Abstract
Gastroesophageal reflux disease (GERD) is highly prevalent in morbidly obese patients, and a high body mass index (BMI) is a risk factor for the development of GERD. However, the mechanism by which the BMI affects esophageal acid exposure is not completely understood. Although many advances have been made in the understanding of the pathophysiology of GERD, many aspects of the pathophysiology of this disease in morbidly obese patients remain unclear. The following review describes the current evidence linking esophageal reflux to obesity, covering the pathophysiology of the disease and the implications for treatment of GERD in the obese patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obesity has reached epidemic proportions. In the United States, 32% of the adult population is obese [1]. Similarly, the prevalence of gastroesophageal reflux disease (GERD) has increased up to 20% in the Western world [2]. In addition, some studies have shown that GERD is highly prevalent in morbidly obese patients and that a high body mass index (BMI) is a risk factor for the development of GERD [2–4]. The mechanism by which BMI affects esophageal acid exposure is not completely understood. It has been suggested that increased intragastric pressure [5], increased transdiaphragmatic gastroesophageal pressure gradient [6], incompetence of the lower esophageal sphincter (LES) [7], and increased frequency of transient LES relaxations [8] may all play a role in the pathophysiology of the disease in morbidly obese patients. To support the hypothesis that obesity increases esophageal acid exposure is the documented relation between increased BMI and the prevalence of GERD and its complications [9–11].
Although many advances have been made in our understanding of the pathophysiology of GERD, many aspects of the pathophysiology of this disease in morbidly obese patients remain unclear. It has been suggested that the pathophysiology of GERD in morbidly obese patients might differ from that of nonobese patients [12]. The therapeutic implication is that correction of reflux in morbidly obese patients might need a different approach.
Prevalence of obesity and GERD
The prevalence of obesity has reached epidemic proportions in the United States. The analysis of height and weight measurements from 3958 children and adolescents aged 2 to 19 years and 4431 adults aged 20 years or older obtained during 2003–2004 as part of the National Health and Nutrition Examination Survey (NHANES) showed that 17% of children and adolescents were overweight, and 32% of adults were obese [1]. This study also showed a worrisome increased trend among children, adolescents, and men. The prevalence of overweight female children and adolescents increased from 14% in 1999–2000 to 16% in 2003–2004; the prevalence of overweight in male children and adolescents increased from 14% to 18%. Among men, the prevalence of obesity increased from 27% in 1999–2000 to 31% in 2003–2004. Among women, no significant increase in obesity was observed between 1999–2000 (33%) and 2003–2004 (33%) [1].
Similarly, the prevalence of GERD has paralleled the increasing prevalence of obesity. A systematic review of 15 epidemiologic studies showed that the prevalence of GERD in the Western world is 20% [2]. In addition, this and other studies found that obesity was a potential risk factor for the development of GERD [3, 4]. For example, increasing prevalence of GERD was associated with higher BMI in two large population cross-sectional studies: the Olmsted County study in the United States and the Bristol Helicobacter Project in Europe [3, 4].
The Olmsted County study was a cross-sectional study conducted in an age- and sex-stratified random sample of the population of Olmsted County, Minnesota. Residents aged 25 to 74 years were mailed a questionnaire that measured reflux symptoms and assessed potential risk factors. Logistic regression analysis showed that a BMI > 30 kg/m2 was associated with frequent (at least weekly) reflux symptoms [odds ratio (OR) 2.8; confidence interval (CI) 1.7–4.5] [3].
The Bristol Helicobacter Project was a randomized controlled trial of eradication of Helicobacter pylori infection in southwest England [13]. From this study, a cross-sectional population-based study was designed to examine the relation between BMI and GERD in a large sample representative of the population of England (10,537 subjects, aged 20–59 years). The study concluded that obesity (BMI >30 kg/m2) significantly increased the likelihood of suffering from GERD and that obese people were almost three times as likely to suffer from GERD as those with normal weight (BMI ≤ 30 kg/m2) [4].
