Abstract
Background
Fast-track surgery (FTS) is a promising program for surgical patients and has been applied to several surgical diseases. FTS is much superior to conventional perioperative care. Our aim was to evaluate and compare the safety and efficacy of FTS and conventional perioperative care for patients undergoing gastrectomy using a systematic review.
Methods
We searched the literature in PubMed, SCOPUS, and EMBASE up to November 2013. No language restriction was applied. Weighted mean differences (WMDs) and odds ratios (ORs) with their 95 % confidence intervals (CIs) were used for analysis by a fixed or a random effects model according to the heterogeneity assumption.
Results
In the present meta-analysis, we included five randomized controlled trials and one controlled clinical trial from five studies. Compared with conventional care, FTS shortened the duration of flatus (WMD −21.08; 95 % CI −27.46 to −14.71, z = 6.48, p < 0.00001 in the open surgery group; WMD −8.20; 95 % CI −12.87 to −3.53, z = 3.44, p = 0.0006 in the laparoscopic surgery group), accelerated the decrease in C-reactive protein (WMD −15.56; 95 % CI 21.28 to 9.83, z = 5.33, p < 0.00001), shortened the postoperative stay (WMD −2.00; 95 % CI −2.69 to −1.30, z = 5.64, p < 0.00001), and reduced hospitalization costs (WMD −447.72; 95 % CI −615.92 to −279.51, z = 5.22, p < 0.00001). FTS made no significant difference in operation times (p = 0.93), intraoperative blood loss (p = 0.79), or postoperative complications (p = 0.07).
Conclusions
Based on current evidence, the FTS protocol was feasible for gastric cancer patients who underwent gastrectomy (distal subtotal gastrectomy, proximal subtotal gastrectomy, or radical total gastrectomy) via open or laparoscopic surgery. Larger studies are needed to validate our findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fast-track surgery (FTS) was first initiated by the Danish surgeon Kehlet [1, 2] in the field of elective colorectal surgery during the 1990s. Since then, it has been rapidly popularized worldwide because of its significant benefits and safety [3]. The core components of FTS include epidural or regional anesthesia, perioperative fluid management, minimally invasive techniques, optimal pain control, early initiation of oral feeding, and early mobilization, among others (Table 1) [4]. These joint approaches have resulted in a significant reduction in complication rates, morbidity and mortality rates, duration of hospital stay, and hospitalization costs. Also, the combination of these approaches reduced stress response and organ dysfunction, thereby greatly shortening the time required for full recovery [5–7]. In recent years, FTS has been applied to several surgical situations, include radical prostatectomy [8], cardiac surgery [9], total knee replacement [10], cesarean section [11], and coronary artery bypass grafting [12]. It has also been used for specific procedures in children [13] and the elderly [14].
Gastric cancer (GC) is the fourth most common cancer worldwide and the second leading cause of cancer mortality. It has been reported that China, Japan, South America, Eastern Europe, and parts of the Middle East have the highest incidence of GC [15]. Approximately 4,00,000 cases of GC are diagnosed in China annually [16], and more than one million cases are diagnosed worldwide.
Up to now, surgery has been the most common treatment for early-stage GC. However, conventional gastrectomy is associated with a complication rate of 10 to 45 % and a postoperative hospital stay of 8 to 13 days [17–20]. A high rate of serious postoperative complications has been linked to an excessive response to surgical stress [21–23]. C-reactive protein (CRP), interleukin-6, tumor necrosis factor-α, and resting energy expenditure may be markers indicating the severity of the surgical stress response [24–26]. FTS is based on reducing surgical stress using various surgical and anesthetic approaches to aid faster recovery.
In contrast to a positive and promising attitude about FTS, some studies have demonstrated that routine nasogastric decompression, intraabdominal drainage, and fasting after gastrectomy were unnecessary and were not beneficial to recovery [19, 20, 27, 28]. Because reports on FTS for GC are rare and a single study would likely lack credibility, we performed a meta-analysis of the published literature to determine the feasibility and safety of fast-track rehabilitation programs in patients with GC and to quantify the potential between-study heterogeneity.
