Abstract
Introduction
Gastroesophageal reflux disease (GERD) may present with heartburn, regurgitation, dysphagia, chronic cough, laryngitis, or even asthma. The clinical presentation of GERD is therefore varied and poses certain challenges to the physician, especially given the limitations of the diagnostic testing.
Discussion
The evaluation of patients with suspected GERD might be challenging. It is based on the evaluation of clinical features, objective evidence of reflux on diagnostic testing, correlation of symptoms with episodes of reflux, evaluation of anatomical abnormalities, and excluding other causes that might account for the presence of the patient’s symptoms.
Conclusions
The diagnostic evaluation should include multiple tests, in addition to a thorough clinical examination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The presentation of patients with suspected gastroesophageal reflux disease (GERD) is complex and might include a cadre of symptoms that include heartburn, regurgitation, dysphagia, chronic cough, laryngitis, or even asthma. The Montréal classification of GERD was created in 2006 to provide a diagnostic standardization of the symptomatology globally [1]. This classification defined GERD as “a condition resulting from reflux of stomach contents and causing troublesome symptoms or complications, occurring at least 2 times per week, with an adverse effect on an individual’s well-being.” The Montréal classification also stated that GERD might present with a typical, or “esophageal,” symptomatology that includes heartburn, regurgitation, and dysphagia and an atypical, or “extraesophageal,” symptomatology that includes chronic cough, laryngitis, hoarseness, or even asthma. However, not all patients with typical symptoms might have GERD. The clinical presentation of GERD is therefore varied and poses certain challenges to the physician, especially considering the limitations of the diagnostic testing. In addition, most of patients with GERD symptoms are often placed on an empiric trial of antireflux medications, as suggested by the 2013 American College of Gastroenterology guidelines [2]. These patients might not have GERD, and the diagnosis of the underlying disease is often delayed [3]. In more dire circumstances, these false positives could be occasionally referred for an unnecessary antireflux operation [4].
The evaluation of patients with suspected GERD is often difficult and is based on the evaluation of clinical symptoms, objective evidence of reflux on diagnostic testing, correlation of symptoms with episodes of reflux, evaluation of anatomical abnormalities (e.g., presence of hiatal hernia), and ruling out other common causes for the patient’s symptoms. This complexity explains the absence of a golden standard single diagnostic test and the reason why the diagnostic evaluation should include multiple tests, such as barium swallow, upper endoscopy, esophageal high-resolution manometry and ambulatory 24-h pH monitoring in addition to a thorough clinical examination that includes the presence, duration, and severity of symptoms and their relief with antireflux medications [5]. A multidisciplinary panel of gastroenterologists and surgeons has developed guidelines on the evaluation of GERD and its diagnostic workup prior to antireflux surgery in 2013 [6]. This panel articulated an evidence and experience-based consensus that recommended a thorough symptomatic evaluation, endoscopy barium swallow, high-resolution impedance manometry (HIRM), ambulatory pH monitoring in all patients with suggestive symptoms of GERD. The panel recommended that a gastric emptying study and combined multichannel impedance pH (MII-pH) should be performed in selected patients [6].
Clinical evaluation
The clinical evaluation should address the presence, duration, and severity of typical “esophageal” (heartburn, regurgitation, and dysphagia) and atypical “extraesophageal” (chronic cough, hoarseness, chest pain) symptoms. Symptom questionnaires developed to aid the diagnosis of GERD, such as the Reflux Disease Questionnaire and the ReQuest symptom scale have modest sensitivity and specificity (65–75%) and are of limited diagnostic help [7, 8]. The clinical evaluation should address the trends in dosage, schedule, and effect of antireflux medications on symptom relief. Campos et al. [9] have shown that the clinical response to proton pump inhibitors (PPIs) together with the presence of typical symptoms and an abnormal pH monitoring can reliably diagnose GERD and become predictors of excellent outcomes of antireflux surgery. Conversely, not all patients with typical symptoms might have GERD. A study from Patti et al. [3] has shown that when the diagnosis of GERD is based exclusively on the presence of heartburn and regurgitation, about one-third of patients have a normal esophageal acid exposure. Furthermore, bloating, nausea, and diarrhea are unlikely manifestations of GERD and they should point out to other functional or organic diseases.