Relation between GERD and obesity
The simultaneous and parallel increase in the prevalence of obesity and GERD over the past decades has led to the hypothesis that obesity may contribute to GERD. To support this hypothesis is the documentation of a dose–response relation between increasing BMI and prevalence of GERD and its complications, such as esophagitis and Barrett’s esophagus [4, 9–11]. For example, a BMI ≥ 25 kg/m2 was found to be associated with a 2.5-fold increased risk of Barrett’s esophagus in a retrospective cross-sectional study in male veterans [10]. However, these observations were not adjusted for other confounding factors, such as the type of diet consumed. It can be argued that consumption of a diet rich in fat, rather than being overweight encourages the development of GERD. However, a cross-sectional study performed on a random sample of Veterans Administration (VA) employees showed that the observed, strong, dose relation between BMI and GERD (twofold increase in the association between obesity and GERD and two- to four-fold increase in the association between obesity and erosive esophagitis) remained unchanged after adjusting for the type of dietary intake [9].
Two recent studies confirmed that obesity is also a risk factor for esophageal adenocarcinoma. One study investigated the association between BMI and prevalence of esophageal cancer in about 500,000 people in the United States and found that a BMI ≥ 35 kg/m2 was associated with an increased risk of esophageal cancer [hazard ratio (HR) 2.27, 95% CI 1.44–3.59] and that increased adiposity was associated with higher risk of esophageal cancer even within the normal weight range [14]. Another study from Europe investigated the prevalence of central adiposity, metabolic syndrome, and a proinflammatory state in patients with Barrett’s esophagus and found that the proinflammatory impact of adipocytokines associated with the metabolic syndrome of central adiposity may play an important role in the pathogenesis of esophageal cancer [15]. The authors found that 46% of Barretts’ patients had metabolic syndrome and 78% were centrally obese. In addition, 60% of patients with long-segment Barrett’s esophagus had metabolic syndrome, and 92% were centrally obese compared with 24% and 62% of patients, respectively, with short-segment Barrett’s esophagus. Moreover, patients with long-segment Barrett’s esophagus had increased levels of interleukin-6 compared with patients with short-segment Barrett’s esophagus.
The implications of the results of these studies are important as these findings emphasize the importance of the preoperative endoscopic evaluation in patients with GERD and postoperative surveillance in patients with Barrett’s esophagus. Melstrom et al., in their retrospective review, identified three patients (of 2875, or 0.1%) who developed esophageal cancer: two after Roux-en-Y gastric bypass and one after vertical banded gastroplasty [16]. All three patients had complaints of reflux, and two were treated with esophagectomy. The third patient presented with invasive carcinoma and died 2 years after diagnosis. Similarly, Allen et al. [17] observed that three patients developed esophageal cancer: two patients after Roux-en-Y gastric bypass and one after vertical banded gastroplasty. The intervals between the weight-loss operations and cancer diagnoses were 21, 16, and 14 years, respectively. All three patients had had symptoms of reflux for many years before dysphagia developed and cancer was diagnosed.
Obesity is therefore an independent risk factor for GERD and its complications. It seems that the risk of developing GERD and its complications increases with increasing weight. However, the mechanism by which obesity increases the risk of GERD is unknown.
How does obesity increase the risk of GERD?
Many aspects of the pathophysiology of GERD in morbidly obese patients remain unclear. In particular, the mechanism by which the increase in BMI increases the risk of GERD is not completely understood. Increased intraabdominal pressure may play a role in the pathogenesis of GERD, as may other co-morbidities. The effects of increased intraabdominal pressure in obesity are well known: increased pleural pressure, cardiac filling pressures, femoral venous pressure, renal venous pressure, systemic blood pressure, vascular resistance, renin and aldosterone levels, and intracranial pressure. Therefore, the co-morbidities caused by increased intraabdominal pressure in obese patients include congestive heart failure, hypoventilation, venous stasis ulcers, urinary stress incontinence, incisional hernia, pseudotumor cerebri, proteinuria, systemic hypertension, and GERD [18]. Specifically, it has been shown that the increase in BMI increases esophageal acid exposure [19]. To explain this finding, it has been suggested that obese patients may experience increased intraabdominal pressure that results in extrinsic gastric compression by visceral fat with a subsequent increase in intragastric pressure [5], increased gastroesophageal pressure gradient [6], and increased risk for developing a hiatal hernia [6], a known risk factor for GERD [20]. Altogether, these factors would promote retrograde flow of gastric contents into the esophagus. Other factors that play a role in the pathophysiology of GERD in nonobese patients, such as incompetence of the LES [7] and increased frequency of transient LES relaxations [8], are also thought to play a role in the pathophysiology of the disease in morbidly obese patients.