Materials and methods
Publication search
Two of the authors (Y.L., T.H.) independently performed a bibliographic search in PubMed, SCOPUS, and EMBASE using the following terms: (“fast-track surgery” or “FTS” or “fast track perioperative care”) and (“gastric cancer” or “GC”). No language restriction was applied. All of the studies found were retrieved, and their references were checked as well for other relevant publications. Review articles were also looked up to find additional eligible studies. The inclusion criteria were (1) evaluation of FTS comparison with conventional care, (2) randomized controlled trials (RCTs) or controlled clinical trials (CCTs), (3) diagnosis of GC based on clinical symptoms, imaging, and pathology. The included studies met all of these criteria. Authors with more than one published study were represented by their most recent publication to avoid multiple reporting of patients. Each article was checked by an associate professor.
Studies were excluded if they (1) were not RCTs, (2) did not compare FTS and conventional care, (3) applied fewer than four elements of FTS, (4) were in a language for which a translation to English was not available, and (5) were unpublished studies with only the abstracts presented at national and international meetings.
Data extraction
The following information was extracted from each study: the first author, published year, country of study population, number, age, sex, body mass index (BMI) and TNM classification of both cases and controls (Table 2). Documentation was extracted from all the publications, independently by two of the authors (Y.L., J.X.). Disagreement was resolved by discussion between the authors. If they could not reach a consensus, the professor adjudicated the disagreement. Six outcome variables were considered suitable for analyzing the efficacy of FTS: operation time, intraoperative blood loss, duration of flatus, CRP, postoperative hospital stay, cost of hospitalization. Postoperative complications were used to assess the safety of FTS. Postoperative hospital stay was calculated from the date of operation to the date of discharge, and all of the costs of hospitalization were calculated by U.S. Dollar. The quality of the RCTs was assessed by two of the authors (Y.L., J.X.) using the Jadad scoring system [29] (Table 3).
Statistical methods
Weighted mean differences (WMDs) and their 95 % confidence intervals (CIs) were used to analyze continuous variables presented in the same scale by a fixed effects model or a random effects model according to the heterogeneity assumption (operation time, intraoperative blood loss, duration of flatus, CRP, postoperative hospital stay, hospitalization cost). p of Q test > 0.1 and I 2 < 50 % indicated a lack of heterogeneity. This outcome was calculated by a fixed effects model. p of Q test < 0.1 and I 2 > 50 % indicated a random effects model. Odds ratios (ORs) and 95 % CIs were used to analyze postoperative complications. If the study provided medians and interquartile ranges instead of means and standard deviations (SDs), we imputed the means and SDs as described by Hozo et al. [30]. Publication bias may be present when there are fewer than 10 studies in a meta-analysis because the low number implies inherent weaknesses in the review. Therefore, we did not emphasize publication bias results. All above of the statistical analyses were performed using RevMan 5.2.0 software (Cochrane-information Management System).
Results
Article search
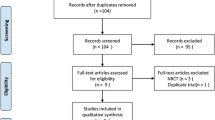
The initial literature search identified 21 studies. Based on the inclusion criteria, 15 studies were excluded, leaving 6 studies to be subjected to a more detailed review. One RCT was excluded because the repeating data from a same group published at a different time [31]. Finally, five RCTs were included [32–36], and the study of Hu et al. [34] can be treat as two independent research studies in that they separately reported the effects and safety of FTS for open and laparoscopic gastrectomy surgery, whereas we perform a subgroup analysis according to open or laparoscopic gastrectomies in our RCT. Therefore, six related studies from five RCTs were included for the meta-analysis (Fig. 1). Characteristics of each trial are given in Table 2. There were 206 patients in the FTS group and 211 in the conventional care group.
