948–955
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357(9255):539–545
Nieswandt B, Hafner M, Echtenacher B, Mannel DN (1999) Lysis of tumor cells by natural killer cells in mice is impeded by platelets. Cancer Res 59(6):1295–1300
Kim PY (2015) Platelets: connecting clotting and lysis. Blood 125(16):2459
Jain S, Harris J, Ware J (2010) Platelets: linking hemostasis and cancer. Arterioscler Thromb Vasc Biol 30(12):2362–2367
Mehrazin R, Uzzo RG, Kutikov A, Ruth K, Tomaszewski JJ, Dulaimi E et al (2015) Lymphopenia is an independent predictor of inferior outcome in papillary renal cell carcinoma. Urol Oncol. 33(9):388.e19-388.e25
Onal C, Yildirim BA, Guler OC, Mertsoylu H (2018) The utility of pretreatment and posttreatment lymphopenia in cervical squamous cell carcinoma patients treated with definitive chemoradiotherapy. Int J Gynecol Cancer 28(8):1553–1559
Loi S, Sirtaine N, Piette F, Salgado R, Viale G, Van Eenoo F et al (2013) Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02–98. J Clin Oncol 31(7):860–867
Wang D, Wu M, Feng FZ, Huang HF, Yang JX, Shen K et al (2013) Pretreatment neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios do not predict survival in patients with cervical cancer treated with neoadjuvant chemotherapy and radical hysterectomy. Chin Med J (Engl) 126(8):1464–1468
Kwon HC, Kim SH, Oh SY, Lee S, Lee JH, Choi HJ et al (2012) Clinical significance of preoperative neutrophil-lymphocyte versus platelet-lymphocyte ratio in patients with operable colorectal cancer. Biomarkers 17(3):216–222
Papathomas TG, Pucci E, Giordano TJ, Lu H, Duregon E, Volante M et al (2016) An international Ki67 reproducibility study in adrenal cortical carcinoma. Am J Surg Pathol 40(4):569–576
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Jong, M.C., Mihai, R. & Khan, S. Neutrophil-to-Lymphocyte Ratio (NLR) and Platelet-to-Lymphocyte Ratio (PLR) as Possible Prognostic Markers for Patients Undergoing Resection of Adrenocortical Carcinoma. World J Surg 45, 754–764 (2021). https://doi.org/10.1007/s00268-020-05868-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05868-6