We have suggested that the pathophysiology of GERD in morbidly obese patients might differ from that of nonobese patients [12]. Nonobese patients with GERD have a mechanically defective LES [21], and about 45% to 60% have abnormal peristalsis [22, 23]. The more abnormal the esophageal peristalsis (lower amplitude of contractions and higher number of nonpropagating waves) the worse is the reflux [22]. In contrast to these observations, we found that morbidly obese patients with GERD had higher LES pressure and higher amplitude of contractions than nonobese patients [12]. In addition, only 10% of morbidly obese patients had hypotensive peristalsis. However, the DeMeester score was similar in the two groups. The finding of a low prevalence (14–21%) of a mechanically defective LES and abnormal peristalsis among obese patients has also been documented by others [24–26]. The meaning of these findings is unclear, but it might reflect a physiologic compensatory response to other factors present in morbidly obese patients, such as increased intragastric pressure [6]. Our linear regression model showed that the BMI, LES pressure, LES abdominal length, and distal esophageal amplitude (DEA) were independently associated with the DeMeester score. After adjustments for these variables, as well as for age and sex, the BMI remained independently associated with the DeMeester score. For each five-point increase in BMI, the DeMeester score was expected to increase by three units [12]. This model helped us explain finding similar DeMeester scores for obese and nonobese patients. The stronger LES and the more vigorous peristalsis among the morbidly obese patients may represent a compensatory mechanism that counteracts the effect of weight on the gastroesophageal junction, thereby limiting the amount of reflux.
Implications for treatment of morbidly obese patients with GERD
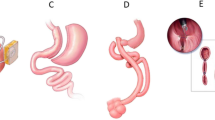
The common causes of reflux in nonobese patients (hypotensive LES and abnormal esophageal peristalsis) occur less frequently in the morbidly obese population. These findings should be taken into account when planning surgical therapy for reflux in morbidly obese patients because surgical correction of reflux in these patients might not be best achieved with an antireflux procedure. The effect of a fundoplication is due to its action at the level of the gastroesophageal junction. In morbidly obese patients, the increased weight imposes a stress on the gastroesophageal junction and promotes retrograde flow of gastric contents into the esophagus.
Although some have reported good results of laparoscopic Nissen fundoplication independent from the patient’s weight [27–30], others have shown a high recurrence rate of reflux in the obese patients [31, 32]. For instance, Perez and colleagues studied the recurrence rate of reflux among 224 patients who underwent either a transthoracic Belsey Mark IV or a transabdominal Nissen fundoplication [31]. Patients were divided into three groups based on their BMI (<25, 25.0–29.9, and ≥30 kg/m2). They found a significantly higher recurrence rate among the obese patients, which was independent of the type of operation. The authors suggested that factors such as elevated intraabdominal pressure may overcome the effect of the fundoplication. In addition, long-term follow-up (11 years) obtained from 166 patients who underwent laparoscopic Nissen fundoplication between 1992 and 1995 showed that preoperative morbid obesity (BMI ≥ 35 kg/m2) was associated with failure (p = 0.036) [32]. On the other hand, a Roux-en-Y gastric bypass might have a more pronounced and durable effect owing to the induced weight loss, the negligible number of parietal cells in the gastric pouch, and complete elimination of the gastroduodenal reflux [33–35].