Diagnostic evaluation
Current applications of methodologies in gastroesophageal reflux disease testing are evolving [10]. In the absence of a golden standard single diagnostic test, the diagnostic evaluation of GERD should include a combination of endoscopy barium swallow, HRIM, ambulatory pH monitoring or MII-pH, and gastric emptying study, in selected cases.
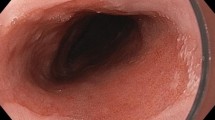
Upper endoscopy
The diagnostic yield of an upper endoscopy in the evaluation of GERD is limited to the detection of high-grade erosive esophagitis (Los Angeles Classification C and D), peptic stricture, and Barrett’s esophagus, findings that can indirectly support a diagnosis of GERD, or malignancy [6]. Additionally, an upper endoscopy helps excluding other differential diagnoses (e.g., gastritis, duodenitis, peptic ulcer disease, and non-reflux esophagitis of infectious or eosinophilic etiology).
Barium swallow
Although barium swallow is being increasingly supplanted by the upper endoscopy in the detection of anatomical abnormalities of the esophagus and stomach, the barium esophagram is still preferred in some centers as a helpful adjunct. This test has no diagnostic role per se, as the presence of reflux during the test does not correlate with the pH-monitoring data [11]. In fact, Bello et al. demonstrated the absence of any radiological sign of reflux in 53% of patients with GERD diagnosed by ambulatory 24-h pH monitoring. The diagnostic yield of a barium swallow in the evaluation of GERD is therefore limited to the identification of a concomitant hiatal hernia, a Schatzki ring (which can be missed on upper endoscopy given the difficulty of distending the distal esophagus with air), and an esophageal stricture.
High-resolution impedance manometry (HRIM)
Although HRIM does not diagnose GERD, it is a test that has a central role in the evaluation of patients with suspected GERD. In fact, HRIM can rule out primary esophageal motility disorders that present with symptoms similar to those with GERD, mainly achalasia, and can aid in the selection of candidates for a partial fundoplication—or a cardiomyotomy, when achalasia is detected. Achalasia in fact may be misdiagnosed as GERD, as heartburn—caused by chronic mucosal irritation by stasis of fermentation of food in an achalasic esophagus—could be present in addition to dysphagia (4). Esophageal manometry also identifies patients with severe abnormality of esophageal motility, such as those with scleroderma, for which a partial fundoplication is indicated [12, 13]. Finally, HRIM localizes the upper level of the lower esophageal sphincter in order to guide the proper placement of the MII-pH catheter. HRIM also provides information pressure and coordination of the hypopharynx and cricopharyngeal muscle. However, the utility of this information is limited to the research arena, as the diagnostic value of HRIM regarding potential association with a diagnosis of laryngopharyngeal reflux (LPR) is still largely unproven [14].
Ambulatory pH monitoring
Ambulatory pH monitoring provides objective evidence of abnormal reflux. It is almost always performed after antireflux medications are withheld for at least 7 days. Indications include clarification of the diagnosis of GERD in those patients with persistent symptoms on PPI or in those who complain of symptoms without endoscopic evidence of esophagitis or with endoscopic evidence of esophagitis Los Angeles Classification A and B, and in the pre- and postoperative evaluation of patients undergoing an antireflux operation [2, 6]. Preoperatively, a positive pH monitoring provides an objective measure of the amount of reflux, which is an important outcome predictor of surgery. In fact, Campos et al. [9] in their multivariate analysis on 199 patients showed that a positive pH monitoring was the strongest predictor of good outcomes after laparoscopic antireflux surgery and that 25% of patients with typical symptoms responding to antisecretory medications yet with a normal pH monitoring had worst outcomes. In addition, postoperative pH monitoring performed in patients with persisting or recurrent symptoms helps identifying failures reliably and direct medical treatment. In fact up to 70% of those who are placed on PPIs postoperatively do not have GERD on pH monitoring [13, 15]. The use of a dual sensor pH-monitoring catheter has also been described to be very helpful in assessing the amount of proximal reflux, often thought to be the cause of extraesophageal and otorhinolaryngologic manifestations [16].