Methodologic quality of the included studies
The methodologic quality of the included trials is explained comprehensively in Table 3. in general, the quality of the studies was moderate to good (all ≥ 3). All data were analyzed in accordance with the intention-to-treat principle.
Operation time
Four studies reported the operation time. There was no significant heterogeneity among the trials (I 2 = 0 %, p = 0.46), neither between the laparoscopic and open surgery groups by subgroup analysis (I 2 = 0 %, p = 0.37). In the fixed-effects models, there was no significant difference in operation time between the FTS and conventional treatment groups (WMD 0.47; 95 % CI −9.79 to 10.72, z = 0.09, p = 0.93) (Fig. 2).
Intraoperative blood loss
Four studies mentioned intraoperative blood loss. There was no significant heterogeneity among the trials (I 2 = 0 %, p = 0.59), neither between the Laparoscopic and Open groups by subgroup analysis (I 2 = 0 %, p = 0.74). In fixed-effects models, there was no significant difference in intraoperative blood loss between the FTS and Conventional groups (WMD 2.02; 95 % CI −12.75 to 16.80, z = 0.27, p = 0.79) (Fig. 3).
Meta-analysis of FTS versus conventional care for intraoperative blood loss. See Fig. 2 for description of symbols
Duration of flatus
All studies analyzed duration of flatus. We extracted relevant data and performed a meta-analysis between FTS and conventional perioperative care grouped by type of surgery. The heterogeneity among the trials was significant (I 2 = 87 %, p < 0.00001), indicating a random effects model. The duration of flatus of patients undergoing FTS was 21.08 h less than those undergoing conventional perioperative care in the open surgery group (WMD −21.08; 95 % CI −27.46 to −14.71, z = 6.48, p < 0.00001) (Fig. 4). In the laparoscopic group, the duration of flatus of patients undergoing FTS was 8.20 h less than that of the controls (WMD −8.20; 95 % CI −12.87 to −3.53, z = 3.44, p = 0.0006) (Fig. 4).
Meta-analysis of FTS versus conventional care for duration of flatus. See Fig. 2 for description of symbols
C-reactive protein
C-reactive protein is a by-product of inflammation usually found in the blood of some acute cases and can be regard as a marker of the severity of the surgical stress response. Four of the six studies recorded CRP levels on days 1 and 3 or 4, 5, or 7 after surgery. The heterogeneity among the trials was significant (I 2 = 70 %, p = 0.0001), indicating a random effects model. In addition to the groups on postoperative day (POD) 1 (z = 0.02, p = 0.99) and POD 5 or 7 (z = 1.34, p = 0.18) who underwent laparoscopic surgery, other subgroup analyses indicated a decrease of CRP in the FTS patients. Overall, the CRP level of patients undergoing FTS was 15.56 mg/L less than in those undergoing conventional perioperative care in the open surgery group (WMD −15.56; 95 % CI −21.28 to −9.83, z = 5.33, p < 0.00001) (Fig. 5).
Meta-analysis of FTS versus conventional care for C-reactive protein. See Fig. 2 for description of symbols
Postoperative hospital stay
All studies recorded the postoperative hospital stay. There was significant heterogeneity among the trials (I 2 = 88 %, p < 0.00001). In the random effects model, the postoperative hospital stay of patients undergoing FTS was 2.00 days less than for those undergoing conventional perioperative care overall (WMD −2.00; 95 % CI −2.69 to −1.30, z = 5.64, p < 0.00001) (Fig. 6). This difference was notable in the open surgery group.
Meta-analysis of FTS versus conventional care for postoperative hospital stay. See Fig. 2 for description of symbols
Cost of hospitalization
All six studies calculated the cost of hospitalization. There was a significant heterogeneity of the trials in the open surgery group (I 2 = 64 %, p = 0.04) but not in laparoscopic group. In the random effects model, the cost of hospitalization of patients undergoing FTS was $447.72 less than for those undergoing conventional perioperative care overall (WMD −447.72; 95 % CI −615.92 to −279.51, z = 5.22, p < 0.00001) (Fig. 7).