Csendes studied the effect of Roux-en-Y gastric bypass on 12 morbidly obese patients [30]. Seven patients had short-segment Barratt’s esophagus (BE), and five patients had a long-segment BE. Two years after surgery, the BMI decreased from 43.2 to 29.4 kg/m2; and 1 year after surgery, symptoms of GERD disappeared in all patients. Erosive esophagitis healed in all patients. There was regression from intestinal metaplasia to cardiac mucosa in four patients (57%) with short-segment BE and in one patient (20%) with long-segment BE. There was no progression to dysplasia.
Future studies should prospectively compare the efficacy of laparoscopic antireflux and bariatric procedures in relation to the presence of GERD and morbid obesity.
References
Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM (2006) Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 295:1549–1555
Dent J, El-Serag HB, Wallander MA, Johansson S (2005) Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 54:710–717
Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd (1999) Risk factors associated with symptoms of gastroesophageal reflux. Am J Med 106:642–649
Murray L, Johnston B, Lane A, Harvey I, Donovan J, Nair P, Harvey R (2003) Relationship between body mass and gastro-oesophageal reflux symptoms: the Bristol Helicobacter Project. Int J Epidemiol 32:645–650
El-Serag HB, Tran T, Richardson P, Ergun G (2006) Anthropometric correlates of intragastric pressure. Scand J Gastroenterol 41:887–891
Pandolfino JE, El-Serag HB, Zhang Q, Shah N, Ghosh SK, Kahrilas PJ (2006) Obesity: a challenge to esophagogastric junction integrity. Gastroenterology 130:639–649
Merrouche M, Sabaté JM, Jouet P, Harnois F, Scaringi S, Coffin B, Msika S (2007) Gastro-esophageal reflux and esophageal motility disorders in morbidly obese patients before and after bariatric surgery. Obes Surg 17:894–900
Wu JC, Mui LM, Cheung CM, Chan Y, Sung JJ (2007) Obesity is associated with increased transient lower esophageal sphincter relaxation. Gastroenterology 132:883–889
El-Serag HB, Graham DY, Satia JA, Rabeneck L (2005) Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am J Gastroenterol 100:1243–1250
Stein DJ, El-Serag HB, Kuczynski J, Kramer JR, Sampliner RE (2005) The association of body mass index with Barrett’s oesophagus. Aliment Pharmacol Ther 22:1005–1010
Hampel H, Abraham NS, El-Serag HB (2005) Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med 143:199–211
Herbella FA, Sweet MP, Tedesco P, Nipomnick I, Patti MG (2007) Gastroesophageal reflux disease and obesity: pathophysiology and implications for treatment. J Gastrointest Surg 11:286–290
Lane JA, Harvey RF, Murray LJ, Harvey IM, Donovan JL, Nair P, Egger M (2002) A placebo-controlled randomized trial of eradication of Helicobacter pylori in the general population: study design and response rates of the Bristol Helicobacter Project. Control Clin Trials 23:321–332
Abnet CC, Freedman ND, Hollenbeck AR, Fraumeni JF Jr, Leitzmann M, Schatzkin A (2008) A prospective study of BMI and risk of oesophageal and gastric adenocarcinoma. Eur J Cancer 44:465–471
Ryan AM, Healy LA, Power DG, Byrne M, Murphy S, Byrne PJ, Kelleher D, Reynolds JV (2008) Barrett esophagus: prevalence of central adiposity, metabolic syndrome, and a proinflammatory state. Ann Surg 247:909–915
Melstrom LG, Bentrem DJ, Salvino MJ, Blum MG, Talamonti MS, Printen KJ (2008) Adenocarcinoma of the gastroesophageal junction after bariatric surgery. Am J Surg 196:135–138