The options available today for pH monitoring include MII-pH, BRAVO® pH capsule (Given Imaging, Yoqneam, Israel), and ResTech™ (Respiratory Technology Corporation, San Diego, CA, USA). The pro and cons of each method of pH testing are shown in Table 1. MII-pH is a catheter that monitors acid and non-acid reflux over 24-h and can detect the proximal extent of reflux. BRAVO® is a capsule deployed during an upper endoscopy and it monitors only acid reflux over 48–96 h. ResTech™ is a single-channel pH catheter placed in the oropharynx without need for manometry or endoscopy and has been used in the assessment of patients with suspected LPR. During testing, patients can document body position, meal times, and symptom events, which can eventually be used by the software to provide a statistical analysis of the correlation of the reflux event (acid or non-acid) with the symptoms [17].
Up until recently, the presence of abnormal reflux and the positive association with symptoms has been considered a diagnostic criterion for GERD. Today, the additional impedance data might offer potentially a more precise diagnosis of GERD especially when the symptom association probability (SAP) can be calculated for both acid and non-acid reflux. SAP is a statistical calculation that allows to reliably identify any meaningful or statistically significant association (when SAP is greater than 95%, which is equivalent to a p value <0.05) between the patient’s symptoms and the presence of acid or non-acid reflux [18]. Desjardin et al. [19] in a retrospective study on 33 patients demonstrated that a preoperative positive SAP was the only reflux parameter associated with favorable outcome after laparoscopic fundoplication for refractory reflux symptoms. Nevertheless, the role of abnormal non-acid reflux and the value of its association with symptoms are still under investigation, especially in those patients with extraesophageal manifestations of GERD [20]. In fact, Francis et al. evaluated 27 patients with objective evidence of GERD who underwent a fundoplication and found that traditional reflux parameters (heartburn with or without regurgitation and esophageal pH < 4 more than 12% of a 24-h period) and not impedance monitoring predicted outcomes [21].
Regarding the proximal location of reflux on MII-pH, studies have shown that this event might indicate LPR. However, we have recently showed that distinguishing whether LPR (or chronic cough and asthma) is caused by GERD remains challenging because investigators have used different methods to link these syndromes to reflux and the unreliability of diagnostic testing [14]. For these reasons, Jobe et al. [6] have recommended MII-pH only to those with symptoms refractory to PPIs and those with cough of unknown origin.
Finally, we have shown the usefulness of pH monitoring in a highly selected groups of patients such as those with scleroderma awaiting lung transplantation, with obesity, and idiopathic pulmonary fibrosis [22–24].
Gastric emptying testing
Gastroparesis may be associated with GERD, although in a very small percentage of patients. Galindo et al. [25] have shown objective evidence of gastroparesis by scintigraphy in 5.8% (16 out 275) of patients with symptoms of GERD. Because of this small prevalence, Jobe et al. have recommended that a radiolabeled gastric emptying study should not be performed routinely during the evaluation of patients with GERD in preparation for antireflux surgery. However, gastric emptying testing should be performed in selected cases: those with nausea and postprandial bloating, in patients with evidence of food in the stomach despite an overnight fast, and in patients with other risk factors such as diabetes and chronic opiate use. In cases of mild abnormality, a Nissen fundoplication might have a therapeutic effect, as this operation could improve gastric emptying by reducing the capacity of the fundus of the stomach [26].