Meta-analysis of FTS versus conventional care for cost of hospitalization. See Fig. 2 for description of symbols
Postoperative complications
Four studies reported postoperative complications. There was no significant heterogeneity among the studies (I 2 = 35 %, p = 0.20). In fixed-effects models, there was no significant difference in postoperative complications between the FTS and conventional perioperative care groups (OR 0.59; 95 % CI 0.33 to 1.05, z = 1.79, p = 0.07) (Fig. 8).
Discussion
The aim of this study was to evaluate the safety, efficacy, and outcome of the FTS protocol employed in the perioperative treatment of GC patients compared to that of conventional perioperative treatment. The results from our meta-analysis suggested that the FTS protocol was feasible for perioperative care of GC patients who underwent gastrectomy (distal subtotal, proximal subtotal, or radical total gastrectomy) by open surgery or laparoscopy. Compared with conventional care, FTS shortened the duration to flatus, accelerated the decrease in CRP, shortened the postoperative stay, and reduced extremely the cost of hospitalization. FTS made no significant difference in terms of operation time or intraoperative blood loss.
A major concern about FTS is a higher risk of postoperative complications. After pooling the data on complications, however, it was apparent that FTS did not increase the possibility of postoperative complications versus conventional care by the overall analysis or the analysis conducted on the open and laparoscopic surgery subgroups.
The FTS protocol comprises a new and revolutionary perioperative treatment that has become prevalent in recent years and is receiving recognition. Many FTS protocols have been suggested by hospital groups that comprise varying preoperative, intraoperative, and postoperative fast-track elements such as preoperative counseling and feeding, no bowel preparation, perioperative high oxygen concentrations, active prevention of hypothermia, and no routine use of nasogastric tubes and drains. Overall, the findings indicate that effective pain relief allows early mobilization, and the hospital stay can be reduced to 2 days without nausea, vomiting, or ileus. Postoperative fatigue and impaired functional activity can be avoided. The use of epidural local anesthetic and early oral nutrition combined with a prokinetic drug (cisapride) as well as the avoidance of opioids and gastric tubes significantly reduce the occurrence of gastrointestinal ileus [1]. The combination of these approaches could reduce the stress response and organ dysfunction, thereby greatly shortening the time required for full recovery.
Studies focused on GC patients who underwent gastrectomy with FTS treatment are limited. In the study of Feng et al. [32], FTS not only shortened the time to flatus, shortened the postoperative hospital stay, and lowered the hospitalization cost, it accelerated the decrease in the white blood cell count (p < 0.05) and alleviated pain in patients after surgery (p < 0.05 on PODs 1–3). Wang et al. [33] indicated that their FTS group showed lower serum levels of tumor necrosis factor-α (days 1 and 3) and interleukin-6 (days 1 and 3) than were seen in the conventional treatment group (all p < 0.05). In a subgroup analysis, Chen et al. [34] proved that a combination of FTS and laparoscopic surgery for GC is safe, feasible, and efficient. However, the time to first flatus in the study of Kim et al. [35] was not different between groups. Tan and his colleagues published a systematic review and meta-analysis of RCTs and CCTs that investigated the FTS strategy after gastrectomy [37]. The meta-analysis included five studies (three RCTs, two CCTs), two of which were included in the present meta-analysis. They concluded that FTS after gastrectomy reduced the time to flatus and the postoperative hospital stay. It also reduced postoperative complications. The present meta-analysis included five RCTs and one CCT. All of these studies came from Asia, which might due to the high incidence of GC in that region. Compared with the meta-analysis reported by Tan and colleagues [37], the present work included one recent large multicenter RCT published in 2013 [32], which pointed out that open surgery combined with FTS care was the optimal approach for patients undergoing radical total gastrectomy for GC.