Allen JW, Leeman MF, Richardson JD (2004) Esophageal carcinoma following bariatric procedures. JSLS 8:372–375
Sugerman HJ (2001) Effects of increased intra-abdominal pressure in severe obesity. Surg Clin North Am 81:1063–1075
El-Serag HB, Ergun GA, Pandolfino J, Fitzgerald S, Tran T, Kramer JR (2007) Obesity increases oesophageal acid exposure. Gut 56:749–755
Patti MG, Goldberg HI, Arcerito M, Bortolasi L, Tong J, Way LW (1996) Hiatal hernia size affects lower esophageal sphincter function, esophageal acid exposure, and the degree of mucosal injury. Am J Surg 171:182–186
Zaninotto G, DeMeester TR, Schwizer W, Johansson KE, Cheng SC (1988) The lower esophageal sphincter in health and disease. Am J Surg 155:104–111
Diener U, Patti MG, Molena D, Fisichella PM, Way LW (2001) Esophageal dysmotility and gastroesophageal reflux disease. J Gastrointest Surg 5:260–265
Kahrilas PJ, Dodds WJ, Hogan WJ, Kern M, Arndorfer RC, Reece A (1986) Esophageal peristaltic dysfunction in peptic esophagitis. Gastroenterology 91:897–904
Di Francesco V, Baggio E, Mastromauro M, Zoico E, Stefenelli N, Zamboni M, Panourgia MP, Frulloni L, Bovo P, Bosello O, Cavallini G (2004) Obesity and gastro-esophageal acid reflux: physiopathological mechanisms and role of gastric bariatric surgery. Obes Surg 14:1095–1102
Suter M, Dorta G, Giusti V, Calmes JM (2004) Gastro-esophageal reflux and esophageal motility disorders in morbidly obese patients. Obes Surg 14:959–966
Weiss HG, Nehoda H, Labeck B, Peer-Kühberger MD, Klingler P, Gadenstätter M, Aigner F, Wetscher GJ (2000) Treatment of morbid obesity with laparoscopic adjustable gastric banding affects esophageal motility. Am J Surg 180:479–482
Fraser J, Watson DI, O’Boyle CJ, Jamieson GG (2001) Obesity and its effect on outcome of laparoscopic Nissen fundoplication. Dis Esophagus 14:50–53
Winslow ER, Frisella MM, Soper NJ, Klingensmith ME (2003) Obesity does not adversely affect the outcome of laparoscopic antireflux surgery (LARS). Surg Endosc 17:2003–2011
Anvari M, Bamehriz F (2006) Outcome of laparoscopic Nissen fundoplication in patients with body mass index > or = 35. Surg Endosc 20:230–234
D’Alessio MJ, Arnaoutakis D, Giarelli N, Villadolid DV, Rosemurgy AS (2005) Obesity is not a contraindication to laparoscopic Nissen fundoplication. J Gastrointest Surg 9:949–954
Perez AR, Moncure AC, Rattner DW (2001) Obesity adversely affects the outcome of antireflux operations. Surg Endosc 15:986–989
Morgenthal CB, Lin E, Shane MD, Hunter JG, Smith CD (2007) Who will fail laparoscopic Nissen fundoplication? Preoperative prediction of long-term outcomes. Surg Endosc 21:1978–1984
Frezza EE, Ikramuddin S, Gourash W, Rakitt T, Kingston A, Luketich J, Schauer P (2002) Symptomatic improvement in gastroesophageal reflux disease (GERD) following laparoscopic Roux-en-Y gastric bypass. Surg Endosc 16:1027–1031
Patterson EJ, Davis DG, Khajanchee Y, Swanström LL (2003) Comparison of objective outcomes following laparoscopic Nissen fundoplication versus laparoscopic gastric bypass in the morbidly obese with heartburn. Surg Endosc 17:1561–1565
Csendes A, Burgos AM, Smok G, Burdiles P, Henriquez A (2006) Effect of gastric bypass on Barrett’s esophagus and intestinal metaplasia of the cardia in patients with morbid obesity. J Gastrointest Surg 10:259–264
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fisichella, P.M., Patti, M.G. Gastroesophageal Reflux Disease and Morbid Obesity: Is There a Relation?. World J Surg 33, 2034–2038 (2009). https://doi.org/10.1007/s00268-009-0045-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0045-z