Gastric emptying testing has been traditionally done by a radiolabeled study over 4 h. More recently, a new technology has been introduced that allows the simultaneous assessment of gastric emptying and the gastric acid secretion. The SmartPill® (Given Imaging, Yoqneam, Israel) is a pill that contains a wireless pH sensor that measures transit times and pH throughout the digestive tract and gastric acid output [27]. Although the role of gastric acid output in GERD remains poorly defined, the SmartPill® technology has a potential role in the clinical management of patients with GERD and disorders of gastric acid secretion.
Other methods to measure gastroesophageal reflux
Salivary pepsin (PepTest™, RD Biomed Limited, Hull, UK) is a simple, non-invasive and inexpensive test mainly used to aid in the diagnosis of LPR [28]. However, the test still has a limited value, as the cutoff values that predict the presence of LPR are not known. The sensitivity and specificity to detect LPR are comparable to symptom questionnaires, response to antireflux medications, and pH monitoring, highlighting the lack of a gold standard test for its diagnosis [14]. Our group has also shown that detection of pepsin in the bronchoalveolar fluid can be used as a diagnostic marker of aspiration and that laparoscopic antireflux surgery has a protective role against it [29, 30].
Special situations (end-stage lung diseases and lung transplants)
The evaluation of GERD in patients with end-stage lung diseases and lung transplants is particularly challenging. Today, many questions persist regarding the causal relationship between GERD and aspiration and its potential to induce both pulmonary demise and allograft failure. Recent studies have demonstrated a significant prevalence of GERD in patients with idiopathic pulmonary fibrosis (IPF), cystic fibrosis (CF), and connective tissue disorders (CTDs), such as scleroderma [31–34]. Work in this field has also attempted to elucidate the association between GERD and bronchiolitis obliterans syndrome (BOS) after lung transplantation and has shown: a) a possible connection between the development of GERD and the progression of BOS; and b) that effective control of GERD with laparoscopic antireflux surgery (LARS) can decrease the incidence of BOS [29, 35, 36]. In 2010, for instance, Davis et al. tried to determine the prevalence and extent of GERD, as well as risk factors, in lung transplant patients. In 35 consecutive patients, they found that more than half had GERD and that half of these patients had proximal reflux, which was more pronounced when supine, with predisposition to aspiration [34]. They also found that 36% of patients with GERD had ineffective esophageal motility compared with the 6% without GERD.
With increasing availability of HRIM and MII-pH, abnormalities in this category of patients have been better recognized [37]. A prospective study by Rhagu et al. [31] reported that 87% of 65 IPF patients had abnormal reflux. Allaix et al. attempted to characterize patterns of esophageal motility, reflux, and clinical presentations in 22 IPF patients compared with 80 controls with GERD. Interestingly, patients in both groups had similar profiles in terms of pH monitoring, esophageal motility, and LES function; however, IPF patients were 40% less likely to present with typical symptoms, had a higher incidence of hypotensive upper esophageal sphincter, demonstrated shorter duration of proximal and distal esophageal amplitudes on HRIM, and had significantly slower acid clearance and more frequent proximal reflux in the supine position when compared with the control group [38]. Davis et al. [39] confirmed these findings and showed no difference in manometric findings in IPF patients compared with those with other end-stage lung disease, as opposed to patients without GERD and no pulmonary involvement. The same authors showed that lung transplant patients with IPF were at increased risk for aspiration and had a greater frequency of acute rejection episodes [39]. They also found no difference in the findings of manometric, barium swallow, or gastric emptying study in IPF patients compared to those with other ESLDs, thus speculating that risk factors for aspiration may be different among those who had undergone transplantation [39]. A study that demonstrated the higher prevalence of GERD in patients according to the type of transplant they received, showed that patients who had undergone bilateral lung transplant or re-transplantation had GERD and proximal reflux, a likely proxy for aspiration, more frequently than those who received a unilateral lung transplant [40]. The authors of the study speculated that iatrogenic vagal nerve disruption could have played a role in causing GERD, as patients with GERD after bilateral or re-transplantation tended to have some indirect evidence of vagal nerve injury, such as a pronounced delayed gastric emptying, impaired esophageal motility, and delayed esophageal acid clearance, when compared to those who had received a unilateral lung transplant.