The shortcomings of the present meta-analysis were as follows. First, one study included in this meta-analysis was not blinded, so there is a possibility of observer bias. Second, as is well known, the success of an FTS program depends on a committed, well-trained, experienced multidisciplinary team often comprised of anesthesiologists, surgeons, dieticians, physiotherapists, and a dedicated nursing staff. In our study, surgeons with varying expertise were from different clinical centers. Therefore, the operation time, intraoperative blood loss, and CRP measurements might be affected. However, intersurgeon variability is a problem encountered in most clinical trials and is difficult to avoid. Finally, although some outcome measures are not significant, it is worth mentioning that the sample size was small. Therefore, any real differences might not be apparent at present, but this factor should be considered when further trials are designed.
Conclusions
The results suggested that FTS pathways could shorten the time to flatus, accelerate the decrease in CRP, shorten the duration of postoperative stay, and reduce the cost of hospitalization gastrectomy without compromising patient safety. Thus, FTS was effective and safe—superior to conventional care in some cases—for GC patients who underwent gastrectomy (distal subtotal, proximal subtotal, and radical total gastrectomy) during and after open or laparoscopic surgery. Future studies have to define the active elements to improve future FTS protocols.
References
Bardram L, Funch-Jensen P, Jensen P et al (1995) Recovery after laparoscopic colonic surgery with epidural analgesia, and early oral nutrition and mobilisation. Lancet 345:763–764
Kehlet H, Slim K (2012) The future of fast-track surgery. Br J Surg 99:1025–1026
Slim K (2011) Fast-track surgery: the next revolution in surgical care following laparoscopy. Colorectal Dis 13:478–480
Wilmore DW, Kehlet H (2001) Management of patients in fast track surgery. BMJ 322:473–476
Wang G, Jiang Z, Zhao K et al (2012) Immunologic response after laparoscopic colon cancer operation within an enhanced recovery program. J Gastrointest Surg 16:1379–1388
Ionescu D, Iancu C, Ion D et al (2009) Implementing fast-track protocol for colorectal surgery: a prospective randomized clinical trial. World J Surg 33:2433–2438. doi:10.1007/s00268-009-0197-x
Varadhan KK, Neal KR, Dejong CH et al (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr 29:434–440
Gralla O, Haas F, Knoll N et al (2007) Fast-track surgery in laparoscopic radical prostatectomy: basic principles. World J Urol 25:185–191
Jawahar K, Scarisbrick AA (2009) Parental perceptions in pediatric cardiac fast-track surgery. AORN J 89:725–731
Husted H, Troelsen A, Otte KS et al (2011) Fast-track surgery for bilateral total knee replacement. J Bone Joint Surg Br 93:351–356
Antipin EE, Uvarov DN, Svirskii DA et al (2011) Realization of fast track surgery principles during cesarean section. Anesteziol Reanimatol 3:33–36
Liang YX, Zhou YB, Shen Y et al (2012) Whether awake coronary artery bypass grafting is contrary to fast-track surgery? Eur J Cardiothorac Surg 41:719–720
Mattioli G, Palomba L, Avanzini S et al (2009) Fast-track surgery of the colon in children. J Laparoendosc Adv Surg Tech A 19(Suppl 1):S7–S9
Day A, Fawcett WJ, Scott MJ et al (2012) Fast-track surgery and the elderly. Br J Anaesth 109:124
Parkin DM, Bray F, Ferlay J et al (2005) Global cancer statistics, 2002. CA Cancer J Clin 55:74–108
Li GC, Zhang YL, Zhang M (2008) An analysis of global cancer incidence and mortality tendency from 1999 to 2002. B Chinese Cancer 17(8):646–649