To date, the most successful management of GERD in patients with ESLD and after lung transplantation is LARS [29, 35]. Studies have shown that LARS is safe even in high-risk lung transplant patients. A study that analyzed morbidity and mortality of LARS in the lung transplant population compared to a control group, found that they were equivalent [41]. Interestingly, in this study lung transplant patients were more prone to proximal reflux, and thus possibly aspiration, than the general population with GERD [41]. Another study also showed that LARS could improve lung function, preventing GERD-induced aspiration. The detection of pepsin identified those who aspirated and that patients with LARS had minimal pepsin levels in their bronchoalveolar lavage fluid. Furthermore, those with GERD who did not have LARS had more pepsin, quicker progression to BOS, and more episodes of acute rejection, which could lead to chronic rejection [29]. The authors also speculated that the ability of LARS in preventing GERD-induced aspiration might modulate the pulmonary inflammatory environment [42].
Finally, the evidence herein reviewed supports an early evaluation for GERD in patients with end-stage lung disease and in those who had lung transplantation, especially bilaterally. The evaluation should be thorough and should include gastric emptying study and pepsin testing, where available, to assist in the decision making to proceed with LARS.
Conclusions
The evaluation of patients with suspected GERD might be challenging. It is based on the evaluation of clinical features, objective evidence of reflux on diagnostic testing, correlation of symptoms with episodes of reflux, evaluation of anatomical abnormalities, and excluding other causes that might account for the presence of the patient’s symptoms. The diagnostic evaluation should include multiple tests, in addition to a thorough clinical examination.
References
Vakil N, van Zanten SV, Kahrilas P, Dent K, Jones R, Global Consensus Group (2006) The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 101(8):1900–1920
Katz PO, Gerson LB, Vela MF (2013) Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 108(3):308–328
Patti MG, Diener U, Tamburini A, Molena D, Way LW (2001) Role of esophageal function tests in the diagnosis of gastroesophageal reflux disease. Dig Dis Sci 46:597–602
Andolfi C, Bonavina L, Kavitt RT, Konda VJ, Asti E, Patti MG (2016) Importance of esophageal manometry and ph monitoring in the evaluation of patients with refractory gastroesophageal reflux disease: a multicenter study. J Laparoendosc Adv Surg Tech A 26(7):548–550
Patti MG, Fisichella PM, Perretta S (2001) Preoperative evaluation of patients with gastroesophageal reflux disease. J Laparoendosc Adv Surg Tech A 11(6):327–331
Jobe BA, Richter JE, Hoppo T et al (2013) Preoperative diagnostic work-up before antireflux surgery: an evidence and experience-based consensus of the esophageal diagnostic advisory panel. J Am Coll Surg 217(4):586–597
Shaw M, Dent J, Beebe T, Junghard O, Wiklund I, Lind T, Johnsson F (2008) The Reflux Disease Questionnaire: a measure for assessment of treatment response in clinical trials. Health Qual Life Outcomes 6:31
Ducrotte P, Zerbib F (2007). ReQuest: a new questionnaire for the simultaneous evaluation of symptoms and well-being in patients with gastro-oesophageal reflux. Digestion, 75Suppl 1:79-86
Campos GM, Peters JH, DeMeester TR, Oberg S, Crookes PF, Tan S, DeMeester SR, Hagen JA, Bremner CG (1999) Multivariate analysis of factors predicting outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg 3:292–300
Weber C, Davis CS, Fisichella PM (2011) Current applications of evolving methodologies in gastroesophageal reflux disease testing. Dig Liver Dis 43(5):353–357
Bello B, Zoccali M, Gullo R et al (2013) Gastroesophageal reflux disease and antireflux surgery—What is the proper preoperative work-up? J Gastrointest Surg 17:14–20
Fisichella PM, Jalilvand A (2014) The role of impaired esophageal and gastric motility in end-stage lung diseases and after lung transplantation. J Surg Res 186(1):201–206
Andolfi C, Vigneswaran Y, Kavitt RT, Herbella FA, Patti MG (2017) Laparoscopic antireflux surgery: importance of patient’s selection and preoperative workup. J Laparoendosc Adv Surg Tech A 27(2):101–105. doi:10.1089/lap.2016.0322
Sidhwa F, Moore A, Alligood E, Fisichella PM. (2016) Diagnosis and treatment of the extraesophageal manifestations of gastroesophageal reflux disease. Ann Surg. Aug 5. PMID: 27455157
Lord RV, Kaminski A, Oberg S et al (2002) Absence of gastroesophageal reflux disease in a majority of patients taking acid suppression medications after Nissen fundoplication. J Gastrointest Surg 6:3–9
Herbella FA, Andolfi C, Vigneswaran Y, Patti MG, Pinna BR (2016) Importance of esophageal manometry and pH monitoring for the evaluation of otorhinolaryngologic (ENT) manifestations of GERD. A multicenter study. J Gastrointest Surg 20(10):1673–1678
Lo KW, Mashimo H (2017) Establishing the diagnosis of GERD. In: Fisichella PM (ed) Failed antireflux therapy: analysis of causes and principles of treatment. Springer-Verlag, London (in press)
Bredenoord AJ, Weustein BLAM, Smout AJPM (2005) Symptom association analysis in ambulatory gastro-oesophageal reflux monitoring. Gut 54(12):1810–1817
Desjardin M, Luc G, Collet D, Zerbib F (2015) 24-hour pH-impedance monitoring on therapy to select patients with refractory reflux symptoms for antireflux surgery. A single center retrospective study. Neurogastroenterol Motil 28(1):146–152
Francis DO, Goutte M, Slaughter JC et al (2011) Traditional reflux parameters and not impedance monitoring predict outcome after fundoplication in extraesophageal reflux. Laryngoscope 121(9):1902–1909
Lai Y-C, Wang P-C, Lin J-C (2008) Laryngopharyngeal reflux in patients with reflux esophagitis. World J Gastroenterol 14(28):4523–4528
Fisichella PM, Reder NP, Gagermeier J, Kovacs EJ (2014) Usefulness of pH monitoring in predicting the survival status of patients with scleroderma awaiting lung transplantation. J Surg Res 189(2):232–237
Fisichella PM, Patti MG (2009) Gastroesophageal reflux disease and morbid obesity: is there a relation? World J Surg 33(10):2034–2038. doi: 10.1007/s00268-009-0045-z
Allaix ME, Fisichella PM, Noth I, Herbella FA, Borraez Segura B, Patti MG (2014) Idiopathic pulmonary fibrosis and gastroesophageal reflux. Implications for treatment. J Gastrointest Surg 18(1):100–104
Galindo G, Vassalle J, Marcus SN, Triadafilopoulos G (2013) Multimodality evaluation of patients with gastroesophageal reflux disease symptoms who have failed empiric proton pump inhibitor therapy. Dis Esophagus 26(5):443–450
Bais JE, Samsom M, Boudesteijn EA, van Rijk PP, Akkermans LM, Gooszen HG (2001) Impact of delayed gastric emptying on the outcome of antireflux surgery. Ann Surg 234:139–146
Weinstein DH, deRijke S, Chow CC, Foruraghi L, Zhao X, Wright EC, Whatley M, Maass-Moreno R, Chen CC, Wank SA (2013) A new method for determining gastric acid output using a wireless ph-sensing capsule. Aliment Pharmacol Ther 37(12):1198–1209