Lee SI, Choi YS, Park DJ et al (2006) Comparative study of laparoscopy-assisted distal gastrectomy and open distal gastrectomy. J Am Coll Surg 202:874–880
Rohde H, Bauer P, Stutzer H et al (1991) Proximal compared with distal adenocarcinoma of the stomach: differences and consequences—German Gastric Cancer TNM Study Group. Br J Surg 78:1242–1248
Carrere N, Seulin P, Julio CH et al (2007) Is nasogastric or nasojejunal decompression necessary after gastrectomy? A prospective randomized trial. World J Surg 31:122–127. doi:10.1007/s00268-006-0430-9
Yoo CH, Son BH, Han WK et al (2002) Nasogastric decompression is not necessary in operations for gastric cancer: prospective randomised trial. Eur J Surg 168:379–383
Kehlet H, Wilmore DW (2002) Multimodal strategies to improve surgical outcome. Am J Surg 183:630–641
Goris RJ (1996) MODS/SIRS: result of an overwhelming inflammatory response? World J Surg 20:418–421. doi:10.1007/s002689900066
Sato N, Koeda K, Ikeda K et al (2002) Randomized study of the benefits of preoperative corticosteroid administration on the postoperative morbidity and cytokine response in patients undergoing surgery for esophageal cancer. Ann Surg 236:184–190
Raeburn CD, Sheppard F, Barsness KA et al (2002) Cytokines for surgeons. Am J Surg 183:268–273
Cruickshank AM, Fraser WD, Burns HJ et al (1990) Response of serum interleukin-6 in patients undergoing elective surgery of varying severity. Clin Sci (Lond) 79:161–165
Bianchi RA, Silva NA, Natal ML et al (2004) Utility of base deficit, lactic acid, microalbuminuria, and C-reactive protein in the early detection of complications in the immediate postoperative evolution. Clin Biochem 37:404–407
Suehiro T, Matsumata T, Shikada Y et al (2004) Accelerated rehabilitation with early postoperative oral feeding following gastrectomy. Hepatogastroenterology 51:1852–1855
Petrowsky H, Demartines N, Rousson V et al (2004) Evidence-based value of prophylactic drainage in gastrointestinal surgery: a systematic review and meta-analyses. Ann Surg 240:1074–1084 discussion 1084–1085
Jadad AR, Moore RA, Carroll D et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Wang DS, Zhou YB, Kong Y et al (2009) Observation of fast track surgery in patients with gastric cancer. Zhonghua Wei Chang Wai Ke Za Zhi 12:462–466
Feng F, Ji G, Li JP et al (2013) Fast-track surgery could improve postoperative recovery in radical total gastrectomy patients. World J Gastroenterol 19:3642–3648
Wang D, Kong Y, Zhong B et al (2010) Fast-track surgery improves postoperative recovery in patients with gastric cancer: a randomized comparison with conventional postoperative care. J Gastrointest Surg 14:620–627
Chen HJ, Xin JL, Cai L et al (2012) Preliminary experience of fast-track surgery combined with laparoscopy-assisted radical distal gastrectomy for gastric cancer. J Gastrointest Surg 16:1830–1839
Kim JW, Kim WS, Cheong JH et al (2012) Safety and efficacy of fast-track surgery in laparoscopic distal gastrectomy for gastric cancer: a randomized clinical trial. World J Surg 36:2879–2887. doi:10.1007/s00268-012-1741-7
Jiang ZW, Li JS, Wang ZM et al (2007) The safety and efficiency of fast track surgery in gastric cancer patients undergoing D2 gastrectomy. Zhonghua Wai Ke Za Zhi 45:1314–1317
Tan SJ, Zhou F, Chen QY et al (2013) Systemic review of the safety and efficacy of fast-track surgery combined with laparoscopy in radical gastrectomy for gastric cancer. Zhonghua Wei Chang Wai Ke Za Zhi 16:974–980
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, Yj., Huo, Tt., Xing, J. et al. Meta-Analysis of Efficacy and Safety of Fast-Track Surgery in Gastrectomy for Gastric Cancer. World J Surg 38, 3142–3151 (2014). https://doi.org/10.1007/s00268-014-2690-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2690-0