Hayat JO, Yazaki E, Moore AT, Hicklin L, Dettmar P, Kang JY, Sifrim D (2014) Objective detection of esophago-pharyngeal reflux in patients with hoarseness and endoscopic signs of laryngeal inflammation. J Clin Gastroenterol 48(4):318–327
Fisichella PM, Davis CS, Lundberg PW, Lowery E, Burnham EL, Alex CG, Ramirez L, Pelletiere K, Love RB, Kuo PC, Kovacs EJ (2011) The protective role of laparoscopic antireflux surgery against aspiration of pepsin after lung transplantation. Surgery 150(4):598–606
Fisichella PM, Davis CS, Gagermeier J, Dilling D, Alex CG, Dorfmeister JA, Kovacs EJ, Love RB, Gamelli RL (2011) Laparoscopic antireflux surgery for gastroesophageal reflux disease after lung transplantation. J Surg Res 170(2):e279–e286
Rhagu G, Freudenberger TD, Yang S et al (2006) High prevalence of abnormal acid gastro-oesophageal reflux in idiopathic pulmonary fibrosis. EurRespir J 27:136
Mendez BM, Davis CS, Weber C, Joehl RJ, Fisichella PM (2012) Gastroesophageal reflux disease in lung transplant patients with cystic fibrosis. Am J Surg 204:21
Patti MG, Gasper WJ, Fisichella PM, Nipomnick I, Palazzo F (2008) Gastroesophageal reflux disease and connective tissue disorders: pathophysiology and implications for treatment. J Gastrointest Surg 12:1900. doi:10.1007/s11605-008-0674-9 Epub 2008 Sep 3
Davis CS, Shankaran V, Kovacs EJ, et al. (2010) Gastroesophageal reflux disease after lung transplantation: pathophysiology and implications for treatment. Surgery, 148:737. Discussion 744e5
Hartwig MG, Davis RD (2012) Gastroesophageal reflux disease induced aspiration injury following lung transplantation. Curr Opin Organ Transplant 17:474
Hoppo T, Jarido V, Pennathur A et al (2011) Antireflux surgery preserves lung function in patients with gastroesophageal reflux disease and end-stage lung disease before and after lung transplantation. Arch Surg 146:1041
Basseri B, Conklin JL, Pimentel M et al (2010) Esophageal motor dysfunction and gastroesophageal reflux are prevalent in lung transplant candidates. Ann Thorac Surg 90:1630
Allaix ME, Fisichella PM, Herbella FA, Patti MG (2014) Idiopathic pulmonary fibrosis and gastroesophageal reflux. Implications for treatment. J Gastrointest Surg Jan;18(1):100-4; discussion 104-5. doi: 10.1007/s11605-013-2333-z
Davis CS, Mendez BD, Flint DV et al (2013) Pepsin concentrations are elevated in the bronchoalveolar lavage fluid of patients with idiopathic pulmonary fibrosis after lung transplantation. J Surg Res. doi:10.1016/j.jss.2013.06.011.:S0022-4804(13)00600-8
Fisichella PM, Davis CS, Shankaran V et al (2012) The prevalence and extent of gastroesophageal reflux disease correlates to the type of lung transplantation. Surg Laparosc Endosc Percutaneous Tech 22:46
Fisichella PM, Davis CS, Gagermeier J et al (2011) Laparoscopic antireflux surgery for gastroesophageal reflux disease after lung transplantation. J Surg Res 170:279
Fisichella PM, Davis CS, Lowery E et al (2012) Pulmonary immune changes early after laparoscopic antireflux surgery in lung transplant patients with gastroesophageal reflux disease. J Surg Res 177:E65
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare
Rights and permissions
About this article
Cite this article
Fisichella, P.M., Andolfi, C. & Orthopoulos, G. Evaluation of Gastroesophageal Reflux Disease. World J Surg 41, 1672–1677 (2017). https://doi.org/10.1007/s00268-017-3953-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-3953-3